Understanding the Mental Status Examination with the Help of Videos
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
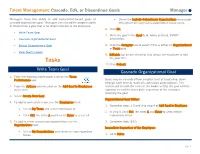
Manager Cascade, Edit, Or Discontinue Goal(S) in Workday
Talent Management: Cascade, Edit, or Discontinue Goals Manager Managers have the ability to add department-based goals or • Check the Include Subordinate Organizations to cascade cascade organization goal. Managers can also edit in-progress goals throughout all supervisory organization below yours. or discontinue a goal that is no longer relevant to the employee. 6. Click OK. • Write Team Goal 7. Write the goal in the Goal field. Add a detailed, SMART • Cascade Organizational Goal description. • Edit or Discontinue a Goal 8. Click the Category box to select if this is either an Organizational or Team goal. • View Team’s Goals 9. Editable will be pre-selected. This allows the employee to edit Tasks the goal title. 10. Click Submit. Write Team Goal Cascade Organizational Goal 1. From the Workday home page, click on the Team Performance app. Goals may be cascaded from a higher level of leadership, down through each level to reach all supervisory organizations. This 2. From the Actions column, click on the Add Goal to Employees section will include the steps of the leader writing the goal and the menu item. approval step of the immediate supervisor of the employee receiving the goal. 3. Select Create New Goal. Organizational Goal Writer: 4. To add to immediate team, use the Employees field: 1. Complete steps 1-3 and skip step 4 of Add Goal to Employee. • Select My Team and select individuals or 2. In step 5, click Ctrl, the letter A and Enter to select entire • Click Ctrl, the letter A and then hit Enter to select all. -

Social Norms and Social Influence Mcdonald and Crandall 149
Available online at www.sciencedirect.com ScienceDirect Social norms and social influence Rachel I McDonald and Christian S Crandall Psychology has a long history of demonstrating the power and and their imitation is not enough to implicate social reach of social norms; they can hardly be overestimated. To norms. Imitation is common enough in many forms of demonstrate their enduring influence on a broad range of social life — what creates the foundation for culture and society phenomena, we describe two fields where research continues is not the imitation, but the expectation of others for when to highlight the power of social norms: prejudice and energy imitation is appropriate, and when it is not. use. The prejudices that people report map almost perfectly onto what is socially appropriate, likewise, people adjust their A social norm is an expectation about appropriate behav- energy use to be more in line with their neighbors. We review ior that occurs in a group context. Sherif and Sherif [8] say new approaches examining the effects of norms stemming that social norms are ‘formed in group situations and from multiple groups, and utilizing normative referents to shift subsequently serve as standards for the individual’s per- behaviors in social networks. Though the focus of less research ception and judgment when he [sic] is not in the group in recent years, our review highlights the fundamental influence situation. The individual’s major social attitudes are of social norms on social behavior. formed in relation to group norms (pp. 202–203).’ Social norms, or group norms, are ‘regularities in attitudes and Address behavior that characterize a social group and differentiate Department of Psychology, University of Kansas, Lawrence, KS 66045, it from other social groups’ [9 ] (p. -

Teacher Training: Learning to Be Instigators of Thought™ Through a Process Aligned with Inspired Teaching's Educational Phil
Transforming education through innovation teacher training Teacher Training: Learning to be Instigators of Thought™ Through a process aligned with Inspired Teaching’s educational philosophy – which engages participants intellectually, physically, and emotionally - Inspired Teaching trains teachers to design and implement rigorous, student-centered lessons and activities that meet student needs and academic standards, including the Common Core State Standards. Like the teaching process itself, our teacher training is complex and allows for customization to meet the specific needs of each teacher. This audience-sensitivity creates a permanent shift in teachers’ thinking about their jobs and is one of the key reasons our process is so effective. Inspired Teaching’s Five Step Process for Teacher Education Each teacher navigates the following process: Step 1. Analyze and deepen my understanding of the ways I learn through a rigorous examination of the teaching and learning process, including my including my own experiences as a child and adult learner. Step 2. Articulate and defend my philosophy of teaching and learning , including what I believe about children. Challenge myself to listen to and consider other points of view and to find room in my philosophy for an appreciation of children's natural curiosity and innate desire to learn. Step 3. Make the connection to classroom practice , analyzing my current instructional strategies and whether they support my philosophy, so that I can explore and develop new ways to make sure what I do in the classroom matches my philosophy of teaching and learning. Step 4. Build the skills of effective teachers , including active listening, asking questions that will spark students' intellect and imaginations, observing to assess for student understanding, and communicating effectively. -

