The Epidemiology of Malaria in Colombia: a Heretical View
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 ¿Qué Es La Cartografía Social?
1 ¿QUÉ ES LA CARTOGRAFÍA SOCIAL? Esta herramienta para construir conocimiento colectivo e integral sobre las dinámicas sociales que se expresan sobre determinada zona es de utilidad para identificar las relaciones sociales, conflictos y oportunidades. 2 ¿CÓMO SE DESARROLLA? Usted deberá responder las preguntas que se realizan a continuación dibujándolas y escribiéndolas sobre una plantilla de mapa. De manera posterior el equipo de Indepaz integrará las cartografías de las personas participantes del taller en una sola y así se construirá una gran cartografía sobre el panorama de la industria de la palma en los departamentos de Meta y Casanare. 3 PREGUNTAS A RESPONDER 1. ¿Dónde están las empresas de palma: plantas, oficinas, cultivos, etc.? 2. ¿Qué problemas identifica en su zona entorno a la industria de la palma: sociales y ambientales? 3. ¿Qué oportunidades y soluciones PLANTILLAS DE MAPAS encuentra de acuerdo a los 4 problemas planteados y entorno a la A continuación se encuentran una serie de mapas base industria de la palma? sobre los cuales usted podrá dibujar la respuesta a las preguntas del punto 3 de esta guía. Los mapas están organizados por departamentos (Meta y Casanare) y regiones; y, contienen información básica como ayuda de ubicación: ríos y vías principales. Usted puede imprimir el mapa que le interese y dibujar sobre él o usarlos como quía para dibujar uno nuevo. A. Departamento del Meta CUNDINAMARCA CASANARE Barranca San Juanito de Upía v El Calvario Cabuyaro Cumaral Restrepo Villavicencio Puerto López Acacias Puerto Gaitán Guamal Cubarral Castilla la San Carlos de Nueva Guaroa VICHADA El Dorado Lejanías El Castillo Granada San Martín Fuente de Oro Mesetas San Juan de Arama Puerto Lleras HUILA La Uribe Mapiripán Puerto Puerto Rico Vista Hermosa Concordia La Macarena GUAVIARE CAQUETÁ A-1. -
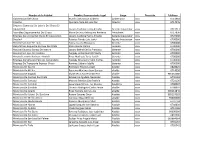
Nombre De La Entidad
Nombre de la Entidad Nombre Representante Legal Cargo Dirección Teléfono Gobernacion Del Choco Murillo Urrutia Luis Gilberto Gobernador xxxx 6713983 Indecho Quintero Peña Edinson Yair Director xxxx 6714976 Empresa Comercial De Loteria Del Choco En Liquidacion Lozano Cordoba Henry Arcadio Gerente Liquidador xxxx 6713711 Asamblea Departamental Del Choco Maria De Jesus Mosquera Renteria Presidente xxxx 6717836 Empresa De Licores Del Choco En Liquidacion Lozano Cordoba Henry Arcadio Gerente Liquidador xxxx 6729000 Dasalud Palacios Parada Luis Javier Agente Interventor xxxx 6700000 Hospital San Jose De Tado Yocira Lozano Mosquera Gerente xxxx 6700000 Hospital San Roque De Carmen De Atrato Mazo Rivera Natalia Gerente xxxx 6700000 Hospital Eduardo Santos De Itsmina Lozano Beltral Emilio Francisco Gerente xxxx 6700000 Hospital San Jose De Condoto Yurgaky Jordan Hailieth Yoarly Gerente xxxx 6700000 Hospital Lascario Barbosa - Acandi Rivas