Patient and Public Participation Group Minutes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Situation of Notice of Polling Stations PCC 2021
Police and Crime Commissioner Election Situation of polling stations Police area name: PCC Voting Area Voting area name: Warwick District Council No. of polling Situation of polling station Description of persons entitled station to vote 1 Shrewley Village Hall, 75 Shrewley Common, KDK-1 to KDK-723 Shrewley, Warwick 2 Bishops Tachbrook Sports & Social Club WAA-1 to WAA-902 STATION A, The Playing Fields, Kingsley Road, Bishops Tachbrook 3 Bishops Tachbrook Sports & Social Club WAA-903 to WAA-1686 STATION B, The Playing Fields, Kingsley Road, Bishops Tachbrook 4 Heathcote Parish Church STATION D, Warwick WAB-1 to WAB-1146 Gates Community Centre, Cressida Close, Warwick 5 Heathcote Parish Church STATION E, Warwick WAB-1147 to WAB-2310 Gates Community Centre, Cressida Close, Warwick 6 Hatton Park Village Hall, Barcheston Drive, WBA-1/1 to WBA-1423 Hatton Park 7 Hatton Village Hall, Birmingham Road, Hatton WBB-1 to WBB-206 8 Budbrooke Village Hall, Old School Lane, WBC-1 to WBC-337 Hampton on the Hill, Warwick 9 Budbrooke Community Centre, Field Barn WBD-1 to WBD-1195 Road, Hampton Magna 10 Norton Lindsey Village Hall, Wolverton Road, WBE-1 to WBE-333 Norton Lindsey 11 Sherbourne Village Hall, Sherbourne WBF-1 to WBF-126 12 Barford Memorial Hall, Church Street, Barford WBG-1 to WBG-1291 13 Wasperton Village Hall, Wasperton WBH-1 to WBH-131 14 Leek Wootton Village Hall, Warwick Road, Leek KCA-1 to KCA-783 Wootton 14 Leek Wootton Village Hall, Warwick Road, Leek WCA-1 to WCA-14 Wootton 15 Stoneleigh Village Hall, Birmingham Road, KCB-1 to KCB-540 -

Warwick District
Warwick District Personal Details: Name: Charles BOURNE E-mail: Postcode: Organisation Name: Comment text: I am very pleased to see that the Boundary Commission has decided to proceed with its own proposals, rather than adopting any of those put forward by Warwick District Council or any of the political parties (although some of these were more reasonable than others!). I totally support the objective of the Boundary Commission of creating wards with the least variation from the population average, and aligning wards as far as possible with the County Council divisions adopted following their most recent revision. However, I wish particularly to express my SUPPORT for two aspects of the Boundary Commission's proposals, both of which "correct" very unfortunate aspects of the County Council boundaries: (1) To include the area between the railway line and the River Leam in Clarendon Ward rather than Brunswick. I live in this area and can categorically confirm that the community on and around Avenue Road/Adelaide Road identify with and consider ourselves part of Leamington Spa town centre and North Leamington (Clarendon Ward or Milverton Ward), and not South Leamington (Brunswick). I am very grateful that members of the Commission took the trouble to visit this area, and affirm their view that hard geographical features separate our area from Brunswick ward. (2) To broaden Milverton Ward across Kenilworth Road so that the ward is coherent, compact and geographically rational. I hope that whatever changes the Boundary Commission might make to these proposals as a result of this consultation, they will not make any alteration to these two elements. -

