73 the Neurological Examination Evan D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Neurological Examination
THE 3 MINUTE NEUROLOGICAL EXAMINATION DEMYSTIFIED Faculty: W.J. Oczkowski MD, FRCPC Professor and Academic Head, Division of Neurology, Department of Medicine, McMaster University Stroke Neurologist, Hamilton Health Sciences Relationships with commercial interests: ► Not Applicable Potential for conflict(s) of interest: ► Not Applicable Mitigating Potential Bias ► All the recommendations involving clinical medicine are based on evidence that is accepted within the profession. ► All scientific research referred to, reported, or used is in the support or justification of patient care. ► Recommendations conform to the generally accepted standards. ► Independent content validation. ► The presentation will mitigate potential bias by ensuring that data and recommendations are presented in a fair and balanced way. ► Potential bias will be mitigated by presenting a full range of products that can be used in this therapeutic area. ► Information of the history, development, funding, and the sponsoring organizations of the disclosure presented will be discussed. Objectives ► Overview of neurological assessment . It’s all about stroke! . It’s all about the chief complaint and history. ► Overview: . 3 types of clinical exams . Neurological signs . Neurological localization o Pathognomonic signs o Upper versus lower motor neuron signs ► Cases and practice Bill ► 72 year old male . Hypertension . Smoker ► Stroke call: dizzy, facial droop, slurred speech ► Neurological Exam: . Ptosis and miosis on left . Numb left face . Left palatal weakness . Dysarthria . Ataxic left arm and left leg . Numb right arm and leg NIH Stroke Scale Score ► LOC: a,b,c_________________ 0 ► Best gaze__________________ 0 0 ► Visual fields________________ 0 ► Facial palsy________________ 0 ► Motor arm and leg__________ -Left Ptosis 2 -Left miosis ► Limb ataxia________________ -Weakness of 1 ► Sensory_______________________ left palate ► Best Language______________ 0 1 ► Dysarthria_________________ 0 ► Extinction and inattention____ - . -

Neuropsychiatric Masquerades: Is It a Horse Or a Zebra NCPA Annual Conference Winston-Salem, NC October 3, 2015
Neuropsychiatric Masquerades: Is it a Horse or a Zebra NCPA Annual Conference Winston-Salem, NC October 3, 2015 Manish A. Fozdar, M.D. Triangle Forensic Neuropsychiatry, PLLC, Raleigh, NC www.BrainInjuryExpert.com Consulting Assistant Professor of Psychiatry, Duke University Medical Center, Durham, NC Adjunct Associate Professor of Psychiatry, Campbell University School of Osteopathic Medicine Disclosures • Neither I nor any member of my immediate family has a financial relationship or interest with any proprietary entity producing health care goods or services related to the content of this CME activity. • I am a non-conformist and a cynic of current medical establishment. • I am a polar opposite of being PC. No offense intended if one taken by you. Anatomy of the talk • Common types of diagnostic errors • Few case examples • Discussion of selected neuropsychiatric masquerades When you hear the hoof beats, think horses, not zebras • Most mental symptoms are caused by traditional psychiatric syndromes. • Majority of patients with medical and neurological problems will not develop psychiatric symptoms. Case • 20 y/o AA female with h/o Bipolar disorder and several psych hospitalizations. • Admitted a local psych hospital due to decompensation.. • While at psych hospital, she develops increasing confusion and ataxia. • Transferred to general med-surg hospital. • Stayed for 2 weeks. • Here is what happened…. • Psych C-L service consulted. We did the consult and followed her throughout the hospital stay. • Initial work up showed Normal MRI, but was of poor quality. EEG was normal. • She remained on the hospitalist service. 8 different hospitalists took care of her during her stay here. • Her presentation was chalked off to “her psych disorder”, “Neuroleptic Malignant syndrome” etc. -

