Use of Sodium Glycerophosphate in Neonatal Parenteral Nutrition Solutions to Increase Calcium and Phosphate Compatibility for Pr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Brochure-Product-Range.Pdf
PRODUCT RANGE 2015 edition ANSI Standard 60 NSF® CERTIFIED HALAL M ISLAMIC FOOD AND NUTRITION ® COUNCIL OF AMERICA Rue Joseph Wauters, 144 ISO 9001:2008 (Quality) / OHSAS 18001:2007 (Health/ B-4480 Engis Safety) / ISO 14001:2004 (Environment) / ISO 22000:2005 www.globulebleu.com (Food Safety) / FSSC 22000:2013 (Food Safety). Tel. +32 (0) 4 273 93 58 Our food grade phosphates are allergen free, GMO free, Fax. +32 (0) 4 275 68 36 BSE/TSE free. www.prayon.com mail. [email protected] Design by www.prayon.com PRODUCT RANGE | 11 TABLE OF CONTENTS HORTICULTURE APPLICATIONS HORTIPRAY® RANGE FOR HORTICULTURE* FOOD AND INDUSTRIAL APPLICATIONS PRODUCT NAME Bulk density P O pH N-NH Made 2 5 4 MONOAMMONIUM PHOSPHATE - NH4H2PO4 in 3 3 % 1% % Sodium orthophosphates ................................................................................... 03 g/cm lbs/ft indicative indicative indicative Water-soluble fertilisers. Sodium pyrophosphates .................................................................................... 04 HORTIPRAY® MAP Horticultural Grade 0.9 56 61 4.5 12 Sodium tripolyphosphates ................................................................................. 05 HORTIPRAY® MAP 12.60 Horticultural Grade 0.9 56 60 5 12.1 Water-soluble fertilisers; Sodium polyphosphates ..................................................................................... 06 HORTIPRAY® MAP anticalc Horticultural Grade 0.9 56 61 4.5 12 preventive action against clogging. Potassium orthophosphates ............................................................................. -

Ionic Liquid + Biomolecule
Sónia Isabel Pereira Branco Licenciatura em Ciências da Engenharia Química e Bioquímica Aqueous Biphasic System based on Cholinium Ionic Liquids: Extraction of Biologically Active Phenolic Acids Dissertação para obtenção do Grau de Mestre em Engenharia Química e Bioquímica Orientador: Doutora Isabel Maria Delgado Jana Marrucho Ferreira, Investigadora Coordenadora, Laboratório de Termodinâmica Molecular, ITQB-UNL Presidente: Doutora Susana Filipe Barreiros Arguente: Doutor Alexandre Babo de Almeida Paiva Vogal: Doutora Isabel Maria Delgado Jana Marrucho Ferreira Setembro 2014 II UNIVERSIDADE NOVA DE LISBOA Faculdade de Ciências e Tecnologia Departamento de Química Aqueous Biphasic System based on Cholinium Ionic Liquids: Extraction of Biologically Active Phenolic Acids Sónia Isabel Pereira Branco Dissertação apresentada na Faculdade de Ciências e Tecnologia da Universidade Nova de Lisboa para obtenção do grau Mestre em Engenharia Química e Bioquímica Orientadores: Doutora Isabel Maria Delgado Jana Marrucho Ferreira 2014 III IV Aqueous Biphasic Systems based on Cholinium Ionic Liquids: Extraction of Biologically Active Phenolic Acids COPYRIGHT Sónia Isabel Pereira Branco Faculdade de Ciências e Tecnologia Universidade Nova de Lisboa A Faculdade de Ciências e Tecnologia e a Universidade Nova de Lisboa têm o direito, perpétuo e sem limites geográficos, de arquivar e publicar esta dissertação através de exemplares impressos reproduzidos em papel ou de forma digital, ou por qualquer outro meio conhecido ou que venha a ser inventado, e de a divulgar através de repositórios científicos e de admitir a sua cópia e distribuição com objectivos educacionais ou de investigação, não comerciais, desde que seja dado crédito ao autor e editor. V VI Agradecimentos Durante a realização desta tese, contei com o apoio de várias pessoas sem as quais não teria concluído esta etapa. -

IFAC Summary of Phosphate Citations the International Food Additives