"Doubleclick Insert Picture"
481, Tachbrook Road, Whitnash, Leamington Spa, CV31 3DQ "DoubleClick Insert Picture" 481, Tachbrook Road, Whitnash, Leamington Spa, CV31 3DQ Offers in Excess of: £650,000 A three bedroom detached property in need of some modernisation with an ‘in and out’ driveway and double garage with a one bedroom self-contained flat over. Features • Three double bedrooms • One bedroom self-contained flat • In an out driveway • Parking for several vehicles • Two reception rooms • Conservatory • Two garages • Open fire place • Mature rear garden Location Whitnash is located two miles from Leamington Spa town centre and has a church and three neighbourhood shopping areas at Coppice Road, Heathcote Road, and Home Farm Crescent. There is a community hall, library and information centre as well as four primary schools. Campion School, Myton School and Trinity Catholic School name Whitnash as being within their priority area. For recreation there is a sports and social club, tennis club, petanque club, football and rugby club, as well as Leamington and County golf club which is also within the parish. The property is ideally situated for the commuter with easy access to major road networks including the M40 and M42. Leamington railway station is easily accessible and offers trains into London Marylebone. Alternatively, direct rail services are offered from nearby Warwick Parkway and Coventry and services into London Euston take just over an hour. Birmingham International Airport is just half an hour’s drive from the property. Flat Accessed via stairs behind a UPVC door in between the two garages. This self-contained area has a double bedroom with storage cupboard, further storage cupboard accessed from the landing, a bathroom with airing cupboard, separate WC and open plan kitchen/sitting room. -

Warwick District Council Ward Boundaries Warwick District Council Submission on Warding Arrangements
LGBCE Review of Warwick District Council Ward Boundaries Warwick District Council Submission on Warding Arrangements 1.0 Introduction 1.1 This submission is made on behalf of Warwick District Council and is based upon the decision of the Council’s Licensing & Regulatory Committee on 11 January 2018. 1.2 This Council has a fundamental principle that wherever reasonably practicable the Electoral Boundaries should be coterminous, but in doing so they should meet the criteria for electoral equality, the interests and identities of local communities and should promote effective and convenient local government 1.3 Having considered this the Council believes that the proposal it has outlined in this submission meets the criteria for the review and would provide an approach that would best meet the needs of the local communities within Warwick District. 1.4 To achieve this outcome, the Council is proposing 20 Wards with a mixture of 1, 2 and 3 Councillors to represent each Ward to give electoral equality but also to recognise the individual communities within the District. 2.0 Delivering electoral equality for local voters 2.1 The Local Government Boundary Commission for England (LGBCE) has accepted the methodology for local elector growth within Warwick District from 109,855 in September 2017 to 123,333 in 2023. Following the decision by the LGBCE to set the Council size at 44, this provides an elector to councillor ratio in 2023 of 2803 to each Councillor. 2.2 The proposal from this Council works on a principle of coterminous boundaries across the District except for a few exceptions, to improve electoral equality within the towns of Leamington and Warwick. -