Machado Tania Yadith Gerente xxxx 6700000 Empresa De Servicios Públicos De Condoto Yurgaky Mosquera Yamil Andres Gerente xxxx 6700000 Empresa De Transporte Expreso Choco Ramirez Cabrera Adolfo Gerente xxxx 6700000 Municipio De Acandi Rodriguez Palacios Azael Alcalde xxxx 6828425 Municipio De Atrato Bejarano Martinez Juan Genecy alcalde xxxx 6714050 Municipio De Bagadó Ely De Jesus Moreno Moreno alcalde xxxx 985662680 Municipio De Carmen De Atrato Echavarria Agudelo Alexander Alcalde xxxx 6790183 Municipio De Certegui Moreno Palacios Lina Patricia Alcalde xxxx 6721120 Municipio De Condoto Agualimpia Benitez Luz -

Resolución No. 5024 Chocó
cNs Comalia riSCIOrtal Electoral COLOMBIA RESOLUCIÓN No. 5024 DE 2019 (18 de septiembre) Por medio del cual se adoptan decisiones en relación con la inscripción irregular de cédulas de ciudadanía, en los Municipios de Alto Baudo, Atrato, Bagado, Bojaya, El Cantón de San Pablo, Carmen del Darién, Certeguí, Condoto, El Carmen de Atrato, El Litoral del San Juan, lstmina, Juradó, Lloró, Medio Baudó, Medio San Juan, Nóvita, Nuqui, Río !ro, Río Quito, Riosucio, Sipl, Tadó y Unión Panamericana, Departamento del Chocó, para las elecciones de autoridades locales de 27 de octubre del año 2019. EL CONSEJO NACIONAL ELECTORAL En ejercicio de sus atribuciones Constitucionales y legales, en especial las conferidas en los artículos 265 numeral 6° y 316 de la Constitución Política, 4° de la ley 163 de 1994, la Resolución No. 2857 de 2018 del Consejo Nacional Electoral y con fundamento en los siguientes: 1. HECHOS Y ACTUACIONES ADMINISTRATIVAS 1.1. El 27 de octubre de 2019 se realizarán en todo el país las elecciones para elegir Autoridades Locales (Gobernadores, Alcaldes, Diputados, Concejales y Miembros de Juntas Administradoras Locales). 1.2. En reparto especial del 14 de noviembre de 2018, correspondió al Despacho del Magistrado Jorge Enrique Rozo Rodríguez, conocer de las investigaciones, por presuntas irregularidades en la inscripción de cédulas de ciudadanía, en los municipios del Departamento de Chocó. 1.3. Mediante los siguientes Autos el Consejo Nacional Electoral, a través del Magistrado Jorge Enrique Rozo Rodriguez, asumió el conocimiento y ordenó iniciar el procedimiento administrativo para determinar la posible inscripción irregular de algunas cédulas de ciudadania en los Municipios de Alto Baudo, Atrato, Bagadó, Bojaya, El Cantón del San Pablo, Carmen del Darién, Cértegui, Condoto, El Carmen de Atrato, El Litoral del San Juan, Istmina, Juradó, Lloró, Medio Baudó, Medio San Juan, Nóvita, Nuquí, Río Iro, Río Quito, Riosucio, Sipí, Tadó y Unión Panamericana, Departamento del Chocó. -

Presentación De Powerpoint
