Celecoxib Loaded In-Situ Provesicular Powder and Its In-Vitro
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Catalyst in Basic Oleochemicals
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Diponegoro University Institutional Repository Bulletin of Chemical Reaction Engineering & Catalysis, 2(2-3), 2007, 22-31 Catalyst in Basic Oleochemicals Eva Suyenty, Herlina Sentosa, Mariani Agustine, Sandy Anwar, Abun Lie, and Erwin Sutanto * Research and Development Department, PT. Ecogreen Oleochemicals Jln. Pelabuhan Kav 1, Kabil, Batam 29435, Telp/Fax: (0778)711374 Presented at Symposium and Congress of MKICS 2007, 18-19 April 2007, Semarang, Indonesia Abstract Currently Indonesia is the world largest palm oil producer with production volume reaching 16 million tones per annum. The high crude oil and ethylene prices in the last 3 – 4 years contribute to the healthy demand growth for basic oleochemicals: fatty acids and fatty alcohols. Oleochemicals are starting to replace crude oil derived products in various applications. As widely practiced in petrochemical industry, catalyst plays a very important role in the production of basic oleochemicals. Catalytic reactions are abound in the production of oleochemicals: Nickel based catalysts are used in the hydrogenation of unsaturated fatty ac- ids; sodium methylate catalyst in the transesterification of triglycerides; sulfonic based polystyrene resin catalyst in esterification of fatty acids; and copper chromite/copper zinc catalyst in the high pressure hydro- genation of methyl esters or fatty acids to produce fatty alcohols. To maintain long catalyst life, it is crucial to ensure the absence of catalyst poisons and inhibitors in the feed. The preparation methods of nickel and copper chromite catalysts are as follows: precipitation, filtration, drying, and calcinations. Sodium methy- late is derived from direct reaction of sodium metal and methanol under inert gas. -

Study of Fatty Acid and Fatty Alcohol Formation from Hydrolysis of Rice Bran Wax Kelly L
1747 A publication of CHEMICAL ENGINEERING TRANSACTIONS The Italian Association VOL. 32, 2013 of Chemical Engineering Online at: www.aidic.it/cet Chief Editors: Sauro Pierucci, Jiří J. Klemeš Copyright © 2013, AIDIC Servizi S.r.l., ISBN 978-88-95608-23-5; ISSN 1974-9791 Study of Fatty Acid and Fatty Alcohol Formation from Hydrolysis of Rice Bran Wax Kelly L. Tronia, Simone M. Silvab, Antonio J.A. Meirellesb, Roberta Ceriani*a a Faculty of Chemical Engineering, University of Campinas (UNICAMP), Zip Code, 13083-852, Campinas, São Paulo, Brazil b Faculty of Food Engineering, University of Campinas (UNICAMP), Zip Code, 13083-862, Campinas, São Paulo, Brazil [email protected] Rice bran wax is waste material of dewaxing process in oil refining. Dewaxing is accomplished by cooling and filtrating for separating wax from the oil to avoid turbidity in the final product. The dewaxing residue may have 20 up to 80 wt% of oil, followed by a main fraction of waxes, free fatty alcohols, free fatty acids and hydrocarbons. The wax fraction of the residue is composed by long-chain fatty alcohols esterified with long-chain fatty acids. Considering that rice bran oil has 4 – 6 wt% of wax, a large amount of this natural source of fatty compounds is undervalued. Noweck and Rider (1987) describe a process based on hydrolysis of waxes with sodium hydroxide, followed by distillation of fatty alcohols and soap. According to best of our knowledge no work has been reported on the formation of fatty acids and alcohols from the hydrolysis of the dewaxing residue using supersaturated stripping steam under high temperatures and high vacuum. -