IFAC Summary of Phosphate Citations The International Food Additives Council (IFAC) is a global association representing manufacturers of food ingredients, including phosphates used as food additives. IFAC strives for the harmonization of food additive standards and specifications worldwide, and supports regulatory processes to identify, categorize and document the safety of food additives. Phosphorus is an essential element critical for several key biochemical processes in the body, including development of cell membranes, growth of bones and teeth, maintenance of acid-base balance, and cellular energetics. Phosphorus is naturally occurring in various types of foods, including meat, grains, and dairy. Additionally, inorganic phosphates can be added to foods to improve texture, flavor, shelf life, and other technological functions. Inorganic phosphates are salts or esters of phosphoric acid. Phosphoric acid is produced starting with naturally-occurring phosphate ore mined around the world. As phosphoric acid, it can be combined with other elements such as calcium, potassium, and sodium into "salts." Phosphate additives are contained in a large number of processed foods and beverages and help contribute to the vast food supply while also minimizing food waste. Following is a comprehensive list of phosphates that are approved for use in food. All of these phosphates have either been approved by the US Food and Drug Administration (FDA) as a direct food additive or reviewed by FDA and determined to be generally recognized as safe (GRAS). Also included are the CAS numbers, International Numbering System (INS) numbers, Food Chemicals Codex (FCC) references and Joint FAO/WHO Expert Committee on Food Additives (JECFA) evaluations, as available. -

WO 2016/074683 Al 19 May 2016 (19.05.2016) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/074683 Al 19 May 2016 (19.05.2016) W P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C12N 15/10 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/DK20 15/050343 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 11 November 2015 ( 11. 1 1.2015) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (25) Filing Language: English PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: PA 2014 00655 11 November 2014 ( 11. 1 1.2014) DK (84) Designated States (unless otherwise indicated, for every 62/077,933 11 November 2014 ( 11. 11.2014) US kind of regional protection available): ARIPO (BW, GH, 62/202,3 18 7 August 2015 (07.08.2015) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, (71) Applicant: LUNDORF PEDERSEN MATERIALS APS TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, [DK/DK]; Nordvej 16 B, Himmelev, DK-4000 Roskilde DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, (DK). -
Shelf Life and Storage Conditions Statement Icl
Webster Groves Technical Center 373 Marshall Avenue Webster Groves, MO 63119 1-855-ICL-SPEC (1-855-425-7732) www.icl-pp.com SHELF LIFE AND STORAGE CONDITIONS STATEMENT ICL Performance Products, ICL Food Specialties (a division of ICL Performance Products), and ICL Fosfatos y Aditivos México S.A. de C.V. manufacture and/or market high quality phosphates, phosphoric acid, sulfates, adipic acid, sea salt, licorice root extract products, and specialty food ingredient blends for use in food, pharmaceutical, and/or industrial applications. The recommended storage conditions are for materials to be kept at ambient temperatures, low to moderate humidity and in the original packaging. Materials stacked during long-term storage may develop some pressure compaction and require screening or milling before use. This is particularly true of powdered products. In addition, Licresse™ products must be stored in sealed packaging that prevents exposure to light, and under cool and dry conditions. ICL does not guarantee the performance of our products indefinitely since we have no control over how materials are stored. However, if the recommended storage conditions are maintained, performance should be assured for the shelf life listed in the attached table, and in the case of some products, for a much longer period of time. ICL will not recertify expired products for shelf life extension. Lori L. Klopf, Ph.D. Regulatory Affairs Manager Food & Pharmaceutical Ingredients ICL Food Specialties (a division of ICL Performance Products LP) February 5, 2015 The information stated herein is presented in good faith and is believed to be correct as of the date specified in this statement. -