INFORME DE INCENDIOS FORESTALES 01DE ENERO – 15 ABRIL DE 2018 DNBC Elaboro: Sala Situacional. MUNICIPIOS UNIDADES NUMERO DEPARTAMENTO MUNICIPIOS EVENTOS AFECTADOS BOMBERILES MAQUINAS AMAGÁ, AMALFI, BELLO, CAREPA, CAUCASIA, CONCORDIA, COPACABANA, EL BAGRE, ENTRERRIOS, ENVIGADO, GIRARDOTA, HELICONIA, ITAGUI, JERICÓ, LA ESTRELLA, MARINILLA, MEDELLÍN, OLAYA, ANTIOQUIA 131 32 958 203 PUERTO NARE, PUERTO TRIUNFO, REMEDIOS, SALGAR, SAN JERÓNIMO, SAN PEDRO DE URABA, SANTA BÁRBARA, SANTA ROSA DE OSOS, SEGOVIA ,SOPETRÁN, TURBO, URRAO ,YOLOMBÓ Y ZARAGOZA. ARAUCA ARAUQUITA Y TAME 15 02 86 19 CANDELARIA, GALAPA, JUAN DE ACOSTA, MALAMBO, SABANALARGA, 31 07 241 44 ATLANTICO SUAN Y TUBARA. BOGOTÁ D.C. BOGOTÁ D.C. 01 01 20 04 ARJONA, CALAMAR, CLEMENCIA,CORDOBA, EL CARMEN DE BOLIVAR, BOLIVAR MAGANGUÉ, MAHATES, MOMPOS, SAN JUAN DE NEPOMUCENO, SANTA 84 13 412 94 ROSA DEL SUR, SIMITÍ , TURBACO Y TURBANÁ. ALMEIDA, AQUITANIA, BELÉN, BOYACÁ, BUENAVISTA, BUSBANZÁ, CHINAVITA, CHIQUIZA, CHITARAQUE, CHIVATÁ, CIÉNEGA, COMBITA, CUÍTIVA, DUITAMA, FIRAVITOBA, FLORESTA, GAMEZA, GUATEQUE, JENESANO, LABRANZAGRANDE, MACANAL, MONIQUIRÁ, NOBSA, NUEVO BOYACA 130 46 861 202 COLÓN, OICATÁ, PAIPA, PAUNA, PESCA, PUERTO BOYACÁ, RAMIRIQUÍ, SAN PABLO DE BORBUR, SANTA ROSA DE VITERBO, SIACHOQUE, SOATÁ, SOGAMOSO, SOMONDOCO, SORACÁ, SOTAQUIRÁ, SUTATENZA, TIBASOSA, TOPAGA, TUNJA, TURMEQUÉ, TUTA Y VILLA DE LEYVA. CALDAS ANSERMA, LA DORADA, VICTORIA Y VITERBO. 13 04 48 14 CAQUETA BELÉN DE LOS ANDAQUÍES , FLORENCIA Y SAN VICENTE DEL GAGUAN. 26 03 170 36 AGUAZUL, MANÍ, NUNCHÍA, OROCUÉ, PAZ DE ARIPORO, PORE, CASANARE SABANALARGA, SAN LUIS DE PALENQUE, TÁMARA, TAURAMENA, 205 13 1.309 304 TRINIDAD, VILLANUEVA Y YOPAL. CAUCA MIRANDA Y POPAYAN. 03 12 12 03 AGUACHICA, BECERRIL, CURUMANI, EL COPEY, EL PASO, LA JAGUA DE CESAR 94 11 647 130 IBIRICO, LA PAZ, PELAYA, RIO DE ORO, SAN ALBERTO Y VALLEDUPAR. -

Plan Operativo Anual (POA)
PLAN DE INVERSIONES “TODOS POR EL PACÍFICO - CHOCÓ” PLAN OPERATIVO ANUAL POA 2015 Empresa de Acueducto y Alcantarillado de Pereira S.A. E.S.P Pereira, 28 de agosto de 2015 “TODOS POR EL PACÍFICO -CHOCÓ” PLAN OPERATIVO ANUAL POA 2015 CONTRATO INTERADMINISTRATIVO No. 186 de 2010 Pereira, 28 de agosto de 2015 Tabla de contenido 1 BREVE DIAGNÓSTICO DEL ACCESO A AGUA Y SANEAMIENTO: .................................................. 6 2 JUSTIFICACION DE LAS VARIACIONES DEL POA 4 RESPECTO AL POG APROBADO. .................. 58 3 COORDINACION DE OBRAS DEL PROGRAMA CON LAS OBRAS DE RECURSOS EXTERNOS. ..... 58 4 ESTRATEGIA PARA EL SISTEMA DE SEGUIMIENTO DE LA CALIDAD DE AGUA........................... 58 5 ACTIVIDADES QUE FINALIZAN POSTERIOR AL CONTRATO 186 DE 2010 .................................. 59 6 EXPLICACION DE ALGUNOS DE LOS PRODUCTOS MENCIONADOS EN EL POA. ........................ 61 7 COORDINACION INTERINSTITUCIONAL SEDE QUIBDO ............................................................. 61 8 MATRIZ DE RESULTADOS........................................................................................................... 61 9 PLAN DE ADQUISICIONES .......................................................................................................... 61 10 CRONOGRAMA ...................................................................................................................... 61 11 ESTADO DE LOS PRODUCTOS A DICIEMBRE 31 DE 2014 ...................................................... 62 12 LIMITANTES DE LA EJECUCIÓN DEL POA 2015 -