Personal Goals, Life Meaning, and Virtue: Wellsprings of a Positive Life
5 PERSONAL GOALS, LIFE MEANING, AND VIRTUE: WELLSPRINGS OF A POSITIVE LIFE ROBERT A. EMMONS Nothing is so insufferable to man as to be completely at rest, without passions, without business, without diversion, without effort. Then he feels his nothingness, his forlornness, his insufficiency, his weakness, his emptiness. (Pascal, The Pensees, 1660/1950, p. 57). As far as we know humans are the only meaning-seeking species on the planet. Meaning-making is an activity that is distinctly human, a function of how the human brain is organized. The many ways in which humans conceptualize, create, and search for meaning has become a recent focus of behavioral science research on quality of life and subjective well-being. This chapter will review the recent literature on meaning-making in the context of personal goals and life purpose. My intention will be to document how meaningful living, expressed as the pursuit of personally significant goals, contributes to positive experience and to a positive life. THE CENTRALITY OF GOALS IN HUMAN FUNCTIONING Since the mid-1980s, considerable progress has been made in under- standing how goals contribute to long-term levels of well-being. Goals have been identified as key integrative and analytic units in the study of human Preparation of this chapter was supported by a grant from the John Templeton Foundation. I would like to express my gratitude to Corey Lee Keyes and Jon Haidt for the helpful comments on an earlier draft of this chapter. 105 motivation (see Austin & Vancouver, 1996; Karoly, 1999, for reviews). The driving concern has been to understand how personal goals are related to long-term levels of happiness and life satisfaction and how ultimately to use this knowledge in a way that might optimize human well- being. -

Descartes' Influence in Shaping the Modern World-View
R ené Descartes (1596-1650) is generally regarded as the “father of modern philosophy.” He stands as one of the most important figures in Western intellectual history. His work in mathematics and his writings on science proved to be foundational for further development in these fields. Our understanding of “scientific method” can be traced back to the work of Francis Bacon and to Descartes’ Discourse on Method. His groundbreaking approach to philosophy in his Meditations on First Philosophy determine the course of subsequent philosophy. The very problems with which much of modern philosophy has been primarily concerned arise only as a consequence of Descartes’thought. Descartes’ philosophy must be understood in the context of his times. The Medieval world was in the process of disintegration. The authoritarianism that had dominated the Medieval period was called into question by the rise of the Protestant revolt and advances in the development of science. Martin Luther’s emphasis that salvation was a matter of “faith” and not “works” undermined papal authority in asserting that each individual has a channel to God. The Copernican revolution undermined the authority of the Catholic Church in directly contradicting the established church doctrine of a geocentric universe. The rise of the sciences directly challenged the Church and seemed to put science and religion in opposition. A mathematician and scientist as well as a devout Catholic, Descartes was concerned primarily with establishing certain foundations for science and philosophy, and yet also with bridging the gap between the “new science” and religion. Descartes’ Influence in Shaping the Modern World-View 1) Descartes’ disbelief in authoritarianism: Descartes’ belief that all individuals possess the “natural light of reason,” the belief that each individual has the capacity for the discovery of truth, undermined Roman Catholic authoritarianism. -

The Hierarchically Mechanistic Mind: a Free-Energy Formulation of the Human Psyche
JID:PLREV AID:1045 /REV [m3SC+; v1.294; Prn:28/01/2019; 9:15] P.1(1-18) Available online at www.sciencedirect.com ScienceDirect Physics of Life Reviews ••• (••••) •••–••• www.elsevier.com/locate/plrev Review The hierarchically mechanistic mind: A free-energy formulation of the human psyche ∗ Paul B. Badcock a,b,c, , Karl J. Friston d, Maxwell J.D. Ramstead d,e,f a Centre for Youth Mental Health, The University of Melbourne, Melbourne, 3052, Australia b Melbourne School of Psychological Sciences, The University of Melbourne, Melbourne, 3010, Australia c Orygen, the National Centre of Excellence in Youth Mental Health, Melbourne, 3052, Australia d Wellcome Trust Centre for Neuroimaging, University College London, London, WC1N3BG, UK e Department of Philosophy, McGill University, Montreal, Quebec, H3A 2T7, Canada f Division of Social and Transcultural Psychiatry, Department of Psychiatry, McGill University, Montreal, Quebec, H3A 1A1, Canada Communicated by Prod Felix Schoeller Abstract This article presents a unifying theory of the embodied, situated human brain called the Hierarchically Mechanistic Mind (HMM). The HMM describes the brain as a complex adaptive system that actively minimises the decay of our sensory and physical states by producing self-fulfilling action-perception cycles via dynamical interactions between hierarchically organised neurocog- nitive mechanisms. This theory synthesises the free-energy principle (FEP) in neuroscience with an evolutionary systems theory of psychology that explains our brains, minds, and behaviour by appealing to Tinbergen’s four questions: adaptation, phylogeny, on- togeny, and mechanism. After leveraging the FEP to formally define the HMM across different spatiotemporal scales, we conclude by exploring its implications for theorising and research in the sciences of the mind and behaviour. -