4248 the London Gazette, I?Th May 1963 National Coal Board Highways Act, 1959
4248 THE LONDON GAZETTE, I?TH MAY 1963 WARWICKSHIRE COUNTY COUNCIL NATIONAL COAL BOARD SURVEY OF RIGHTS OF WAY Boroughs of Leamington Spa and Warwick COAL ACT, 1938, AND COAL INDUSTRY Urban District of Kenilworth NATIONALISATION ACT, 1946 Rural District of Warwick Notice is hereby given that pursuant to paragraph Notice is hereby given that the Warwickshire County 6 (2) of the Second Schedule of the Coal Act, 1938, Council, in accordance with the provisions of section the National Coal Board propose to exercise the right 32 of the National Parks and Access to the Country- to withdraw support vested in them by virtue of side Act, 1949, have prepared a Definitive Map and Paragraph 6 (1) of the said Schedule and the Coal Statement in respect of rights of way in the Boroughs Industry Nationalisation Act, 1946, so far as the of Leamington Spa and Warwick, the Urban District said right applies in relation to any land within an of Kenilworth and the Rural District of Warwick, area situate in the Municipal Borough of Prestwich showing footpaths and bridleways wherever, in their indicated on a plan which is deposited and open for opinion, such public rights of way subsist or are •inspection at the National Coal Board's North reasonably alleged to have subsisted on the relevant Western Divisional Survey and Mineral Estates dates for the purposes of the said Act. Office, 40 Portland Street, Manchester 1. Dated 13th May 1963. Copies of the Map and Statement may be inspected, free of charge on any weekday during normal office M. -
Warwick District
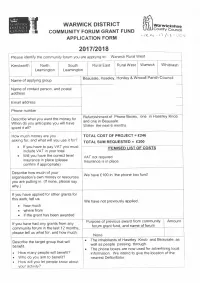
WARWICK DISTRICT ~ Warwickshire COMMUNITY FORUM GRANT FUND t/1J County Council ,,,._J(<__ V'-1 - II /1 6 - 00 (,, APPLICATION FORM 2017/2018 Please identify the community forum you are applying to: Warwick Rural West Kenilworth North South Rural East Rural West Warwick Whitnash Leamington Leamington Beausale, Haseley, Honiley & Wroxall Parish Council Name of applying group - Name of contact person, and postal address - Email address - Phone number Refurbishment of Phone Boxes, one in Haseley Knob Describe what you want the money for. and one in Beausale. When do you anticipate you will have Within the next 6 months spent it all? How much money are you TOTAL COST OF PROJECT = £246 asking for, and what will you use it for? TOTAL SUM REQUESTED = £200 • If you have to pay VAT you must ITEMISED LIST OF COSTS include VAT in your total • Will you have the correct level VAT not required insurance in place {please Insurance is in place confirm if appropriate) Describe how much of your We have £100 in 'the phone box fund' organisation's own money or resources you are putting in. {If none, please say why.) If you have applied for other grants for this work, tell us: We have not previously applied. • how much • where from • if the grant has been awarded Purpose of previous award from community Amount If you have had any grants from any forum grant fund, and name of forum community forum in the last 12 months, please tell us what for, and how much. None The inhabitants of Haseley .Knob and Beausale, as Describe the target group that will • well as people passing through. -

Locality Name: NORTH LEAMINGTON
Community Forum Profile July 2009 Community Forum Name: Southam District: Stratford-on-Avon Description of Community Forum Area The Southam Community Forum Area comprises the wards of Harbury, Long Itchington, Southam, Stockton and Napton and part of Fenny Compton. It includes the County Council Electoral Divisions of Feldon and Southam. The area is essentially rural in nature with a mix of small towns, villages, hamlets and farms. It borders the outskirts of Whitnash and Leamington Spa to the west and Daventry in Northamptonshire to the east. © Crown Copyright. All rights reserved. Warwickshire County Council, 100019520, 2008. Population: Southam Warwickshire Community Forum No. % No. % Total Population (Mid-2006)1 17,190 522,200 Male/Female Split1 49 / 51 49 / 51 Total 0-15 year olds1 3,541 20.6 97,839 18.7 Total Working Age* Population1 10,194 59.3 320,363 61.3 Total 65+ Males, 60+ Females1 3,455 20.1 104,030 19.9 Non-White British Population2 638 3.7 36,553 7.2 Urban/Rural Population Split1,3 0 / 100 68 / 32 *16-64 Males, 16-59 Females Households: Southam Warwickshire Community Forum No. % No. % Total Resident Households2 6,790 210,898 Average Household Size2 2.49 2.37 Socially Rented Housing2 823 12.1 30,196 14.3 Terraced Housing2 1,154 16.4 51,458 23.6 Households with no car/van2 874 12.8 40,130 19.0 Econom y & Employment: Southam Warwickshire Community Forum No. % No. % Mean Household Income5 £37,100 £34,600 Job-Seekers Allowance Claimants4 126 1.2 5,998 1.9 (June 2008) All Working Age Benefit Claimants4 705 6.9 33,800 10.5 (February 2008) - Incapacity Benefit4 320 3.1 16,130 5.0 - Lone Parent Benefit4 100 1.0 4,260 1.3 www.warwickshireobservatory.org Community Forum Profile July 2009 Southam Warwickshire Occupation of those aged 16-74 in Community Forum Employment2 No. -