( 12 ) United States Patent ( 10 ) Patent No .: US 10,751,310 B2 Freeman Et Al
US010751310B2 ( 12 ) United States Patent ( 10 ) Patent No .: US 10,751,310 B2 Freeman et al . ( 45 ) Date of Patent : Aug. 25 , 2020 ( 54 ) PREVENTION , TREATMENT AND ( 56 ) References Cited REVERSAL OF DISEASE USING THERAPEUTICALLY EFFECTIVE U.S. PATENT DOCUMENTS AMOUNTS OF DICARBOXYLIC ACID 3,527,789 A 9/1970 Payne COMPOUNDS 4,166,913 A 9/1979 Kesling , Jr. et al . 6,528,499 B1 * 3/2003 Kozikowski C07C 59/347 ( 71 ) Applicant: UNIVERSITY OF 514/574 8,324,277 B2 12/2012 Freeman PITTSBURGH — OF THE 8,735,449 B2 5/2014 Freeman COMMONWEALTH SYSTEM OF 9,066,902 B2 6/2015 Freeman et al . HIGHER EDUCATION , Pittsburgh , 9,186,408 B2 11/2015 Freeman et al . PA (US ) 9,700,534 B2 7/2017 Freeman et al . 9,750,725 B2 9/2017 Freeman et al . 10,213,417 B2 2/2019 Freeman et al . ( 72 ) Inventors : Bruce A. Freeman , Pittsburgh , PA 10,258,589 B2 4/2019 Freeman et al . ( US ) ; Francisco J. Schopfer , 2015/0018417 Al 1/2015 Freeman et al . Pittsburgh , PA ( US ) FOREIGN PATENT DOCUMENTS ( 73 ) Assignee : University of Pittsburgh — of the CN 103705499 4/2014 Commonwealth System of Higher DE 102011118462 5/2013 Education , Pittsburgh , PA ( US ) GB 1153464 5/1969 WO WO 2002/022627 3/2002 WO WO 2009/017802 2/2009 ( * ) Notice : Subject to any disclaimer , the term of this WO WO 2009/112455 9/2009 patent is extended or adjusted under 35 WO WO 2010/005521 1/2010 U.S.C. 154 ( b ) by 0 days . WO WO 2010/014889 2/2010 WO WO 2011/014261 2/2011 WO WO 2013/116753 8/2013 ( 21 ) Appl. -

Acemetacin.Pdf
Methods and Findings in Experimental and Clinical Pharmacology 2010, 32(2): ???-??? THOMSON REUTERS Copyright © 2010 Prous Science, S.A.U. or its licensors. All rights reserved. CCC: 0379-0355/2010 DOI: 10.1358/mf.2010.32.2.1423883 ORIGINAL ARTICLE ACEMETACIN ANTINOCICEPTIVE MECHANISM IS NOT RELATED TO NO OR K+ CHANNEL PATHWAYS. M. Gil-Flores1, M.I. Ortiz2, G. Castañeda-Hernández1 and A.E. Chávez-Piña1 1Departamento de Farmacología, Centro de Investigación y de Estudios Avanzados del Instituto Politécnico Nacional, México, D.F., México. 2Área Académica de Medicina del Instituto de Ciencias de la Salud, Universidad Autónoma del Estado de Hidalgo, Pachuca, Hidalgo, México SUMMARY Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) used for the treatment of acute gout and inflammation. However, its use is limited due to side effects. Acemetacin is a prodrug of indomethacin that exhibits better gastric tolerability in preclinical and clinical tri- als. The aim of this study was to examine if the systemic administration of acemetacin involved the sequential participation of nitric oxide (NO) or K+ channel pathways to confer its antinociceptive effect, as compared to indomethacin. The antinociceptive effect of both drugs was studied with the formalin test. Equimolar doses of acemetacin or indomethacin were administered orally. The intraplantar administra- tion of either L-NAME, glibenclamide, apamin or charybdotoxin plus indomethacin or acemetacin was studied using the formalin test and the anti-inflammatory and antihyperalgesic effects were measured. The antinociceptive effect of acemetacin or indomethacin was not sig- nificantly different when pretreatment with L-NAME, glibenclamide, apamin or charybdotoxin was done. The antihyperalgesic and anti- inflammatory effects were also similar for both indomethacin and acemetacin. -

