Acemetacin.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Binding of Nonsteroidal Anti-Inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects
4132 Langmuir 2008, 24, 4132-4139 Binding of Nonsteroidal Anti-inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects Marlene Lu´cio,*,†,⊥ Frank Bringezu,‡,|,⊥ Salette Reis,† Jose´ L. F. C. Lima,† and Gerald Brezesinski§,⊥ REQUIMTE, Faculdade de Farma´cia, UniVersidade do Porto, Rua Anı´bal Cunha, 4099-030 Porto, Portugal, Institute of Medical Physics and Biophysics, UniVersity of Leipzig, Ha¨rtelstrasse 16, D-04103 Leipzig, Germany, and Max-Planck Institute of Colloids and Interfaces, Research Campus Golm, Am Mu¨hlenberg 1, D-14476 Potsdam, Germany ReceiVed NoVember 16, 2007. In Final Form: January 8, 2008 The effect of nonsteroidal anti-inflammatory drugs (NSAIDs) on the phase transition and phase properties of 1,2-dipalmitoylphosphatidylcholine (DPPC) has been investigated in both 2D (monolayers at the air/water interface) and 3D (multilayers in lipid/water dispersions) model systems. The 2D membrane models have been characterized by means of pressure-area isotherms and grazing incidence X-ray diffraction (GIXD) measurements. Differential scanning calorimetry (DSC) and simultaneous small- and wide-angle X-ray diffraction have been applied to lipid aqueous dispersions. All NSAIDs studied altered the main transition temperature of the gel to liquid-crystalline phase transition, with the arylacetic acid derivatives (acemetacin and indomethacin) showing the largest effects. A comparison of the results reveals distinct structural features of the membrane models after interaction with the NSAID. All drugs induced perturbations in the lipid liquid-crystalline phase, suggesting a major change in the hydration behavior of DPPC. Again, the largest effects on the structural parameters are found for the arylacetic acid derivatives. The results obtained in the different model systems give indications of the role of the membrane/NSAID interactions that might also be important for NSAID gastric injury. -
Download Product Insert (PDF)
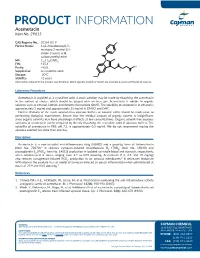
PRODUCT INFORMATION Acemetacin Item No. 29615 CAS Registry No.: 53164-05-9 Cl Formal Name: 1-(4-chlorobenzoyl)-5- methoxy-2-methyl-1H- indole-3-acetic acid, O carboxymethyl ester N MF: C21H18ClNO6 FW: 415.8 O OH Purity: ≥98% O Supplied as: A crystalline solid O Storage: -20°C O Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Acemetacin is supplied as a crystalline solid. A stock solution may be made by dissolving the acemetacin in the solvent of choice, which should be purged with an inert gas. Acemetacin is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of acemetacin in ethanol is approximately 3 mg/ml and approximately 25 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of acemetacin can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of acemetacin in PBS, pH 7.2, is approximately 0.5 mg/ml. We do not recommend storing the aqueous solution for more than one day. Description Acemetacin is a non-steroidal anti-inflammatory drug (NSAID) and a prodrug form of indomethacin 1 (Item No. 70270). It reduces zymosan-induced thromboxane B2 (TXB2; Item No. 19030) and prostaglandin E2 (PGE2; Item No. 14010) production in isolated rat whole blood and stomach, respectively, when administered at doses ranging from 2.7 to 83.8 µmol/kg. -

Inflammatory Drugs (Nsaids) for People with Or at Risk of COVID-19
Evidence review Acute use of non-steroidal anti- inflammatory drugs (NSAIDs) for people with or at risk of COVID-19 Publication date: April 2020 This evidence review sets out the best available evidence on acute use of non- steroidal anti-inflammatory drugs (NSAIDs) for people with or at risk of COVID-19. It should be read in conjunction with the evidence summary, which gives the key messages. Evidence review commissioned by NHS England Disclaimer The content of this evidence review was up-to-date on 24 March 2020. See summaries of product characteristics (SPCs), British national formulary (BNF) or the MHRA or NICE websites for up-to-date information. For details on the date the searches for evidence were conducted see the search strategy. Copyright © NICE 2020. All rights reserved. Subject to Notice of rights. ISBN: 978-1-4731-3763-9 Contents Contents ...................................................................................................... 1 Background ................................................................................................. 2 Intervention .................................................................................................. 2 Clinical problem ........................................................................................... 3 Objective ...................................................................................................... 3 Methodology ................................................................................................ 4 Summary of included studies -