Chemical Specific Parameters May 2019
Regional Screening Level (RSL) Chemical-specific Parameters Supporting Table April 2019 Contaminant Molecular Weight Volatility Parameters Melting Point Density Diffusivity in Air and Water Partition Coefficients Water Solubility Tapwater Dermal Parameters H` HLC H` and HLC VP VP MP MP Density Density Dia Diw Dia and Diw Kd Kd Koc Koc log Kow log Kow S S B τevent t* Kp Kp Analyte CAS No. MW MW Ref (unitless) (atm-m3/mole) Ref mmHg Ref C Ref (g/cm3) Ref (cm2/s) (cm2/s) Ref (L/kg) Ref (L/kg) Ref (unitless) Ref (mg/L) Ref (unitless) (hr/event) (hr) (cm/hr) Ref Acephate 30560-19-1 1.8E+02 PHYSPROP 2.0E-11 5.0E-13 EPI 1.7E-06 PHYSPROP 8.8E+01 PHYSPROP 1.4E+00 CRC89 3.7E-02 8.0E-06 WATER9 (U.S. EPA, 2001) 1.0E+01 EPI -8.5E-01 PHYSPROP 8.2E+05 PHYSPROP 2.1E-04 1.1E+00 2.7E+00 4.0E-05 EPI Acetaldehyde 75-07-0 4.4E+01 PHYSPROP 2.7E-03 6.7E-05 PHYSPROP 9.0E+02 PHYSPROP -1.2E+02 PHYSPROP 7.8E-01 CRC89 1.3E-01 1.4E-05 WATER9 (U.S. EPA, 2001) 1.0E+00 EPI -3.4E-01 PHYSPROP 1.0E+06 PHYSPROP 1.3E-03 1.9E-01 4.5E-01 5.3E-04 EPI Acetochlor 34256-82-1 2.7E+02 PHYSPROP 9.1E-07 2.2E-08 PHYSPROP 2.8E-05 PHYSPROP 1.1E+01 PubChem 1.1E+00 PubChem 2.2E-02 5.6E-06 WATER9 (U.S. -

Biobutanol Recovery from Model Solutions/Fermentation Broth Using Tripotassium Phosphate
Biochemical Engineering Journal 115 (2016) 85–92 Contents lists available at ScienceDirect Biochemical Engineering Journal journal homepage: www.elsevier.com/locate/bej Regular article Biobutanol recovery from model solutions/fermentation broth using tripotassium phosphate Shaoqu Xie, Weini Ji, Yulei Zhang, Yong Zhou, Zeru Wang, Conghua Yi ∗, Xueqing Qiu ∗ School of Chemistry & Chemical Engineering, South China University of Technology, No. 381 Wushan Road, Guangzhou 510640, PR China article info a b s t r a c t Article history: The acetone + 1-butanol + ethanol (ABE) fermentation has a long history but still faces the challenge of Received 19 July 2016 enhancing the low ABE concentration to reduce production cost. Nowadays there is an unprecedented Received in revised form 28 August 2016 resurgence of interest in separation and purification technology to recovery ABE from fermentation broth. Accepted 31 August 2016 Here we describe a simple salting out procedure for extracting ABE fermentation products efficiently from Available online 1 September 2016 model solutions/fermentation broth by employing tripotassium phosphate (K3PO4). Increasing the K3PO4 content permits the liquid-liquid splits and enables the recovery of ABE. The liquid-liquid equilibria were Keywords: mainly determined by the K PO content and slightly affected by temperature and original solvents level. Biobutanol 3 4 Recovery The correlation between the solubility of ABE and the molality of K3PO4 demonstrated this. More than Model solutions/fermentation broth 90 wt% of ABE was recovered from the model solutions/fermentation broth and more than 99.75% of water Salting-out was removed. This study provides a means to reduce the energy demand of the subsequent distillation Tripotassium phosphate process for ABE purification. -

Controlling and Exploiting the Caesium Effect in Palladium Catalysed Coupling Reactions
