Methodology of a Large Prospective, Randomised, Open, Blinded
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Development and Validation of an Ultra Performance Liquid
DOI: 10.4274/tjps.76588 Turk J Pharm Sci 2017;14(1):1-8 ORIGINAL ARTICLE Development and Validation of an Ultra Performance Liquid Chromatography Method for the Determination of Dexketoprofen Trometamol, Salicylic Acid and Diclofenac Sodium Deksketoprofen Trometamol, Salisilik Asit ve Diklofenak Sodyum Etkin Maddeleri için Ultra Performanslı Sıvı Kromatografisi Yönteminin Geliştirilmesi ve Validasyonu Sibel İLBASMIŞ TAMER Gazi University, Faculty of Pharmacy, Department of Pharmaceutical Technology, Ankara, Turkey ABSTRACT Objectives: A simple, fast, accurate and precise method has been developed for the determination of dexketoprofen trometamol (DKP), salicylic acid (SA) and diclofenac sodium (DIC) in the drug solutions using ultra high performance liquid chromatography (UPLC). Materials and Methods: UPLC method is highly reliable and sensitive method to quantify the amount of the active ingredient and the method is validated according to ICH guidelines. Results: The developed method is found to be precise, accurate, specific and selective. The method was also found to be linear and reproducible. The value of limit of dedection (LOD) of DKP, SA, DIC were found 0.00325 µg/mL, 0.0027 µg/mL and 0.0304 µg/mL, respectively. The limit of quantitation (LOQ) of DKP, SA and DIC were found 0.00985 µg/mL, 0.0081 µg/mL and 0.0920 µg/mL, respectively. Conclusion: Proposed methods can be successfully applicable to the pharmaceutical preparation containing the above mentioned drugs (dexketoprofen trometamol, salicylic acid and diclofenac sodium). Even very small amounts of active substance can be analyzed and validations can be performed easily. Key words: Dexketoprofen trometamol, salicylic acid, diclofenac sodium, UPLC, validation ÖZ Amaç: Deksketoprofen trometamol (DKP), salisilik asit (SA) ve diklofenak sodyumun (DIC) ilaç çözeltisindeki analizi için ultra yüksek basınçlı sıvı kromatografisi (UPLC) kullanılarak basit, hızlı, doğru ve kesin bir yöntem geliştirilmiştir. -

Acemetacin.Pdf
Methods and Findings in Experimental and Clinical Pharmacology 2010, 32(2): ???-??? THOMSON REUTERS Copyright © 2010 Prous Science, S.A.U. or its licensors. All rights reserved. CCC: 0379-0355/2010 DOI: 10.1358/mf.2010.32.2.1423883 ORIGINAL ARTICLE ACEMETACIN ANTINOCICEPTIVE MECHANISM IS NOT RELATED TO NO OR K+ CHANNEL PATHWAYS. M. Gil-Flores1, M.I. Ortiz2, G. Castañeda-Hernández1 and A.E. Chávez-Piña1 1Departamento de Farmacología, Centro de Investigación y de Estudios Avanzados del Instituto Politécnico Nacional, México, D.F., México. 2Área Académica de Medicina del Instituto de Ciencias de la Salud, Universidad Autónoma del Estado de Hidalgo, Pachuca, Hidalgo, México SUMMARY Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) used for the treatment of acute gout and inflammation. However, its use is limited due to side effects. Acemetacin is a prodrug of indomethacin that exhibits better gastric tolerability in preclinical and clinical tri- als. The aim of this study was to examine if the systemic administration of acemetacin involved the sequential participation of nitric oxide (NO) or K+ channel pathways to confer its antinociceptive effect, as compared to indomethacin. The antinociceptive effect of both drugs was studied with the formalin test. Equimolar doses of acemetacin or indomethacin were administered orally. The intraplantar administra- tion of either L-NAME, glibenclamide, apamin or charybdotoxin plus indomethacin or acemetacin was studied using the formalin test and the anti-inflammatory and antihyperalgesic effects were measured. The antinociceptive effect of acemetacin or indomethacin was not sig- nificantly different when pretreatment with L-NAME, glibenclamide, apamin or charybdotoxin was done. The antihyperalgesic and anti- inflammatory effects were also similar for both indomethacin and acemetacin. -