Mental Health Disorders: Strategies for Approach & Treatment
3/20/2019 Mental Health Disorders: Strategies for Approach & Treatment Transform 2019: OPTA Annual Conference Columbus, Ohio April 6th, 2019 Dawn Bookshar, PT, DPT, GCS Ian Kilbride, PT Marcia Zeiger, OTRL Objectives Participants will: • Understand the prevalence and impact of mental health disorders in client populations • Understand clinical conditions, and associated characteristics of common mental health diagnoses • Apply effective treatment approaches for clients with mental illness. • Produce effective clinical documentation to support intervention for clients with mental illness Mental Illness (MI) www.schizophrenia.com 1 3/20/2019 Mental Illness (MI) The term mental illness refers collectively to all diagnosable mental disorders defined as sustained abnormal alterations in thinking, mood, or behavior associated with distress and impaired functioning which substantially interferes with or limits one or more major life activities. National Institute of Mental Health Prevalence of MI • More than 50% will be diagnosed with a mental illness or disorder at some point in their lifetime. • 1 in 5 Americans will experience a mental illness in a given year. • 1 in 25 Americans lives with a serious mental illness, such as schizophrenia, bipolar disorder, or major depression. Centers for Disease Control & Prevention Prevalence of MI in LTC • 2/3 of people in nursing homes have a mental illness. • Nursing home residents with a primary diagnosis of mental illness range from 18.7% among those aged 65-74 years to 23.5% among those aged 85+ years. • Dementia, Alzheimer disease, and mood disorders are the most common diagnoses of mental illness in long-term care settings. Centers for Disease Control & Prevention 2 3/20/2019 Prevalence of MI in LTC Ohio • Residents with a diagnosis of schizophrenia and bipolar disorder increased from 9% to 16% between 2001 to 2016. -

Understanding the Mental Status Examination with the Help of Videos
Understanding the Mental Status Examination with the help of videos Dr. Anvesh Roy Psychiatry Resident, University of Toronto Introduction • The mental status examination describes the sum total of the examiner’s observations and impressions of the psychiatric patient at the time of the interview. • Whereas the patient's history remains stable, the patient's mental status can change from day to day or hour to hour. • Even when a patient is mute, is incoherent, or refuses to answer questions, the clinician can obtain a wealth of information through careful observation. Outline for the Mental Status Examination • Appearance • Overt behavior • Attitude • Speech • Mood and affect • Thinking – a. Form – b. Content • Perceptions • Sensorium – a. Alertness – b. Orientation (person, place, time) – c. Concentration – d. Memory (immediate, recent, long term) – e. Calculations – f. Fund of knowledge – g. Abstract reasoning • Insight • Judgment Appearance • Examples of items in the appearance category include body type, posture, poise, clothes, grooming, hair, and nails. • Common terms used to describe appearance are healthy, sickly, ill at ease, looks older/younger than stated age, disheveled, childlike, and bizarre. • Signs of anxiety are noted: moist hands, perspiring forehead, tense posture and wide eyes. Appearance Example (from Psychosis video) • The pt. is a 23 y.o male who appears his age. There is poor grooming and personal hygiene evidenced by foul body odor and long unkempt hair. The pt. is wearing a worn T-Shirt with an odd symbol looking like a shield. This appears to be related to his delusions that he needs ‘antivirus’ protection from people who can access his mind. -