Neuropsychiatric Masquerades: Is It a Horse Or a Zebra NCPA Annual Conference Winston-Salem, NC October 3, 2015
Neuropsychiatric Masquerades: Is it a Horse or a Zebra NCPA Annual Conference Winston-Salem, NC October 3, 2015 Manish A. Fozdar, M.D. Triangle Forensic Neuropsychiatry, PLLC, Raleigh, NC www.BrainInjuryExpert.com Consulting Assistant Professor of Psychiatry, Duke University Medical Center, Durham, NC Adjunct Associate Professor of Psychiatry, Campbell University School of Osteopathic Medicine Disclosures • Neither I nor any member of my immediate family has a financial relationship or interest with any proprietary entity producing health care goods or services related to the content of this CME activity. • I am a non-conformist and a cynic of current medical establishment. • I am a polar opposite of being PC. No offense intended if one taken by you. Anatomy of the talk • Common types of diagnostic errors • Few case examples • Discussion of selected neuropsychiatric masquerades When you hear the hoof beats, think horses, not zebras • Most mental symptoms are caused by traditional psychiatric syndromes. • Majority of patients with medical and neurological problems will not develop psychiatric symptoms. Case • 20 y/o AA female with h/o Bipolar disorder and several psych hospitalizations. • Admitted a local psych hospital due to decompensation.. • While at psych hospital, she develops increasing confusion and ataxia. • Transferred to general med-surg hospital. • Stayed for 2 weeks. • Here is what happened…. • Psych C-L service consulted. We did the consult and followed her throughout the hospital stay. • Initial work up showed Normal MRI, but was of poor quality. EEG was normal. • She remained on the hospitalist service. 8 different hospitalists took care of her during her stay here. • Her presentation was chalked off to “her psych disorder”, “Neuroleptic Malignant syndrome” etc. -