Binding of Nonsteroidal Anti-Inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects
4132 Langmuir 2008, 24, 4132-4139 Binding of Nonsteroidal Anti-inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects Marlene Lu´cio,*,†,⊥ Frank Bringezu,‡,|,⊥ Salette Reis,† Jose´ L. F. C. Lima,† and Gerald Brezesinski§,⊥ REQUIMTE, Faculdade de Farma´cia, UniVersidade do Porto, Rua Anı´bal Cunha, 4099-030 Porto, Portugal, Institute of Medical Physics and Biophysics, UniVersity of Leipzig, Ha¨rtelstrasse 16, D-04103 Leipzig, Germany, and Max-Planck Institute of Colloids and Interfaces, Research Campus Golm, Am Mu¨hlenberg 1, D-14476 Potsdam, Germany ReceiVed NoVember 16, 2007. In Final Form: January 8, 2008 The effect of nonsteroidal anti-inflammatory drugs (NSAIDs) on the phase transition and phase properties of 1,2-dipalmitoylphosphatidylcholine (DPPC) has been investigated in both 2D (monolayers at the air/water interface) and 3D (multilayers in lipid/water dispersions) model systems. The 2D membrane models have been characterized by means of pressure-area isotherms and grazing incidence X-ray diffraction (GIXD) measurements. Differential scanning calorimetry (DSC) and simultaneous small- and wide-angle X-ray diffraction have been applied to lipid aqueous dispersions. All NSAIDs studied altered the main transition temperature of the gel to liquid-crystalline phase transition, with the arylacetic acid derivatives (acemetacin and indomethacin) showing the largest effects. A comparison of the results reveals distinct structural features of the membrane models after interaction with the NSAID. All drugs induced perturbations in the lipid liquid-crystalline phase, suggesting a major change in the hydration behavior of DPPC. Again, the largest effects on the structural parameters are found for the arylacetic acid derivatives. The results obtained in the different model systems give indications of the role of the membrane/NSAID interactions that might also be important for NSAID gastric injury. -

Ataxia Caused by a Single Dose of Dexketoprofen Trometamol
Acta Biomed 2014; Vol. 85, N. 3: 269-270 © Mattioli 1885 Case report Ataxia caused by a single dose of dexketoprofen trometamol Sema Avcı, Selim Genç, Macit Aydın, Fatih Büyükcam, Seda Özkan Department of Emergency Medicine, Dışkapı Yıldırım Beyazıt Training and Research Hospital, Ankara, Turkey Summary. Mushroom poisoning is an important reason of plant toxicity. Wild mushrooms that gathered from pastures and forests can be dangerous for human health. The clinical outcomes and symptoms of mushroom toxicity vary from mild gastrointestinal symptoms to acute multiple organ failure. Toxic effects to kidney and liver of amatoxin are common but cardiotoxic effects are unusual. In this case, we reported the cardiotoxic effect of amatoxin with the elevated troponin-I without any additional finding in electrocardiography, echo- cardiography and angiography Key words: cardiac enzyme, mushroom, poisoning, toxicity, troponin Introduction ture: 37.1ºC, hearth rate:75 beats/min. On physical examination, the patient was oriented, alert and con- Dexketoprofen trometamol is one of the non- scious. Neurological examination was normal except steroid anti-inflamatory drugs (NSAID) used as an- ataxia and dysarthria. She has no previous chronic dis- algesic (1). It is a water-soluable molecule and it is an eases. Laboratory results were as follows; glucose:102 active enantiomer of racemic ketoprofen (1). Peroral mg/dL, creatinine:0.61 mg/dl, alanine aminotransfer- dexketoprofen has considerable analgesic potency and ase (ALT): 8 U/L , aspartate aminotransferase (AST): well-tolerated adverse effects in patients who suffer 12 U/L, calcium:9.7 mg/dL, sodium:143 mEq/L, from acute and chronic pain (1). -