Systematic Review Risk of Acute MI with Nsaids in Real
Web Appendix 1 – Systematic review Risk of acute MI with NSAIDs in real-world use: a Bayesian IPD MA Web Table 1: Search strategies for the systematic review of observational studies of NSAIDs and risk of acute MI Individual observational studies PubMed # Keywords 1 (((case-control studies [mh] OR cohort studies [mh] OR cross-over studies [mh] OR epidemiologic studies [mh:noexp] OR cross-sectional studies [mh] OR evaluation studies as topic [mh] OR meta-analysis as topic [mh] OR practice guidelines as topic [mh] OR case control [tw] OR case controlled [tw] OR case controls [tw] OR cohort [tw]OR cohorts [tw] OR follow-up [tw] OR followup [tw] OR longitudinal [tw] OR matched-pair analysis [mh] OR observational studies [tw] OR observational study [tw] OR multicenter study [pt]) AND ((comparative study [pt] OR compare [tw] OR compares [tw] OR compared [tw] OR compared [tw] OR comparing [tw] OR comparison [tw] OR comparative [tw] OR effective [tw] OR effectiveness [tw] OR versus [ti] OR vs [ti]) AND (activities of daily living [mh] OR benefit [tw] OR benefits [tw] OR budgets [mh] OR chronic disease [mh] OR clinical trials data monitoring committees [mh] OR cognitive function [tw] OR ec [sh] OR death [mh] OR diffusion of innovation [mh] OR discharge [tw] OR economics, pharmaceutical [mh] OR evidence based practice [mh] OR functional status [tw] OR guideline adherence [mh] OR harm [tw] OR harms [tw] OR health services research [mh] OR health status [mh] OR hospitalization [mh] OR interventions [tw] OR life expectancy [mh] OR longevity [mh] OR -

Prescription Medications, Drugs, Herbs & Chemicals Associated With
Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus American Tinnitus Association Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form, or by any means, without the prior written permission of the American Tinnitus Association. ©2013 American Tinnitus Association Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus American Tinnitus Association This document is to be utilized as a conversation tool with your health care provider and is by no means a “complete” listing. Anyone reading this list of ototoxic drugs is strongly advised NOT to discontinue taking any prescribed medication without first contacting the prescribing physician. Just because a drug is listed does not mean that you will automatically get tinnitus, or exacerbate exisiting tinnitus, if you take it. A few will, but many will not. Whether or not you eperience tinnitus after taking one of the listed drugs or herbals, or after being exposed to one of the listed chemicals, depends on many factors ‐ such as your own body chemistry, your sensitivity to drugs, the dose you take, or the length of time you take the drug. It is important to note that there may be drugs NOT listed here that could still cause tinnitus. Although this list is one of the most complete listings of drugs associated with tinnitus, no list of this kind can ever be totally complete – therefore use it as a guide and resource, but do not take it as the final word. The drug brand name is italicized and is followed by the generic drug name in bold. -