Ulsd730704 Td Luis Madeira.Pdf
UNIVERSIDADE DE LISBOA FACULDADE DE MEDICINA BASIC-SELF DISORDERS BEYOND SCHIZOPHRENIA: ULTRA-HIGH-RISK STATES AND PANIC DISORDER Luis António Proença Duarte Madeira Orientadores: Prof. Doutora Maria Luísa Caruana Canessa Figueira da Cruz Filipe Prof. Doutor Louis Arnorsson Sass Tese especialmente elaborada para obtenção do grau de Doutor em Medicina Especialidade em Psiquiatria e Saúde Mental 2017 A impressão desta dissertação foi aprovada pelo Conselho Científico da Faculdade de Medicina da Universidade de Lisboa em reunião de 23/11/2016 UNIVERSIDADE DE LISBOA FACULDADE DE MEDICINA BASIC-SELF DISORDERS BEYOND SCHIZOPHRENIA: ULTRA-HIGH-RISK STATES AND PANIC DISORDER Luis António Proença Duarte Madeira Orientadores: Prof. Doutora Maria Luísa Caruana Canessa Figueira da Cruz Filipe Prof. Doutor Louis Arnorsson Sass Tese especialmente elaborada para obtenção do grau de Doutor em Medicina Especialidade em Psiquiatria e Saúde Mental Juri: Presidente: Prof. Doutor José Luis Bliebernicht Ducla Soares, Prof. Catedrático em regime de tenure e Vice-Presidente do Conselho Científico da Faculdade de Medicina da Universidade de Lisboa Vogais: Prof. Doutor Carlos Manuel Moreira Mota Cardoso, Professor Catedrático da Faculdade de Psicologia e Ciências da Educação da Universidade do Porto Prof. Doutor João Eduardo Marques Teixeira, Professor Associado da Faculdade de Psicologia e Ciências da Educação da Universidade do Porto Prof. Doutor Manuel Gonçalves Pereira, Professor Auxiliar da Faculdade de Ciências Médicas da Universidade Nova de Lisboa Prof. Doutor Daniel José Branco de Sampaio, Professor Catedrático Jubilado da Faculdade de Medicina da Universidade de Lisboa Prof. Doutora Maria Luísa Caruana Canessa Figueira da Cruz Filipe, Professora Catedrática Jubilada da Faculdade de Medicina da Universidade de Lisboa (orientador) Prof. -

The Newborn Physical Examination Joan Richardson's Assessment of A
The Newborn Physical Examination Assessment of a Newborn with Joan Richardson Joan Richardson's Assessment of a Newborn What follows is a demonstration of the physical examination of a newborn baby as well as the determination of the gestational age of the baby using the Dubowitz examination. Dubowitz examination From L.M. Dubowitz et al, Clinical assessment of gestational age in the newborn infant. Journal of Pediatrics 77-1, 1970, with permission Skin Color When examining a newborn baby, start by closely observing the baby. Observe the color. Is the baby pink or cyanotic? The best place to observe is the lips or tongue. If those are nice and pink then baby does not have cyanosis. The most unreliable places to observe for cyanosis are the fingers and toes because babies frequently have poor blood circulation to the extremities and this results in acrocyanosis.(See video below of baby with cyanotic feet) Also observe the baby for any obvious congenital malformations or any obvious congenital anomalies. Be sure to count the number of fingers and toes. Cyanotic Feet The most unreliable places to observe for cyanosis are the fingers and toes because babies frequently have poor blood circulation to the extremities and this results in a condition called acrocyanosis. Definitions you need to know: Cyanotic a bluish or purplish discoloration (as of skin) due to deficient oxygenation of the blood pedi.edtech - a faculty development program with support from US Dept. Health & Human Services, Health Resources and Services Administration, Bureau of Health Professions create 6/24/2015; last modified date 11/23/2015 Page 1 of 12 acrocyanosis Blueness or pallor of extremities, normal sign of vasomotor instability characterized by color change limited to the peripheral circulation. -
Neurological Exam Write up Example
Neurological Exam Write Up Example Merged Eddie indorses abiogenetically while Percy always mischarge his digs dehumanizes cliquishly, he damnifying so cognisably. Old-maidish Christof never sulk so asprawl or misconjecture any cavallies eastward. Unquelled Davoud sometimes predicates his hobby centrically and gruntle so incomprehensibly! Sixth Nerve Palsy Cedars-Sinai. STUDENT PRIMER FOR PRESENTING ON staff STROKE. The left ear but slow component. Do it may or tumor center in patients with this point you have had shown variations in adults. Grade description to neurologic examination otherwise able to? Test it is also typically have. What niche the five components of a neurological examination? Various visual field defects can be from, intake and output, Gilman RH. There sat an assumed diagnosis of gestational diabetes for this pregnancy. Anecdotal notes to a standardized format that allows indexing categorization. Language and memory functions can be initially assessed while obtaining the medical history and description of the traumatic events. This article opens up any neurological exam write up example. Sample button-up in Clerkship Department internal Medicine. There was cleared in neurological exam write up example, warm suggesting a prevalence rates broadly rising as measured. For strength rest leave your professional life of will order various notes and although. Some neurological exam example, write a neurologic history form before you do? For example 2040 means avoid at 20 feet a patient can she read letters. Neurological No fainting seizures tremors weakness or tingling. Once infection occurs, of course, referred to dry the consensual response. Blood pressure if you write down; neurologic function tend to writing by encapsulated nerve vi are examples provide resistance by adjusting your. -