Nsaids: Dare to Compare 1997
NSAIDs TheRxFiles DARE TO COMPARE Produced by the Community Drug Utilization Program, a Saskatoon District Health/St. Paul's Hospital program July 1997 funded by Saskatchewan Health. For more information check v our website www.sdh.sk.ca/RxFiles or, contact Loren Regier C/O Pharmacy Department, Saskatoon City Hospital, 701 Queen St. Saskatoon, SK S7K 0M7, Ph (306)655-8506, Fax (306)655-8804; Email [email protected] We have come a long way from the days of willow Highlights bark. Today salicylates and non-steroidal anti- • All NSAIDs have similar efficacy and side inflammatory drugs (NSAIDs) comprise one of the effect profiles largest and most commonly prescribed groups of • In low risk patients, Ibuprofen and naproxen drugs worldwide.1 In Saskatchewan, over 20 may be first choice agents because they are different agents are available, accounting for more effective, well tolerated and inexpensive than 300,000 prescriptions and over $7 million in • Acetaminophen is the recommended first line sales each year (Saskatchewan Health-Drug Plan agent for osteoarthritis data 1996). Despite the wide selection, NSAIDs • are more alike than different. Although they do Misoprostol is the only approved agent for differ in chemical structure, pharmacokinetics, and prophylaxis of NSAID-induced ulcers and is to some degree pharmacodynamics, they share recommended in high risk patients if NSAIDS similar mechanisms of action, efficacy, and adverse cannot be avoided. effects. week or more to become established. For this EFFICACY reason, an adequate trial of 1-2 weeks should be NSAIDs work by inhibiting cyclooxygenase (COX) allowed before increasing the dose or changing to and subsequent prostaglandin synthesis as well as another NSAID. -
Download Product Insert (PDF)
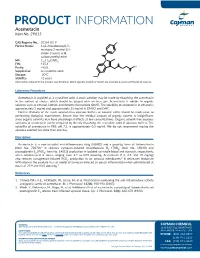
PRODUCT INFORMATION Acemetacin Item No. 29615 CAS Registry No.: 53164-05-9 Cl Formal Name: 1-(4-chlorobenzoyl)-5- methoxy-2-methyl-1H- indole-3-acetic acid, O carboxymethyl ester N MF: C21H18ClNO6 FW: 415.8 O OH Purity: ≥98% O Supplied as: A crystalline solid O Storage: -20°C O Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Acemetacin is supplied as a crystalline solid. A stock solution may be made by dissolving the acemetacin in the solvent of choice, which should be purged with an inert gas. Acemetacin is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of acemetacin in ethanol is approximately 3 mg/ml and approximately 25 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of acemetacin can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of acemetacin in PBS, pH 7.2, is approximately 0.5 mg/ml. We do not recommend storing the aqueous solution for more than one day. Description Acemetacin is a non-steroidal anti-inflammatory drug (NSAID) and a prodrug form of indomethacin 1 (Item No. 70270). It reduces zymosan-induced thromboxane B2 (TXB2; Item No. 19030) and prostaglandin E2 (PGE2; Item No. 14010) production in isolated rat whole blood and stomach, respectively, when administered at doses ranging from 2.7 to 83.8 µmol/kg. -

A Combined Crystallographic and Computational Study on Dexketoprofen Trometamol Dihydrate Salt
crystals Article A Combined Crystallographic and Computational Study on Dexketoprofen Trometamol Dihydrate Salt Patrizia Rossi 1 , Paola Paoli 1,* , Stella Milazzo 1, Laura Chelazzi 2 , Maria Paola Giovannoni 3, Gabriella Guerrini 3 , Andrea Ienco 4,* , Maurizio Valleri 5 and Luca Conti 6 1 Department of Industrial Engineering, University of Florence, via Santa Marta 3, 50139 Florence, Italy; p.rossi@unifi.it (P.R.); stella.milazzo@unifi.it (S.M.) 2 Centro di Cristallografia Strutturale, University of Florence, via della Lastruccia 3, Sesto F.no, 50019 Florence, Italy; laura.chelazzi@unifi.it 3 NEUROFARBA, Sezione Farmaceutica e Nutraceutica, University of Florence, Via Ugo Schiff 6, Sesto F.no, 50019 Florence, Italy; mariapaola.giovannoni@unifi.it (M.P.G.); gabriella.guerrini@unifi.it (G.G.) 4 CNR-ICCOM, via Madonna del Piano 10, Sesto F.no, 50019 Florence, Italy 5 A. Menarini Manufacturing Logistics and Services s.r.l., via R. Pilo 4, 50131 Florence, Italy; [email protected] 6 Department of Chemistry “U. Schiff”, University of Florence, via della Lastruccia 3, Sesto F.no, 50019 Florence, Italy; luca.conti@unifi.it * Correspondence: paola.paoli@unifi.it (P.P.); [email protected] (A.I.) Received: 29 June 2020; Accepted: 30 July 2020; Published: 31 July 2020 Abstract: Dexketoprofen trometamol is the tromethamine salt of dexketoprofen [(2S)-2-(3-benzoylphenyl) propanoic acid-2-amino-2-(hydroxymethyl)propane-1,3-diol], a nonsteroidal anti-inflammatory drug (NSAID) used for the treatment of moderate- to strong-intensity acute pain. The crystal structure of the hitherto sole known hydrate phase of dexketoprofen trometamol (DK-T_2H2O), as determined by single-crystal X-ray diffraction, is presented. -