Binding of Nonsteroidal Anti-Inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects
4132 Langmuir 2008, 24, 4132-4139 Binding of Nonsteroidal Anti-inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects Marlene Lu´cio,*,†,⊥ Frank Bringezu,‡,|,⊥ Salette Reis,† Jose´ L. F. C. Lima,† and Gerald Brezesinski§,⊥ REQUIMTE, Faculdade de Farma´cia, UniVersidade do Porto, Rua Anı´bal Cunha, 4099-030 Porto, Portugal, Institute of Medical Physics and Biophysics, UniVersity of Leipzig, Ha¨rtelstrasse 16, D-04103 Leipzig, Germany, and Max-Planck Institute of Colloids and Interfaces, Research Campus Golm, Am Mu¨hlenberg 1, D-14476 Potsdam, Germany ReceiVed NoVember 16, 2007. In Final Form: January 8, 2008 The effect of nonsteroidal anti-inflammatory drugs (NSAIDs) on the phase transition and phase properties of 1,2-dipalmitoylphosphatidylcholine (DPPC) has been investigated in both 2D (monolayers at the air/water interface) and 3D (multilayers in lipid/water dispersions) model systems. The 2D membrane models have been characterized by means of pressure-area isotherms and grazing incidence X-ray diffraction (GIXD) measurements. Differential scanning calorimetry (DSC) and simultaneous small- and wide-angle X-ray diffraction have been applied to lipid aqueous dispersions. All NSAIDs studied altered the main transition temperature of the gel to liquid-crystalline phase transition, with the arylacetic acid derivatives (acemetacin and indomethacin) showing the largest effects. A comparison of the results reveals distinct structural features of the membrane models after interaction with the NSAID. All drugs induced perturbations in the lipid liquid-crystalline phase, suggesting a major change in the hydration behavior of DPPC. Again, the largest effects on the structural parameters are found for the arylacetic acid derivatives. The results obtained in the different model systems give indications of the role of the membrane/NSAID interactions that might also be important for NSAID gastric injury. -
Download Product Insert (PDF)
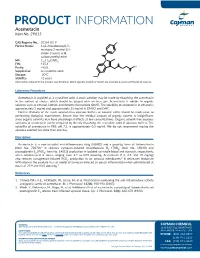
PRODUCT INFORMATION Acemetacin Item No. 29615 CAS Registry No.: 53164-05-9 Cl Formal Name: 1-(4-chlorobenzoyl)-5- methoxy-2-methyl-1H- indole-3-acetic acid, O carboxymethyl ester N MF: C21H18ClNO6 FW: 415.8 O OH Purity: ≥98% O Supplied as: A crystalline solid O Storage: -20°C O Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Acemetacin is supplied as a crystalline solid. A stock solution may be made by dissolving the acemetacin in the solvent of choice, which should be purged with an inert gas. Acemetacin is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of acemetacin in ethanol is approximately 3 mg/ml and approximately 25 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of acemetacin can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of acemetacin in PBS, pH 7.2, is approximately 0.5 mg/ml. We do not recommend storing the aqueous solution for more than one day. Description Acemetacin is a non-steroidal anti-inflammatory drug (NSAID) and a prodrug form of indomethacin 1 (Item No. 70270). It reduces zymosan-induced thromboxane B2 (TXB2; Item No. 19030) and prostaglandin E2 (PGE2; Item No. 14010) production in isolated rat whole blood and stomach, respectively, when administered at doses ranging from 2.7 to 83.8 µmol/kg. -

(ATRA) with Arsenic Trioxide (ATO) Induction Therapy
NCCP Chemotherapy Regimen Tretinoin (ATRA) with Arsenic Trioxide (ATO) Induction Therapy INDICATIONS FOR USE: Regimen *Reimbursement INDICATION ICD10 Code Status Treatment of patients with newly diagnosed low to intermediate C92 00356a Hospital risk Acute Promyelocytic Leukaemia (APL) *If the reimbursement status is not defined i, the indication has yet to be assessed through the formal HSE reimbursement process. TREATMENT: The starting dose of the drugs detailed below may be adjusted downward by the prescribing clinician, using their independent medical judgement, to consider each patients individual clinical circumstances. The treatment is administered until haematological complete remission (CR) or for a maximum of 60 days. Patients who achieve haematological CR progress to Consolidation Therapy with all trans retinoic acid (ATRA) and Arsenic Trioxide (Reference NCCP Regimen 00357). CR is defined as where the bone marrow is regenerating normal haematopoietic cells and contains <5% blast cells by morphology in an aspirate sample with at least 200 nucleated cells. Day Drug Dose Route Cycle 1 until complete Tretinoin 45mg/m2 in aPO n/a Continuous until remission (ATRA) divided doses Complete Remission (CR) is achieved or up to a maximum of 60 days 1-5 inclusive Arsenic 0.3mg/kg IV 250ml of 0.9% NaCl over Week 1 only trioxide infusion 2 hoursb Twice weekly Arsenic 0.25mg/kg IV 250ml of 0.9% NaCl over Week 2 to 8 trioxide infusion 2 hoursb 1 until end of Prednisolone 0.5mg/kg/day PO induction a Tretinoin (ATRA) is available as 10mg capsules. Round dose to nearest 10mg. The capsules should be swallowed whole with water. -