Diapositiva 1
Communitarian State: Development for All, and its Application to the Pacific National Planning Department June 3rd, 2007 Index 1.1. WWhhaatt isis mmeaeanntt byby ththee PPaacciifificc RRegegiioon?n? 2.2. WWhhyy hhaaveve aa ppoolilicycy foforr ththee PPaciacifificc?? 3.3. HHowow iiss ththee ppoolilicycy fforor ththee PPaacifcificic ddeeveveloloppeed?d? 4.4. WWhhaatt dodoeess ththee ssttrraateteggyy conconsisistst oof?f? • AA vivisisioonn comcombibinedned wiwithth stratstrategiegicc oobjbjectiectivveses • AA rolrolee forfor thethe PaciPacifificc wiwithithinn thethe NNatiationonalal DeDevelvelopopmentment PPllanan − DemocDemocratiraticc popolliicycy wwithith ssociociaallllyy iintegntegratedrated assassiistastancence − PovPovertyerty rereductductiionon aandnd propromotingmoting ofof equaequalliityty − StrongStrong andand sussustaitainanablblee devedevellopmeopmentnt − EnvEnviironmeronmentalntal manamanagemegementnt whiwhicchh fosfostersters devdevelelopopmentment − SpecSpeciialal aspeaspectscts ofof dedevelveloopmenpmentt • StrenStrengtheninggthening ofof succsuccessfulessful casescases Index • WWhhaatt isis mmeaeanntt byby ththee PPaacciifificc RRegegiioon?n? • Why have a policy for the Pacific? • How is the policy for the Pacific developed? • What does the strategy consist of? • A vision combined with strategic objectives • A role for the Pacific within the National Development Plan − Democratic policy with socially integrated assistance − Poverty reduction and promoting of equality − Strong and sustainable development − Environmental management -

Guainía En Sus Asentamientos Humanos
GUAINÍA En sus asentamientos humanos INSTITUTO AMAZÓNICO DE INVESTIGACIONES CIENTÍFICAS SINCHI GUAINÍA En sus asentamientos humanos Carlos Ariel Salazar C. Franz Gutiérrez R. Martín Franco A. Diciembre de 2006 Salazar C., Carlos Ariel; Gutiérrez R., Franz; Franco A., Martín. Guainía en sus asentamientos. Carlos Ariel Salazar C, Franz Gutiérrez R., Martín Franco A. Bogotá, Colombia: Instituto Amazónico de Investigaciones Científicas- Sinchi, 2006 1. GEOGRAFÍA ECONÓMICA 2. DINÁMICA POBLACIONAL 3. ASENTAMIENTOS HUMANOS 4. GUAINÍA Revisión técnica: Camilo Domínguez ISBN: Instituto Amazónico de Investigaciones Científicas – Sinchi Ministerio de Ambiente, Vivienda y Desarrollo Territorial Primera edición: Noviembre de 2006 Diseño: Julián Hernández Impresión: Panamericana Formas e Impresos Reservados todos los Derechos El contenido de esta publicación es propiedad del Instituto Amazónico de Investigaciones Científicas -Sinchi- Prohibida su reproducción con fines comerciales. Disponible en: Instituto Sinchi, Calle 20 No. 5-44 Tel.: 4442060, www.sinchi.org.co Impreso en Colombia LUZ MARINA MANTILLA CÁRDENAS Directora General ROSARIO PIÑERES VERGARA Subdirectora Administrativa y Financiera Carlos Ariel Salazar Cardona DIRECTOR DE PROYECTO Grupo Procesos de Ocupación, Poblamiento y Urbanización en la Región Amazónica Grupo Colciencias Categoría A 5 6 TABLA DE CONTENIDO PREFACIO 13 INTRODUccIÓN 19 PERSPEctIVA GENERAL 23 ANTECEDENTES 23 IMPORTANCIA INTERNACIONALDE LOS ASENTAMIENTOS HUMANOS 24 ASENTAMIENTOS HUMANOSDEL ORIENTE AMAZÓNICO. UNA PROPUESTA -