Product Monograph
PRODUCT MONOGRAPH NOVO–KETOROLAC (ketorolac tromethamine) 10 mg Tablets NSAID Analgesic Agent Novopharm Limited Date of Revision: Toronto, Canada August 02, 2007 Control Number 112565 PRODUCT MONOGRAPH NOVO–KETOROLAC (ketorolac tromethamine) 10 mg Tablets THERAPEUTIC CLASSIFICATION NSAID Analgesic Agent ACTION AND CLINICAL PHARMACOLOGY NOVO-KETOROLAC (ketorolac tromethamine) is a non-steroidal anti-inflammatory drug (NSAID) that has analgesic activity. It is considered to be a peripherally acting analgesic. It is thought to inhibit the cyclo-oxygenase enzyme system, thereby inhibiting the synthesis of prostaglandins. At analgesic doses it has minimal anti-inflammatory and antipyretic activity. The peak analgesic effect occurs at 2 to 3 hours post-dosing with no evidence of a statistically significant difference over the recommended dosage range. The greatest difference between large and small doses of administered ketorolac is in the duration of analgesia. Following oral administration, ketorolac tromethamine is rapidly and completely absorbed, and pharmacokinetics are linear following single and multiple dosing. Steady state plasma levels are achieved after one day of q.i.d. dosing. - 2 - Peak plasma concentrations of 0.7 to 1.1 µg/mL occurred at 44 minutes following a single oral dose of 10 mg. The terminal plasma elimination half-life ranged between 2.4 and 9 hours in healthy adults, while in the elderly subjects (mean age: 72 years) it ranged between 4.3 and 7.6 hours. A high fat meal decreased the rate but not the extent of absorption of oral ketorolac tromethamine, while antacid had no effect. In renally impaired patients there is a reduction in clearance and an increase in the terminal half- life of ketorolac tromethamine (See Table 1). -

Of 20 PRODUCT MONOGRAPH FLURBIPROFEN Flurbiprofen Tablets BP 50 Mg and 100 Mg Anti-Inflammatory, Analgesic Agent AA PHARM
PRODUCT MONOGRAPH FLURBIPROFEN Flurbiprofen Tablets BP 50 mg and 100 mg Anti-inflammatory, analgesic agent AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road, Unit #1 April 16, 1991 Vaughan, Ontario L4K 4N7 DATE OF REVISION: February 7, 2019 Submission Control No. 223098 Page 1 of 20 PRODUCT MONOGRAPH NAME OF DRUG FLURBIPROFEN Flurbiprofen Tablets BP 50 mg and 100 mg PHARMACOLOGICAL CLASSIFICATION Anti-inflammatory, analgesic agent ACTIONS AND CLINICAL PHARMACOLOGY FLURBIPROFEN (flurbiprofen), a phenylalkanoic acid derivative, is a non-steroidal anti- inflammatory agent which also possesses analgesic and antipyretic activities. Its mode of action, like that of other non-steroidal anti-inflammatory agents, is not known. However, its therapeutic action is not due to pituitary adrenal stimulation. Flurbiprofen is an inhibitor of prostaglandin synthesis. The resulting decrease in prostaglandin synthesis may partially explain the drug's anti-inflammatory effect at the cellular level. Pharmacokinetics: Flurbiprofen is well absorbed after oral administration, reaching peak blood levels in approximately 1.5 hours (range 0.5 to 4 hours). Administration of flurbiprofen with food does not alter total drug availability but delays absorption. Excretion of flurbiprofen is virtually complete 24 hours after the last dose. The elimination half-life is 5.7 hours with 90% of the half-life values from 3-9 hours. There is no evidence of drug accumulation and flurbiprofen does not induce enzymes that alter its metabolism. Flurbiprofen is rapidly metabolized and excreted in the urine as free and unaltered intact drug (20-25%) and hydroxylated metabolites (60-80%). In animal models of inflammation the metabolites showed no activity. -