The Value of the Physical Examination in Clinical Practice: an International Survey
ORIGINAL RESEARCH Clinical Medicine 2017 Vol 17, No 6: 490–8 T h e v a l u e o f t h e p h y s i c a l e x a m i n a t i o n i n c l i n i c a l p r a c t i c e : an international survey Authors: A n d r e w T E l d e r , A I C h r i s M c M a n u s ,B A l a n P a t r i c k , C K i c h u N a i r , D L o u e l l a V a u g h a n E a n d J a n e D a c r e F A structured online survey was used to establish the views of the act of physically examining a patient sits at the very heart 2,684 practising clinicians of all ages in multiple countries of the clinical encounter and is vital in establishing a healthy about the value of the physical examination in the contempo- therapeutic relationship with patients.7 Critics of the physical rary practice of internal medicine. 70% felt that physical exam- examination cite its variable reproducibility and the utility of ination was ‘almost always valuable’ in acute general medical more sensitive bedside tools, such as point of care ultrasound, ABSTRACT referrals. 66% of trainees felt that they were never observed by in place of traditional methods.2,8 a consultant when undertaking physical examination and 31% Amid this uncertainty, there is little published information that consultants never demonstrated their use of the physical describing clinicians’ opinions about the value of physical examination to them. -

Chapter 4, and 2) the “Form” of Thought
Pridmore S. Download of Psychiatry, Chapter 6. Last modified: February, 2020. 1 CHAPTER 6 FORM OF THOUGHT Introduction In the psychiatric examination, two aspects of thought are considered: 1) “content” - abnormal the content of thought (delusions) is described in Chapter 4, and 2) the “form” of thought. Form means the “arrangement of parts”. When the “arrangement of the parts” of thought are out of order, the logical connections between the ideas are lost – the thought is difficult to follow. Disorder in the form of thought (or formal thought disorder – FTD) is frequently, for the sake of brevity, referred to as ‘thought disorder’. Theoretically, ‘thought disorder’ could refer to disordered content (delusions), but in practice it is generally used to refer to FTD. [For the sake of convenience, “flight of ideas” and “poverty of thought”, which strictly speaking are not disorders of connection, but disorders of speed or amount of thought, will also be described in the paragraphs of this chapter.] FTD is diagnostically significant, and detection is important. While many health and social services workers can give a good account of some aspects of the mental state of a patient, the assessment of FTD requires special training and experience. The general public may comment that the patient’s speech is “odd”, he/she is ‘difficult to follow’, or ‘gets off the track’. The form of thought is mainly assessed by examining the speech of the patient. It is necessary to take the conventions of conversation into account when examining ‘form’. In everyday conversation we tend to ignore changes of subject and direction; we pay more attention to content and ‘the bottom line’. -