Leamington & Warwick
to University of Warwick, W e Kenilworth sth d ill to a 69 and Coventry o Ro Weston under Leamington & Warwick R a d h d g oa Wetherley i R le K y e en gb to Kenilworth n ilw Ru o o t rt Where to catch your bus S h R s e d. Cubbington Warwick s n from Warwick Bus Station 16 a a p L - ©P1ndar ©P1ndar ©P1ndar y r W Blackdown PRIORY ROAD Service Stops B e t s a 5 h T e t 1 n e 1 (to Leamington & Whitnash) r c C r w 1 o n i A E T v a e 67 o 4 E H L Stirling Ave. i A L Kelvin St. E 15 A (to Stratford via Wellesbourne c B High w T R K e e Road l n k l n i s T B r o f U e t e o Av o o and Warwick Gates) n r r e e r t S T iv e n t d R n g e u R v i n T il n u n B o l i S (to Leamington) K e d w o D M e b L SQ a M v b a 664 E U o o to Southam O AR 16 A (to Hatton Park) d ld A u R R r C E O t T E (to Kenilworth) h 67 P A 69 a A E r C X17 D (to Warwick Hospital, R 664 v k H e l H o . -

Highway Maintenance Plan 2008/09 and Five Year List of Structural
Agenda No AGENDA MANAGEMENT SHEET Name of Committee Warwick Area Committee Date of Committee 10 March 2009 Report Title Highway Maintenance Plan 2009/10 and Five Year List of Structural Maintenance Schemes Summary The report provides information about highway maintenance work proposed in 2009/2010 and lists other sites where maintenance work will be required in the future. For further information Peter Samwell please contact County Highways Project Manager Tel. 01926 736530 [email protected] Would the recommended No decision be contrary to the Budget and Policy Framework? Background Papers None CONSULTATION ALREADY UNDERTAKEN:- Details to be specified Other Committees .......................................................................... Local Member(s) .......................................................................... (With brief comments, if appropriate) Other Elected Members .......................................................................... Cabinet Member .......................................................................... (Reports to The Cabinet, to be cleared with appropriate Cabinet Member) Chief Executive .......................................................................... Legal X I Marriott Finance .......................................................................... Areaw/0309/ww5 WA 1 of 7 Other Chief Officers .......................................................................... District Councils ......................................................................... -

Whitnash Town Council
NOTICE OF POLL Election of Town Councillors for Whitnash West Notice is hereby given that: 1. A poll for the election of Town Councillors for Whitnash West will be held on Thursday 7 May 2015, between the hours of 7:00 am and 10:00 pm. 2. The number of Town Councillors to be elected is four. 3. The names, home addresses and descriptions of the Candidates remaining validly nominated for election and the names of all persons signing the Candidates nomination paper are as follows: Names of Signatories Name of Candidate Home Address Description (if any) Proposers(+), Seconders(++) & Assentors ADAMS 11 Erica Drive, Whitnash Residents Stephen K McFadden Edel C McFadden (++) Nigel Paul Whitnash, Leamington Association (+) Spa, Warwickshire CLEMMEY 4 Ashford Gardens, Labour Party Anne M Chambers (+) Robert H Attwood (++) William David Whitnash, Leamington Spa, CV31 2NB HEATH 53 Whitnash Road, Whitnash Residents Stephen K McFadden Bernard Kirton (++) Tony Whitnash, CV31 2HF Association (+) MCFADDEN 2 Moorhill Road, Whitnash Residents Bernard Kirton (+) Edel C McFadden (++) Steve Whitnash, Association Warwickshire, CV31 2LG VAUGHAN 96 Heathcote Road, Whitnash Residents Edel C McFadden (+) Stephen K McFadden Steve Whitnash, CV31 2LY Association (++) 4. The situation of Polling Stations and the description of persons entitled to vote thereat are as follows: Station Ranges of electoral register numbers of Situation of Polling Station Number persons entitled to vote thereat Whitnash Sports and Social Club, Heathcote Road, Whitnash 116W WWH5-1 to WWH5-1077 Warwick Gates Community Centre STATION C, The Main Hall, 117W WWH6-1 to WWH6-1193/2 Cressida Close, Warwick 5. Where contested this poll is taken together with the election of District Councillors and the election of a Member of Parliament for the Warwick and Leamington Constituency. -