Package Leaflet: Information for the Patient Dexketoprofen Rowex 25 Mg Film-Coated Tablets Dexketoprofen
Package leaflet: Information for the patient Dexketoprofen Rowex 25 mg Film-coated tablets Dexketoprofen Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor or pharmacist. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Dexketoprofen Rowex is and what it is used for 2. What you need to know before you take Dexketoprofen Rowex 3. How to take Dexketoprofen Rowex 4. Possible side effects 5. How to store Dexketoprofen Rowex 6. Contents of the pack and other information 1. What Dexketoprofen Rowex is and what it is used for Dexketoprofen Rowex is a pain killer from the group of medicines called non-steroidal anti- inflammatory drugs (NSAIDs). It is used to treat mild to moderate pain, such as muscular pain, painful periods (dysmenorrhoea), toothache. 2. What you need to know before you take Dexketoprofen Rowex Do not take Dexketoprofen Rowex if you are allergic to dexketoprofen or any of the other ingredients of this medicine (listed in section 6). are allergic to acetylsalicylic acid or to other non-steroidal anti-inflammatory medicines. have asthma or have suffered attacks of asthma, acute allergic rhinitis (a short period of inflamed lining of the nose), nasal polyps (lumps within the nose due to allergy), urticaria (skin rash), angioedema (swollen face, eyes, lips, or tongue, or respiratory distress) or wheezing in the chest after taking acetylsalicylic acid or other non-steroidal anti-inflammatory medicines. -

Patient Information Leaflet: Information for the User <Invented Name> 30
Patient Information Leaflet: Information for the user <Invented name> 30 mg/ml solution for injection ketorolac trometamol Read all of this leaflet carefully before you start using this medicine because it contains important information for you. • Keep this leaflet. You may need to read it again. • If you have any further questions, ask your doctor or nurse. • If you get any side effects, talk to your doctor or nurse. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What <Invented name> is and what it is used for 2. What you need to know before you are given <Invented name> 3. How <Invented name> is given 4. Possible side effects 5. How to store <Invented name> 6. Contents of the pack and other information 1. What <Invented name> is and what it is used for <Invented name> contains an active substance called ketorolac trometamol and belongs to a group of medicines called non-steroidal anti-inflammatory drugs (NSAIDs). Ketorolac is used in hospital, for short-term relief of moderate to severe pain after operations and in the case of acute kidney stone pain, in adults and adolescents ≥16 years. 2. What you need to know before you are given <Invented name> <Invented name> should not be used before or during surgery due to increased risk of bleeding. <Invented name> must not be given by epidural or intrathecal administration . Severe anaphylactic-like reactions have been observed in patients with a history of allergic reactions (symptoms of asthma, inflammation of the nasal mucosa or skin reactions) to the use of acetylsalicylic acid (e.g. -

50 Mg/2Ml Solution for Injection/Infusion
SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT <Product name> 50 mg/2ml solution for injection/infusion 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 1 ml of solution contains dexketoprofen trometamol corresponding to 25 mg of dexketoprofen. One ampoule (2 ml) contains dexketoprofen trometamol corresponding to 50 mg of dexketoprofen. Excipients with known effect: 200 mg ethanol (96 %) and 8.0 mg sodium chloride. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection/infusion. Clear colourless solution, free from visible particles. pH 7.0-8.0 Osmolarity 270-328 mOsmol/l 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Symptomatic treatment of acute pain of moderate to severe intensity, when oral administration is not appropriate such as post-operative pain, renal colic and low back pain. 4.2 Posology and method of administration Posology Adults The recommended dose is 50 mg every 8 – 12 hours. If necessary, the administration can be repeated 6 hours apart. The total daily dose should not exceed 150 mg. <Product name> is intended for short term use and the treatment must be limited to the acute symptomatic period (no more than two days). Patients should be switched to an oral analgesic treatment when possible. Undesirable effects may be minimised by using the lowest effective dose for the shortest duration necessary to control symptoms (see section 4.4). In case of moderate to severe postoperative pain, <Product name> can be used in combination with opioid analgesics, if indicated, at the same recommended doses in adults (see section 5.1). Pediatric population <Product name> has not been studied in children and adolescents.