Controlling and exploiting the caesium effect in palladium catalysed coupling reactions Thomas J. Dent Submitted in accordance with the requirements for the degree of Doctor of Philosophy The University of Leeds School of Chemistry May 2019 i The candidate confirms that the work submitted is his own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the report may be published without proper acknowledgement The right of Thomas Dent to be identified as Author of this work has been asserted by him in accordance with the Copyright, Designs and Patents Act 1988. © 2019 The University of Leeds and Thomas J. Dent ii Acknowledgements This project could not have been completed without the help of several individuals who’ve helped guide the project into the finished article. First and foremost I’d like to thank Dr. Bao Nguyen his support, useful discussions and the ability to sift through hundreds of experiments of kinetic data to put together a coherent figure. My writing has come a long way from my transfer report, so all the comments and suggestions seem to have mostly not been in vain. To Paddy, the discussions relating to the NMR studies and anything vaguely inorganic were incredibly useful, and provided me with data that supported our hypothesis with more direct evidence than just the reaction monitoring experiments. Rob, I really enjoyed my time at AZ and your support during my time there was incredibly useful so I could maximise my short secondment when I was getting more results than I knew what to do with. -

Alkalizer for Fibre Reactive Dyes in Cotton
Europaisches Patentamt J European Patent Office 0 Publication number: 0 283 114 B1 Office_„. europeen„ des brevets ^ © EUROPEAN PATENT SPECIFICATION © Date of publication of patent specification: 25.08.93 © Int. Cl.5: D06P 1/673, D06P 3/66 © Application number: 88300516.7 @ Date of filing: 22.01.88 © Alkalizer for fibre reactive dyes in cotton. © Priority: 17.02.87 US 15428 Qj) Proprietor: SYBRON CHEMICALS INC Birmingham Road Box 66 @ Date of publication of application: Birmingham New Jersey 08011 (US) 21.09.88 Bulletin 88/38 @ Inventor: De Guzman, Ernesto V. © Publication of the grant of the patent: 108 Redwood Circle 25.08.93 Bulletin 93/34 Spartanburg South Carolina 29301 (US) Inventor: Moran, James C. © Designated Contracting States: Route 2 Fews Bridge Road AT BE CH DE FR GB IT LI LU NL SE Taylors South Carolina 29687(US) © References cited: FR-A- 2 148 294 © Representative: Ackroyd, Robert et al W.P. Thompson & Co. Eastcheap House DATABASE WPIL, no.81-42770D,Derwent Central Approach Publications Ltd, London, GB Letchworth Hertfordshire SG6 3DS (GB) CD CO CO CM Note: Within nine months from the publication of the mention of the grant of the European patent, any person ® may give notice to the European Patent Office of opposition to the European patent granted. Notice of opposition £^ shall be filed in a written reasoned statement. It shall not be deemed to have been filed until the opposition fee LU has been paid (Art. 99(1) European patent convention). Rank Xerox (UK) Business Services (3.10/3.6/3.3.1) EP0 283 114 B1 Description Background of the Invention 5 In the dyeing of cellulosic materials using fibre-reactive dyes, it is the practice to add the cellulosic material and dye to the dyebath first. -

Rabbi Eliyahu Shuman Director of Supervision Effective Through 05
May 19, 2021 8 Sivan 5781 Lianyungang Shuren Kechuang Food Additive Co., Ltd. No. 22 Linhong Ave Dapu Industry Park Lianyungang ETDZ, Jiangsu 222000 China This is to certify that the 27 products specified in the listing below, manufactured by LIANYUNGANG SHUREN KECHUANG FOOD ADDITIVE CO., LTD. of the above address, are Kosher and under our supervision. PLEASE NOTE THE FOLLOWING CONDITIONS OF CERTIFICATION: All products listed below are Pareve. All products listed below are certified Kosher when manufactured by Lianyungang Shuren Kechuang Food Additive Co., Ltd., 3212FD008 of Lianyungang ETDZ, Jiangsu, China, as stated on original manufacturer's label. This letter of certification is valid through May 31, 2022 and is subject to renewal at that time. BRAND: Shuren UKD# PRODUCT LISTING SK7VW6IXEB4 Ammonium Citrate SK2AN2SWPOQ Calcium Carbonate SKRTK0CWURQ Calcium Citrate SKBUWKIX2JZ Calcium Propionate SK4F5VTJWIO Dicalcium Phosphate SK5JNRLESGF Dipotassium Phosphate SKDID81LP84 Disodium Phosphate SK2YNHH5HTJ Magnesium Citrate SK6E8L09DX5 Monocalcium Phosphate SKSRPPBEYTC Monopotassium Phosphate SK0GPUP3P9V Monosodium Phosphate SKIT4VB3NJK Potassium Chloride SKWTFX6NM2K Potassium Citrate SKADJ8FFZFY Potassium Sorbate SKK71YHVF8W