Strategic Housing Land Availability Assessment
LDF Evidence Base Strategic Housing Land Availability Assessment Site Assessments: Leamington & Whitnash May 2014 www.warwickdc.gov.uk Site Ref L01 Site Name Lime Avenue Site Size 0.37 Settlement Leamington Spa (Hectares) Source SHLAA 08 Land Type Previously developed Adjacent/ Overlapping Site Suitability for Housing Location Built up area Policy Restrictions None Physical Constraints Potential ground contamination Potential Impacts Adjacent to Lillington Village Conservation Area Environmental Satisfactory Conditions Overall Suitability Suitable Availability Owner has indicated that the site could become available by 2012 Achievability Achievable, subject to market. Housing Capacity Development Mix Housing 67% Other 33% Uses Potential Capacity 30dph 7 40dph 10 50dph 12 Timeframe (in terms 2014/19 10 2019/24 0 2024/29 0 of practicality only) 2 6 17 1 6 1 4 5 8 1 2 A 6 8 6 a 6 2 H 8 3 A D 1 R IA N L I C M L E O 9 A S V E E N U E 1 1 0 3 1 4 Pavilion Manor Farm House 2 3 0 Pavilion 1 4 2 8 5 Wickham 2 Court 9 6 3 1 7 4 Manor Farm 1 House 1 4 Hall 21 Garage 1 2 8 4 3 1 T H E 103 11 H O Club 9 L T 1 2 L IM 7 9 D E A A O V R E M N R U A E F 95 2 44 4 89 2 4 3 1 4 30 1 2 D 9 A 1 2 1 O 4 R 2 2 2 R 16 O N A C M lin ic 1 5 87 2 © Crown copyright and database rights [2011] Ordnance Survey 100018302. -

40 Heathcote Road, Whitnash, Leamington Spa, CV31 2NF Offers Over £290,000
40 Heathcote Road, Whitnash, Leamington Spa, CV31 2NF Offers Over £290,000 A spacious and attractive bay fronted traditional semi detached property set in the popular Whitnash, south Leamington Spa. The property is well maintained and proportioned throughout being within easy reach of the town centre, shops, amenities, schools and transport links. This would make a fantastic home for any families wishing to move up the property ladder. In brief the property comprises large living room, large second reception room, fitted kitchen, garage, lean to/utility, three well proportioned bedrooms, family bathroom, large driveway and good size garden to the rear. APPROACH Approached via the large driveway, good size fireplace, wall mounted lights and central heating radiator, TV GARAGE With up and over door, power and lighting and well maintained front garden with wall, hedge and fenced point and centrally mounted ceiling lights. housing the boiler. borders. DINING ROOM Another good size reception room with bay ON THE FIRST FLOOR ENTRANCE PORCH With obscured double glazed doors to window to the rear elevation, patio doors leading to the rear LANDING With double glazed window to the side elevation, the front elevation. garden, feature electric fireplace, TV point, central heating loft access and centrally mounted ceiling lighting radiator and two centrally mounted ceiling lights. ENTRANCE HALL With door to front with attractive original MASTER BEDROOM Having large double glazed bay stained glass leaded light windows, stairs ro the first floor, FITTED KITCHEN Fitted with a range of wall and base level window to the front elevation, large built in wardrobes, central central heating radiator and door leading to :- units, ceiling light, space for cooker, sink and drainer and door heating radiator and two ceiling lights.