Caracterización De La Infraestructura Tecnológica, Las Organizaciones Y El Apoyo Institucional En La Agroindustria De Los Muni
CARACTERIZACIÓN DE LA INFRAESTRUCTURA TECNOLÓGICA, LAS ORGANIZACIONES Y EL APOYO INSTITUCIONAL EN LA AGROINDUSTRIA DE LOS MUNICIPIOS DE GRANADA, FUENTE DE ORO Y EL CASTILLO – META PARA LOS PLANES DE ENERGIZACIÓN RURAL SOSTENIBLES – PERS: UNA OPCIÓN PARA EL DESARROLLO RURAL PRODUCTIVO CARLOS ALBERTO GUEVARA PÁEZ UNIVERSIDAD DE LOS LLANOS FACULTAD DE CIENCIAS AGROPECUARIAS Y RECURSOS NATURALES INGENIERÍA AGROINDUSTRIAL VILLAVICENCIO – META 2018 CARACTERIZACIÓN DE LA INFRAESTRUCTURA TECNOLÓGICA, LAS ORGANIZACIONES Y EL APOYO INSTITUCIONAL EN LA AGROINDUSTRIA DE LOS MUNICIPIOS DE GRANADA, FUENTE DE ORO Y EL CASTILLO – META PARA LOS PLANES DE ENERGIZACIÓN RURAL SOSTENIBLES – PERS: UNA OPCIÓN PARA EL DESARROLLO RURAL PRODUCTIVO AUTOR: CARLOS ALBERTO GUEVARA PÁEZ TÍTULO A OBTENER: INGENIERO AGROINDUSTRIAL ÁREA DE PROFUNDIZACIÓN: INNOVACIÓN AGROEMPRESARIAL LÍNEA DE INVESTIGACIÓN: DESARROLLO Y CRECIMIENTO ECONOMICO DIRECTOR (A): LUZ MERY BARRERA R. UNIVERSIDAD DE LOS LLANOS FACULTAD DE CIENCIAS AGROPECUARIAS Y RECURSOS NATURALES INGENIERÍA AGROINDUSTRIAL VILLAVICENCIO – META 2018 AGRADECIMIENTOS Mi total gratitud es para Dios, por mostrarme el camino y darme la sabiduría necesaria que me permitieron culminar con éxitos mis estudios. A mis padres, por sus incansables muestras de apoyo, afecto y cariño que propiciaron en mí los más excelentes valores y principios. También quiero compartir mis agradecimientos con mi Directora de Grado la Profesora Luz Mery y con todos aquellos quienes estuvieron detrás del desarrollo de este trabajo aportando valiosos -

La Historia De Mapiripán
El conflicto histórico por la tierra en el municipio de Mapiripán – Meta “… a Mapiripán llegamos donde la gente vivía de la buena fe, lo que primaba allá era la palabra, la palabra era una escritura, yo recuerdo lo que decía mi padre que uno tenía que hacer honor a la palabra y en Mapiripán la palabra era la última verdad, allí la gente Equipo de Investigación compraba las fincas con el solo hecho de dar la palabra”. Carlos Bonell (Conrado Salazar, habitante de Mapiripán y ex alcalde del municipio). Emil Villamizar Olga Silva “mientras allá los campesinos de Mapiripán en el 97 trabajaban el campo todos allá, pues po- demos ver que los empresario y banqueros y políticos también de la región y de nivel nacional se reunieron para pensar cómo era que iban a sacar esos campesinos de Mapiripán y pues la salida fue sembrar el terror en Mapiripán con los grupos paramilitares” (JC