Sodium Acetate SKJIDKIUPRX Sodium Acid Pyrophosphate (SAPP) SKB6YPFVN6K Sodium Benzoate SKKKBJ98YFJ Sodium Citrate SKFXTLHDB58 Sodium Diacetate Rabbi Eliyahu Shuman Effective Through 05/31/2022 Director of Supervision Page 1 of 2 May 19, 2021 8 Sivan 5781 Lianyungang Shuren Kechuang Food Additive Co., Ltd. No. 22 Linhong Ave Dapu Industry Park Lianyungang ETDZ, Jiangsu 222000 China PLEASE NOTE THE FOLLOWING CONDITIONS OF CERTIFICATION: All products listed below are Pareve. All products listed below are certified Kosher when manufactured by Lianyungang Shuren Kechuang Food Additive Co., Ltd., 3212FD008 of Lianyungang ETDZ, Jiangsu, China, as stated on original manufacturer's label. -

I- Monoammonium Phosphate
Health Canada Santé Canada STATUS DECISION OF CONTROLLED AND NON-CONTROLLED SUBSTANCE(S) Substance: I- Monoammonium phosphate; II- Diammonium phosphate; III- Monocalcium phosphate; IV- Tricalcium phosphate; V- Monopotassium phosphate; VI- Dipotassium phosphate; VII- Tripotassium phosphate; VIII- Monosodium phosphate; IX- Disodium phosphate; X- Trisodium phosphate. Based on the current information available to the Office of Controlled Substances, it appears that the above substance is: Controlled ☐ Not Controlled X under the schedules of the Controlled Drugs and Substances Act (CDSA) for the following reason(s): These substances are not captured under item 22 in Part 1 of Schedule VI to the CDSA. Prepared by: _______________________________________ Date: _______________ Vincent Marleau Verified by: _______________________________________ Date: ________________ Mark Kozlowski Approved by: _______________________________________ Date: ________________ DIRECTOR, OFFICE OF CONTROLLED SUBSTANCES This status was requested by: “third party information removed as per agreement with applicant” 2 Drug Status Report Drug: I- Monoammonium phosphate; II- Diammonium phosphate; III- Monocalcium phosphate; IV- Tricalcium phosphate; V- Monopotassium phosphate; VI- Dipotassium phosphate; VII- Tripotassium phosphate; VIII- Monosodium phosphate; IX- Disodium phosphate; X- Trisodium phosphate. Drug Name Status: I- Monoammonium phosphate; II- Diammonium phosphate; III- Monocalcium phosphate; IV- Tricalcium phosphate; V- Monopotassium phosphate; VI- Dipotassium -
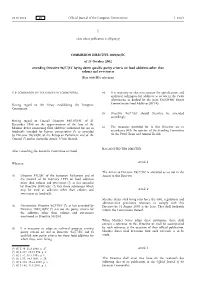
Commission Directive 2002/82/EC Amending Directive 96
28.10.2002 EN Official Journal of the European Communities L 292/1 I (Acts whose publication is obligatory) COMMISSION DIRECTIVE 2002/82/EC of 15 October 2002 amending Directive 96/77/EC laying down specific purity criteria on food additives other than colours and sweeteners (Text with EEA relevance) THE COMMISSION OF THE EUROPEAN COMMUNITIES, (4) It is necessary to take into account the specifications and analytical techniques for additives as set out in the Codex Alimentarius as drafted by the Joint FAO/WHO Expert Having regard to the Treaty establishing the European Committee on Food Additives (JECFA). Community, (5) Directive 96/77/EC should therefore be amended accordingly. Having regard to Council Directive 89/107/EEC of 21 December 1988 on the approximation of the laws of the Member States concerning food additives authorised for use in (6) The measures provided for in this Directive are in foodstuffs intended for human consumption (1), as amended accordance with the opinion of the Standing Committee by Directive 94/34/EC of the European Parliament and of the on the Food Chain and Animal Health, Council (2) and in particular Article 3(3)(a) thereof, HAS ADOPTED THIS DIRECTIVE: After consulting the Scientific Committee on Food, Whereas: Article 1 The Annex to Directive 96/77/EC is amended as set out in the (1) Directive 95/2/EC of the European Parliament and of Annex to this Directive. the Council of 20 February 1995 on food additives other than colours and sweeteners (3), as last amended by Directive 2001/5/EC (4), lists those substances which may be used as additives other than colours and Article 2 sweeteners in foodstuffs.