Pharmacokinetics of Acemetacin and Its Active Metabolite Indomethacin in Rats During Acute Hepatic Damage and Liver Regeneration
medigraphic Artemisaen línea AE Chávez-PiñaAnnals of et Hepatology al. Acemetacin 2009; pharmacokinetics 8(2): April-June: and 141-147 liver damage 141 Original Article Annals of Hepatology Pharmacokinetics of acemetacin and its active metabolite indomethacin in rats during acute hepatic damage and liver regeneration Aracely E. Chávez-Piña;1 Liliana Favari;1 Gilberto Castañeda-Hernández1 Abstract and indomethacin was comparable to control values. In conclusion: Indomethacin bioavailability after oral Background and aim: The pharmacokinetics of acem- administration of its precursor, acemetacin, is signifi- etacin, a non-steroidal anti-inflammatory drug which cantly reduced by acute hepatitis produced by CCl4. is biotransformed to indomethacin by hepatic first-pass Pharmacokinetic alterations, as liver damage, are re- effect, was examined during the necrotic and regenera- versible, but do not require complete liver regenera- tion phases resulting from acute hepatitis induced by tion to return to basal conditions. carbon tetrachloride (CCl4). Material and methods: Acute hepatitis was induced by oral CCl4 administra- Key words: Hepatitis, carbon tetrachloride, bioavail- tion to male Wistar rats. On days 0, 1 and 3 after the in- ability, first-pass effect, hepatic metabolism. sult, liver histological analysis was performed, bio- chemical markers of liver damage and regeneration Introduction were measured, and the pharmacokinetics of oral acemetacin and of its active metabolite, indomethacin, Acemetacin, a carboxymethyl ester derivative of in- were determined. Results: One day after CCl4 adminis- domethacin, is currently used in the treatment of inflam- tration, liver necrosis was apparent and there was an mation and pain.1-3 It has been shown that equimolar dos- increase in the circulating levels of indicators of liver es of both agents result in comparable analgesic and anti- damage and regeneration with regard to control condi- inflammatory effects.1,2 Notwithstanding, clinical studies tions. -

Inflammatory Drug
Abbreviations used: AR(s), adverse hepatotoxicity, 17 reaction(s); ADR(s), adverse drug manufacturers, 9 reaction(s); NSAID(s), non-steroid anti amorfazone, trade mark names and inflammatory drug(s) manufacturers, 9 Amuno, generic name and manufacturer, 12 anaemia absorption interactions, drug, 180-1 aplastic, 83 acemetacin, trade mark names and report rate, 33 manufacturers, 8 haemolytic, 84-5 acetyl salicylic acid, see Aspirin in rheumatoid patients, inappropriate action, drug, ~ pharmacoactivity therapy, 250 activation (of drugs), 243-5, 246, 247 anaphylaxis/anaphylactoid reactions, 17, pathway, 244 81 Actol, generic name and manufacturer, 13 Anaprox, generic name and manufacturer, Actosal, generic name and manufacturer, 13 9 angioedema, 6 acyl-coenzyme A formation, 221-2 angiotensin-converting enzyme, 195, 196 adjuvant induced arthritis, ~ inhibitors arthritis function, 195 Af1oxan, generic name and manufacturer, NSAID interactions with, 195-200 14 animal(s) age see also elderly experimentation, ethics of, 267 gastrointestinal susceptibility re inter species differences in lated to, 164, 286-8 propionate chiral inversion, use of anti-arthritics correlated 222-3, 223 with, 152 Ansaid, generic name and manufacturer, aged, the, ~ elderly 11 agranulocytosis antacids, 292 incidence, 7, 100-2 passim effect on drug absorption, 180, 181 in Sweden, 66, 67 NSAID interactions with, 185, 193 pyrazolone-induced, 7, 99-104 anthranilic acid, relative safety, 18 analytical epidemiological anti-arthritic drugs, ~ antirheumatic studies, 101-3 drugs -

COX-2 Selective Non-Steroidal Anti-Inflammatory Drugs For
Health Technology Assessment Health Technology Health Technology Assessment 2008; Vol. 12: No. 11 2008; 12: No. 11 Vol. selective non-steroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis COX-2 Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation Feedback The HTA Programme and the authors would like to know Y-F Chen, P Jobanputra, P Barton, S Bryan, your views about this report. The Correspondence Page on the HTA website A Fry-Smith, G Harris and RS Taylor (http://www.hta.ac.uk) is a convenient way to publish your comments. If you prefer, you can send your comments to the address below, telling us whether you would like us to transfer them to the website. We look forward to hearing from you. April 2008 The National Coordinating Centre for Health Technology Assessment, Mailpoint 728, Boldrewood, Health Technology Assessment University of Southampton, NHS R&D HTA Programme Southampton, SO16 7PX, UK. HTA Fax: +44 (0) 23 8059 5639 Email: [email protected] www.hta.ac.uk http://www.hta.ac.uk ISSN 1366-5278 HTA How to obtain copies of this and other HTA Programme reports. An electronic version of this publication, in Adobe Acrobat format, is available for downloading free of charge for personal use from the HTA website (http://www.hta.ac.uk). A fully searchable CD-ROM is also available (see below). Printed copies of HTA monographs cost £20 each (post and packing free in the UK) to both public and private sector purchasers from our Despatch Agents. -