habitante de Mapiripán desplazado). Olga Silva Coordinadora General del proyecto Humanidad Vigente Colombia, 2016. Todos los derechos reservados. Una publicación de: Introducción Un poco de historia Mapiripán es un municipio ubicado en el extremo suroriental de las sabanas del departamento del Los primeros pasos para su fundación están relacionados con el auge cauchero que tuvo lugar a prin- Meta, en frontera con las selvas del Guaviare, a orillas del río que lleva el mismo nombre. Tristemente cipios del siglo XX en esta región, donde la explotación cauchera atrajo mano de obra de trabajadores célebre, es conocido en la historia de Colombia, sólo a partir de 1997 cuando se produce la llamada de regiones circundantes, en dicha época esta zona era un corregimiento del municipio de San Martín. -

Meta Fecha De Realización Del Informe: 09 De Diciembre De 2019 Nombre De Quien Elabora El Informe: Juliana Daniela Padilla Castillo 1
FORMATO DE PREPARACIÓN DE INFORMACIÓN PARA LA RENDICIÓN DE CUENTAS Periodo a reportar: 01 de diciembre de 2018 al 31 de diciembre de 2019 Página: 1 de 26 DATOS GENERALES Dependencia y /o Regional: Meta Fecha de realización del informe: 09 de diciembre de 2019 Nombre de quien elabora el informe: Juliana Daniela Padilla Castillo 1. Meta del Plan Estratégico Institucional1 1. Acompañamientos Psicojurídicos en procesos Judiciales de víctimas. (No. de acompañamientos Psicojurídicos en procesos Judiciales de víctimas atendidos / 0 No. de acompañamientos Psicojurídicos en procesos Judiciales de víctimas solicitados) 2. No. de víctimas orientadas en las audiencias. 0 3. Sesiones de la Mesa de Participación acompañadas (No. de sesiones de Mesa de Participación realizadas / No. de sesiones de Mesa de Participación ordenadas por el protocolo de participación) 8 4. Comités territoriales de justicia transicional. (No. de participaciones en Comités territoriales de justicia transicional / No. de Comités territoriales de justicia transicional convocados) 17 5. No. de Trámites por la vía Judicial 98 6. No. de Tramites por la vía Administrativa 646 7. No. de solicitudes de representante judicial para procesos de justicia y paz, diligenciadas y remitidas a 5 Defensoría Pública en el proceso de Justicia y Paz. 8. No. de orientaciones y asesorías individual realizadas 2182 9. Eventos del componente grupal de la estrategia psicojurídica. (No. de eventos del componente grupal de la estrategia psicojurídica realizadas / No. de eventos del componente grupal de la estrategia psicojurídica 56 programadas y convocadas) 10. No. de víctimas orientadas en las actividades del componente grupal de la estrategia psicojurídica. 1657 11. Declaraciones recibidas en la Regional para sujetos colectivos no étnicos (No. -

Diagnóstico Departamental Meta