Predicting Distribution of Ethoxylation Homologues With
1 PREDICTING THE DISTRIBUTION OF ETHOXYLATION HOMOLOGUES WITH A PROCESS SIMULATOR Nathan Massey, Chemstations, Inc. Introduction Ethoxylates are generally obtained by additions of ethylene oxide (EO) to compounds containing dissociated protons. Substrates used for ethoxylation are primarily linear and branched C12-C18 alcohols, alkyl phenols, nonyl (propylene trimer) or decyl (propylene tetramer) groups, fatty acids and fatty acid derivatives. The addition of EO to a substrate containing acidic hydrogen is catalyzed by bases or Lewis acids. Amphoteric catalysts, as well as heterogeneous catalysts are also used. The degree of ethoxylation ( the moles of EO added per mole of substrate ) varies over wide ranges, in general between 3 and 40, and is chosen according to the intended use. As an illustration of how this distribution might be predicted using a process simulator, Chemcad was used to simulate the ethoxylation of Nonylphenols. Description of the Ethoxylation Chemistry The reaction mechanisms of base catalyzed and acid catalyzed ethoxylation differ, which affects the composition of the reaction products. In base catalyzed ethoxylation an alcoholate anion, formed initially by reaction with the catalyst ( alkali metal, alkali metal oxide, carbonate, hydroxide, or alkoxide ) nucleophilically attacks EO. The resulting union of the EO addition product can undergo an equilibrium reaction with the alcohol starting material or ethoxylated product, or can react further with EO: Figure 1 O RO- + H2CCH2 - - RO CH2CH2O O ROH H2CCH2 - - RO RO CH2CH2OH RO RO CH2CH2O 2 As Figure 1 illustrates, in alkaline catalyzed ethoxylations several reactions proceed in parallel. The addition of EO to an anion with the formation of an ether bond is irreversible. -

Acitretin; Adapalene; Alitretinoin; Bexarotene; Isotretinoin
8 February 2018 EMA/254364/2018 Pharmacovigilance Risk Assessment Committee (PRAC) Assessment report Referral under Article 31 of Directive 2001/83/EC resulting from pharmacovigilance data Retinoids containing medicinal products INN: Acitretin, Adapalene, Alitretinoin, Bexarotene, Isotretinoin, Tretinoin, Tazarotene Procedure number: EMEA/H/A-31/1446 Panretin EMEA/H/A-31/1446/C/000279/0037 Targretin EMEA/H/A-31/1446/C/000326/0043 Note: Assessment report as adopted by the PRAC and considered by the CHMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2018. Reproduction is authorised provided the source is acknowledged. Table of contents Table of contents ......................................................................................... 2 1. Information on the procedure ................................................................. 3 2. Scientific discussion ................................................................................ 3 2.1. Introduction......................................................................................................... 3 2.2. Clinical aspects .................................................................................................... 5 2.3. Data on efficacy .................................................................................................. -

Aetna Formulary Exclusions Drug List
Covered and non-covered drugs Drugs not covered – and their covered alternatives 2020 Advanced Control Plan – Aetna Formulary Exclusions Drug List 05.03.525.1B (7/20) Below is a list of medications that will not be covered without a Key prior authorization for medical necessity. If you continue using one of these drugs without prior approval, you may be required UPPERCASE Brand-name medicine to pay the full cost. Ask your doctor to choose one of the generic lowercase italics Generic medicine or brand formulary options listed below. Preferred Options For Excluded Medications1 Excluded drug name(s) Preferred option(s) ABILIFY aripiprazole, clozapine, olanzapine, quetiapine, quetiapine ext-rel, risperidone, ziprasidone, VRAYLAR ABSORICA isotretinoin ACANYA adapalene, benzoyl peroxide, clindamycin gel (except NDC^ 68682046275), clindamycin solution, clindamycin-benzoyl peroxide, erythromycin solution, erythromycin-benzoyl peroxide, tretinoin, EPIDUO, ONEXTON, TAZORAC ACIPHEX, esomeprazole, lansoprazole, omeprazole, pantoprazole, DEXILANT ACIPHEX SPRINKLE ACTICLATE doxycycline hyclate capsule, doxycycline hyclate tablet (except doxycycline hyclate tablet 50 mg [NDC^ 72143021160 only], 75 mg, 150 mg), minocycline, tetracycline ACTOS pioglitazone ACUVAIL bromfenac, diclofenac, ketorolac, PROLENSA acyclovir cream acyclovir (except acyclovir cream), valacyclovir ADCIRCA sildenafil, tadalafil ADZENYS XR-ODT amphetamine-dextroamphetamine mixed salts ext-rel†, dexmethylphenidate ext-rel, dextroamphetamine ext-rel, methylphenidate ext-rel†, MYDAYIS, -