Non-Steroidal Anti-Inflammatory Drugs and Risk of Heart Failure In
RESEARCH BMJ: first published as 10.1136/bmj.i4857 on 28 September 2016. Downloaded from OPEN ACCESS Non-steroidal anti-inflammatory drugs and risk of heart failure in four European countries: nested case-control study Andrea Arfè,1 Lorenza Scotti,1 Cristina Varas-Lorenzo,2 Federica Nicotra,1 Antonella Zambon,1 Bianca Kollhorst,3 Tania Schink,3 Edeltraut Garbe,3 Ron Herings,4 Huub Straatman,4 René Schade,5 Marco Villa,6 Silvia Lucchi,6 Vera Valkhoff,5 Silvana Romio,5 Frantz Thiessard,7 Martijn Schuemie,5 Antoine Pariente,7 Miriam Sturkenboom,5 Giovanni Corrao1 On behalf of the Safety of Non-steroidal Anti-inflammatory Drugs (SOS) Project Consortium 1Unit of Biostatistics, ABSTRACT of hospital admission for heart failure (adjusted odds Epidemiology, and Public OBJECTIVES ratio 1.19; 95% confidence interval 1.17 to 1.22), Health, Department of Statistics compared with past use of any NSAIDs (use >183 days and Quantitative Methods, To investigate the cardiovascular safety of non- University of Milano-Bicocca, steroidal anti-inflammatory drugs (NSAIDs) and in the past). Risk of admission for heart failure 20126 Milan, Italy estimate the risk of hospital admission for heart failure increased for seven traditional NSAIDs (diclofenac, 2RTI Health Solutions, with use of individual NSAIDs. ibuprofen, indomethacin, ketorolac, naproxen, Barcelona, Spain nimesulide, and piroxicam) and two COX 2 inhibitors 3 DESIGN Leibniz Institute of Prevention (etoricoxib and rofecoxib). Odds ratios ranged from Research and Epidemiology, Nested case-control study. Bremen, Germany 1.16 (95% confidence interval 1.07 to 1.27) for naproxen SETTING 4PHARMO Institute, Utrecht, to 1.83 (1.66 to 2.02) for ketorolac. -

Anti-Inflammatory/Analgesic Combination of Alpha
Patentamt JEuropàischesEuropean Patent Office ® Publication number: 0 1 09 036 Office européen des brevets g "j © EUROPEAN PATENT SPECIFICATION (45) Dateof publication of patent spécification: 02.09.87 (jjj) jnt ci 4- A 61 K 31/415, A 61 K 31/62, (22) Dateoffiling: 08.11.83 (54) Anti-inf lammatory/analgesic combination of alpha-fluoromethylhistidine and a selected non-steroidal anti-inflammatory drug (NSAID). (§) Priority: 15.11.82 US 441581 (73) Proprietor: MERCK & CO. INC. 126, East Lincoln Avenue P.O. Box 2000 Rahway New Jersey 07065 (US) (43) Date of publication of application: 23.05.84 Bulletin 84/21 @ Inventor: Goldenberg, Marvin M. 721 Shackamaxon Drive (45) Publication of the grant of the patent: Westfield New Jersey 07090 (US) 02.09.87 Bulletin 87/36 (74) Representative: Abitz, Walter, Dr.-lng. et al (84) Designated Contracting States: Abitz, Morf, Gritschneder, Freiherr von CH DE FR GB IT LI NL Wittgenstein Postfach 86 01 09 D-8000 Munchen 86 (DE) (§) References cited: EP-A-0 046290 US-A-4325 961 CÛ (£> o o> o Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted. Notice of opposition shall CL be filed in a written reasoned statement. It shall not be deemed to have been filed until the opposition fee has been LU paid. (Art. 99( 1 ) European patent convention). Courier Press, Leamington Spa, England. BACKGROUND OF THE INVENTION This invention relates to novel pharmaceutical combinations comprising a-fluoromethylhistidine (FMH) and a non-steroidal anti-inflammatory/analgesic drug (NSAID) particularly indomethacin, diflunisal and naproxen. -