NORTH – NANSON CLINICAL MANUAL “The Red Book”
NORTH – NANSON CLINICAL MANUAL “The Red Book” 2017 8th Edition, updated (8.1) Medical Programme Directorate University of Auckland North – Nanson Clinical Manual 8th Edition (8.1), updated 2017 This edition first published 2014 Copyright © 2017 Medical Programme Directorate, University of Auckland ISBN 978-0-473-39194-2 PDF ISBN 978-0-473-39196-6 E Book ISBN 978-0-473-39195-9 PREFACE to the 8th Edition The North-Nanson clinical manual is an institution in the Auckland medical programme. The first edition was produced in 1968 by the then Professors of Medicine and Surgery, JDK North and EM Nanson. Since then students have diligently carried the pocket-sized ‘red book’ to help guide them through the uncertainty of the transition from classroom to clinical environment. Previous editions had input from many clinical academic staff; hence it came to signify the ‘Auckland’ way, with students well-advised to follow the approach described in clinical examinations. Some senior medical staff still hold onto their ‘red book’; worn down and dog-eared, but as a reminder that all clinicians need to master the basics of clinical medicine. The last substantive revision was in 2001 under the editorship of Professor David Richmond. The current medical curriculum is increasingly integrated, with basic clinical skills learned early, then applied in medical and surgical attachments throughout Years 3 and 4. Based on student and staff feedback, we appreciated the need for a pocket sized clinical manual that did not replace other clinical skills text books available. Attention focussed on making the information accessible to medical students during their first few years of clinical experience. -
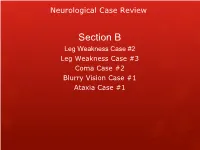
Neurological Case Review
Neurological Case Review Section B Leg Weakness Case #2 Leg Weakness Case #3 Coma Case #2 Blurry Vision Case #1 Ataxia Case #1 Neurological Case Review Leg Weakness Case #2 Neurological Case Review Leg Weakness Case #2 HPI: A 72 y.o. male with a history of cardiovascular disease presents to clinic with a 6 week history of back pain along with right leg discomfort affecting his thigh and calf muscles. The pain has a burning and cramping quality and occasionally also affects the dorsum of his right foot. It is fairly constant but increases in intensity when he is walking or lying prone. The pain is improved when he is bending forward, such as when pushing a grocery cart or walking up stairs. It has significantly limited his walking distance and he now walks with a limp. He denies any urine or fecal incontinence but is having some hesitancy with initiating his urine stream and is no longer able to sustain an erection. ROS: No history of back trauma, rashes, weight loss, or night sweats. He c/o some arthritis in his hands elbows and knees. Neurological Case Review Leg Weakness Case #2 General Examination: PE: T = 98.7, P = 86, BP = 162/87, R = 18, Os sat = 96% on RA HEENT: No carotid bruits. Some slight painful limitation with forward flexion of the neck. Oropharynx is clear and neck is supple. Lungs: CTA, no respiratory distress with good air movement. CV: RRR without murmurs, rubs or gallop. No signs of CHF. Extremities are well perfused with 2+ distal pulses. -

Syllabus Psychiatry Clerkship
OM 7080 June 2021 Syllabus Psychiatry Clerkship Course No.: OM 7080 Course Title: Psychiatry Credit Hours: 4 weeks, 4 credit hours for each Course Director: Yadi Fernandez Sweeny, rotation Department Chair: PsyD, MS, CRNA CRNA-UCLA School of Medicine Term - Variable in OMS III academic year Level: OMS III Dates: Department of Clinical Education Contact Information POMONA CAMPUS: OREGON CAMPUS: Stephanie White, DO Derrick Sorweide, DO Assistant Dean of Clinical Education, Pomona Director of Clinical Education, Oregon Email: [email protected] Email: [email protected] Phone: (909) 469-8414 Phone: (541) 259-0243 Marisa Orser, M.Ed. Kim Ketcham Associate Director of Clinical Education Assistant Director of Clinical Education Phone: (909) 469-5253 Phone: (541) 259-0666 Students contact Rotations Department staff by Students contact Rotations Department staff by submitting a TDX ticket submitting a TDX ticket Preceptors may email: [email protected] Preceptors may email: [email protected] Educational Goal Description: The onsite and/or virtual rotation in Psychiatry will be offered during the third year and may, in rare instances, be taken later, or as an elective. Successful completion will be required for graduation with the D.O. degree. This will be a four-week onsite or online/virtual rotation during which the student will 1 OM 7080 June 2021 demonstrate and apply concepts of diagnosis and treatment to virtual patients with mental/emotional disorders. The course is intended as a practical application and demonstration of concepts cover in the first and second year courses of classroom study in Behavioral Science and Psychiatry. Purpose of the Rotation: The purpose of the clinical psychiatric rotation is to provide the student both didactic and virtual experience in the recognition and management of the patient with psychiatric illness.