Acitretin; Adapalene; Alitretinoin; Bexarotene; Isotretinoin
21 June 2018 EMA/261767/2018 Updated measures for pregnancy prevention during retinoid use Warning on possible risk of neuropsychiatric disorders also to be included for oral retinoids On 22 March 2018, the European Medicines Agency (EMA) completed its review of retinoid medicines, and confirmed that an update of measures for pregnancy prevention is needed. In addition, a warning on the possibility that neuropsychiatric disorders (such as depression, anxiety and mood changes) may occur will be included in the prescribing information for oral retinoids (those taken by mouth). Retinoids include the active substances acitretin, adapalene, alitretinoin, bexarotene, isotretinoin, tazarotene and tretinoin. They are taken by mouth or applied as creams or gels to treat several conditions mainly affecting the skin, including severe acne and psoriasis. Some retinoids are also used to treat certain forms of cancer. The review confirmed that oral retinoids can harm the unborn child and must not be used during pregnancy. In addition, the oral retinoids acitretin, alitretinoin and isotretinoin, which are used to treat conditions mainly affecting the skin, must be used in accordance with the conditions of a new pregnancy prevention programme by women able to have children. Topical retinoids (those applied to the skin) must also not be used during pregnancy, and by women planning to have a baby. More information is available below. Regarding the risk of neuropsychiatric disorders, the limitations of the available data did not allow to clearly establish whether this risk was due to the use of retinoids. However, considering that patients with severe skin conditions may be more vulnerable to neuropsychiatric disorders due to the nature of the disease, the prescribing information for oral retinoids will be updated to include a warning about this possible risk. -

Unusual Aldehyde Reductase Activity for Production of Full-Length Fatty Alcohol by Cyanobacterial Aldehyde Deformylating Oxygenase
Unusual Aldehyde Reductase Activity for Production of Full-length Fatty Alcohol by Cyanobacterial Aldehyde Deformylating Oxygenase Supacha Buttranon Vidyasirimedhi Institute of Science and Technology Pattarawan Intasian Vidyasirimedhi Institute of Science and Technology Nidar Treesukkasem Vidyasirimedhi Institute of Science and Technology Juthamas Jaroensuk Vidyasirimedhi Institute of Science and Technology Somchart Maenpuen Burapha university Jeerus Sucharitakul Chulalongkorn University Faculty Of Dentistry Narin Lawan Chiang Mai University Faculty of Science Pimchai Chaiyen Vidyasirimedhi Institute of Science and Technology Thanyaporn Wongnate ( [email protected] ) School of Biomolecular Science and Engineering, Vidyasirimedhi Institute of Science and Technology (VISTEC), 555 Wangchan Valley, Rayong 21210, Thailand https://orcid.org/0000-0001-5072-9738 Research Keywords: Non-heme diiron enzyme, Aldehyde-deformylating oxygenase, NADPH-dependent fatty aldehyde reductase, Fatty alcohol, Oxido-reductase Posted Date: November 5th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-100741/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/28 Abstract Background: Aldehyde-deformylating oxygenase (ADO) is a non-heme di-iron enzyme that catalyzes deformylation of aldehydes to generate alkanes/alkenes. In this study, we report for the rst time that under anaerobic or limited oxygen conditions, Prochlorococcus marinus (PmADO) can generate full- length fatty alcohols from fatty aldehydes without eliminating a carbon unit. Results: Unlike the native activity of ADO which requires electrons from the Fd/FNR electron transfer complex, the aldehyde reduction activity of ADO requires only NADPH. Our results demonstrated that yield of alcohol products can be affected by oxygen concentration and type of aldehyde.