Celecoxib Loaded In-Situ Provesicular Powder and Its In-Vitro
pharmaceutics Article Celecoxib Loaded In-Situ Provesicular Powder and Its In-Vitro Cytotoxic Effect for Cancer Therapy: Fabrication, Characterization, Optimization and Pharmacokinetic Evaluation Ali M. Nasr 1,2,* , Sameh S. Elhady 3 , Shady A. Swidan 4,5,* and Noha M. Badawi 4,5,* 1 Department of Pharmaceutics, Faculty of Pharmacy, Port Said University, Port Said 42526, Egypt 2 Department of Pharmaceutics, Faculty of Pharmacy, Sinai University, Alarish, North Sinai 45511, Egypt 3 Department of Natural Products and Alternative Medicine, Faculty of Pharmacy, King Abdulaziz University, Jeddah 21589, Saudi Arabia; [email protected] 4 Department of Pharmaceutics, Faculty of Pharmacy, The British University in Egypt, El-Sherouk city, Cairo 11837, Egypt 5 The Center for Drug Research and Development (CDRD), Faculty of Pharmacy, The British University in Egypt, El-Sherouk City, Cairo 11837, Egypt * Correspondence: [email protected] (A.M.N.); [email protected] (S.A.S.); [email protected] (N.M.B.) Received: 4 November 2020; Accepted: 26 November 2020; Published: 28 November 2020 Abstract: Introduction: Several recent studies have shown that the role of cyclooxygenase 2 (COX-2) in carcinogenesis has become more evident. It affects angiogenesis, apoptosis, and invasion, and plays a key role in the production of carcinogens. It has also been reported that COX-2 inhibitors such as celecoxib (CLX) might play an effective role in preventing cancer formation and progression. Formulation of CLX into nanovesicles is a promising technique to improve its bioavailability and anticancer efficacy. Aim: The aim of this study is to optimize and evaluate the anticancer efficacy of CLX-loaded in-situ provesicular powder composed of surfactants and fatty alcohol-based novel nanovesicles in-vitro and determine its pharmacokinetic parameters in-vivo. -

Nonsteroidal Anti-Inflammatory Drugs and Risk of Esophageal and Gastric Cancer
444 Cancer Epidemiology, Biomarkers & Prevention Nonsteroidal Anti-inflammatory Drugs and Risk of Esophageal and Gastric Cancer Mats Lindblad,1 Jesper Lagergren,1,2 and Luis A. Garcı´a Rodrı´guez 3 1Department of Surgical Sciences, Karolinska University Hospital and 2Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden; and 3Centro Espan˜ol de Investigacio´n Farmacoepidemiologica, Madrid, Spain Abstract Introduction: Nonsteroidal anti-inflammatory drugs (NSAID) esophageal (OR, 0.82; 95% CI, 0.57-1.18) and gastric cancer might reduce risks of esophageal and gastric cancer, but (OR, 0.65; 95% CI, 0.44-0.94), whereas long-term aspirin users previous studies are limited and provide somewhat might be at decreased risk of esophageal cancer (OR, 0.76; conflicting results. 95% CI, 0.53-1.08), but not of gastric cancer (OR, 1.09; 95% CI, Methods: We tested these associations in a prospective, 0.82-1.45). All estimates of reduced risk were weakened in nested case-control study based on the General Practitioners the 2 years lag time analysis except the association between Research Database, including over 2 million persons in the nonaspirin NSAIDs long-term users and gastric cancer. United Kingdom between 1994 and 2001. In multivariate Potentially protective effects were suggestive of being more analyses we calculated odds ratios (OR) with 95% confidence marked among subjects with a history of UGI disorders. intervals (95% CI). Data were stratified by history of upper Conclusions: Nonaspirin NSAIDs long-term use was associ- gastrointestinal (UGI) disorders and recalculated using 2 ated with a reduced risk of gastric cancer, whereas no other years lag time on data (i.e., excluding all information 2 years studied associations could be firmly established.