Diagnóstico Departamental Meta Procesado y georeferenciado por el Observatorio del Programa Presidencial de DH y DIH Vicepresidencia de la República Fuente base cartográfica: Igac Introducción El departamento de Meta limita por el norte con en hogares tiene Necesidades Básicas Cundinamarca, Casanare y Bogotá D.C., por el Insatisfechas (NBI) y al igual que en la mayoría de este con Vichada, por el sur con Caquetá y los departamentos del país, las personas más Guaviare, y por el occidente con los departamentos afectadas se encuentran en las zonas más alejadas de Huila y Cundinamarca. De acuerdo con el censo de los centros administrativos. En Meta, el 44,4% 20051, el departamento está dividido en 29 del total de la población rural tiene NBI, en municipios, que suman 789.276 habitantes, de los comparación con el 20,2% de los habitantes de las cuales 579.195 habitan en los cascos urbanos y los zonas urbanas con esta problemática. 210.081 restantes en las zonas rurales. De acuerdo con esta fuente, el 24,8% de la población Para efectos de este estudio, se llevará a cabo una regionalización del departamento en 5 subregiones, según la dinámica de la confrontación 1 Dane, Censo 2005. 1 Diagnóstico Departamental Meta armada en cada una de ellas. La primera se una cadena de unos doce frentes, que partía desde denominará Ariari–Guayabero, y está conformada Uribe, en Meta y que llegaba hasta la frontera con por los siguientes municipios: El Castillo, El Venezuela, con lo que también se buscaba dividir Dorado, Fuente de Oro, Granada, La Macarena, la Orinoquía y la Amazonía del resto del país2. -

Principales Cultivos Por Área Sembrada En 2017
Meta Principales Cultivos por Área Sembrada en 2017 Área Sembrada (ha) Área Cosechada (ha) Producción (t) Rendimiento (t/ha) Cultivo Variación Participación Variación Participación Variación Participación Variación 2016 2017 (%) (%) 2016 2017 (%) (%) 2016 2017 (%) (%) 2016 2017 (%) TOTAL 523.522 617.232 17,9 100,0 390.165 494.454 26,7 100,0 3.350.094 5.041.186 50,5 100,0 8,59 10,20 18,7 Palma de Aceite 221.090 231.826 4,9 37,6 153.246 171.689 12,0 34,7 478.790 698.220 45,8 13,9 3,12 4,07 30,2 Maíz Tecnificado 79.150 84.027 6,2 13,6 63.484 81.547 28,5 16,5 420.462 485.665 15,5 9,6 6,62 5,96 - 10,1 Arroz Mecanizado 77.335 82.756 7,0 13,4 79.005 82.070 3,9 16,6 413.260 394.032 - 4,7 7,8 5,23 4,80 - 8,2 Soya 28.237 65.086 130,5 10,5 21.630 50.811 134,9 10,3 54.895 145.578 165,2 2,9 2,54 2,87 12,9 Caña Azucarera 16.750 31.000 85,1 5,0 14.238 26.624 87,0 5,4 1.195.950 2.236.453 87,0 44,4 84,00 84,00 - Plátano 24.412 26.545 8,7 4,3 15.060 21.607 43,5 4,4 274.197 434.292 58,4 8,6 18,21 20,10 10,4 Caucho 21.846 22.775 4,3 3,7 2.433 2.599 6,8 0,5 3.496 3.725 6,6 0,1 1,44 1,43 - 0,2 Maíz Tradicional 4.520 16.277 260,1 2,6 6.468 15.241 135,6 3,1 14.242 18.085 27,0 0,4 2,20 1,19 - 46,1 Cacao 10.359 9.232 - 10,9 1,5 5.076 6.513 28,3 1,3 3.358 4.034 20,1 0,1 0,66 0,62 - 6,4 Yuca 6.969 9.014 29,3 1,5 6.544 7.752 18,5 1,6 103.174 149.242 44,7 3,0 15,77 19,25 22,1 Otros Cultivos 32.853 38.694 17,8 6,3 22.983 28.001 21,8 5,7 388.269 471.860 21,5 9,4 16,89 16,85 - 0,3 FUENTE: Ministerio de Agricultura y Desarrollo Rural.