Delirium: Presentation, Epidemiology, and Diagnostic Evaluation (Part 1)
IDENTIFYING AND MANAGING PSYCHIATRIC EMERGENCIES Delirium: Presentation, Epidemiology, and Diagnostic Evaluation (Part 1) COLIN J. HARRINGTON, MD; KALYA VARDI, MD 18 23 EN ABSTRACT state, acute brain dysfunction, acute brain failure, acute Delirium is a highly prevalent and complex neuro- organic brain syndrome, ICU psychosis, and metabolic en- psychiatric disorder marked by attentional dysfunction, cephalopathy, amongst others. The term delirium is derived disturbances in multiple cognitive domains, and changes from the Latin roots de (translated “away from”) and lira in motor behavior, perception, sleep, and thought pro- (translated “furrow of a field”) thus suggesting that one is cess. Delirium results from diverse toxic, metabolic, in- derailed from the plowed or straight path.11 fectious, and structural etiologies and is associated with The term encephalopathy is often employed in place of or a number of adverse outcomes. Delirium pathophysiol- alongside delirium and allows for the proper grouping togeth- ogy involves perturbation of multiple neurotransmitter er of delirium and dementia as cognitive disorders – while systems. Behavioral presentations of delirium are com- also providing for the longitudinal course-based distinction mon and are often misattributed to primary psychiatric between delirium and dementia, as acute and reversible, and processes. Diagnostic assessment of delirium includes chronic and progressive forms of encephalopathy, respec- thorough physical examination, careful cognitive test- tively. Use of this terminology also allows for description ing, appropriate metabolic and infectious studies, re- of the intermediate syndrome of sub-acute encephalopathy view of medications, and structural brain imaging and where cognitive dysfunction is often less obvious and electroencephalography as indicated. Pharmacologic and neuropsychiatric symptoms predominate. -
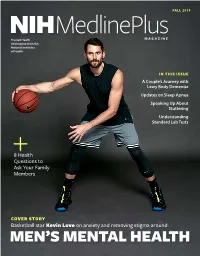
Mlpmfall19.Pdf
FALL 2019 MedlinePlus NIH MAGAZINE Trusted Health Information from the National Institutes of Health IN THIS ISSUE A Couple’s Journey with Lewy Body Dementia Updates on Sleep Apnea Speaking Up About Stuttering Understanding Standard Lab Tests 8 Health Questions to Ask Your Family Members COVER STORY Basketball star Kevin Love on anxiety and removing stigma around MEN’S MENTAL HEALTH In this issue id you know that more than 31% of U.S. adults experience an anxiety disorder at some point Din their lives, according to the National Institute of Mental Health (NIMH)? For our fall issue cover feature, Cleveland Cavaliers basketball player Kevin Love opens up about his own struggles with anxiety and his path to managing the condition. He talks about the special challenges facing men with mental health conditions and explains what he’s doing to combat that stigma as an athlete and advocate. We also spoke with the National Basketball Players Association’s Mental William Parham, Ph.D. (center) is the first-ever director of the National Basketball Players Association’s Mental Health Program. Also pictured Health Program Director William Parham, are Antonio Davis, Keyon Dooling, Michele Roberts, Garrett Temple, Ph.D., about their new program to help and Chris Paul. players stay healthy both on and off the court and with leading researchers from NIMH to get the latest, need-to-know Finally, as you gather with loved ones this information on anxiety conditions. season, make sure to take a look at our helpful Also in this issue, we provide research updates list of health questions to ask your family. -

Attitudes Toward Emotions
Journal of Personality and Social Psychology © 2011 American Psychological Association 2011, Vol. 101, No. 6, 1332–1350 0022-3514/11/$12.00 DOI: 10.1037/a0024951 Attitudes Toward Emotions Eddie Harmon-Jones and Cindy Harmon-Jones David M. Amodio Texas A&M University New York University Philip A. Gable University of Alabama The present work outlines a theory of attitudes toward emotions, provides a measure of attitudes toward emotions, and then tests several predictions concerning relationships between attitudes toward specific emotions and emotional situation selection, emotional traits, emotional reactivity, and emotion regula- tion. The present conceptualization of individual differences in attitudes toward emotions focuses on specific emotions and presents data indicating that 5 emotions (anger, sadness, joy, fear, and disgust) load on 5 separate attitude factors (Study 1). Attitudes toward emotions predicted emotional situation selection (Study 2). Moreover, attitudes toward approach emotions (e.g., anger, joy) correlated directly with the associated trait emotions, whereas attitudes toward withdrawal emotions (fear, disgust) correlated inversely with associated trait emotions (Study 3). Similar results occurred when attitudes toward emotions were used to predict state emotional reactivity (Study 4). Finally, attitudes toward emotions predicted specific forms of emotion regulation (Study 5). Keywords: discrete emotions, approach motivation, withdrawal motivation, emotion regulation, behav- ioral activation system (BAS) Emotions pervade subjective experience (Izard, 2009), and al- theory by assessing relationships between attitudes toward specific though often perceived as a single subjective state, emotional emotions and emotional traits, emotional reactivity, emotional experience is likely composed of many different elements. Tom- situation selection, and emotion regulation. kins (1962, 1963) and others (Ellsworth, 1994; Izard, 1971) sug- gested that the evaluation of an emotion is part of the experience of emotion. -

Mental Health Disorders: Strategies for Approach & Treatment
3/20/2019 Mental Health Disorders: Strategies for Approach & Treatment Transform 2019: OPTA Annual Conference Columbus, Ohio April 6th, 2019 Dawn Bookshar, PT, DPT, GCS Ian Kilbride, PT Marcia Zeiger, OTRL Objectives Participants will: • Understand the prevalence and impact of mental health disorders in client populations • Understand clinical conditions, and associated characteristics of common mental health diagnoses • Apply effective treatment approaches for clients with mental illness. • Produce effective clinical documentation to support intervention for clients with mental illness Mental Illness (MI) www.schizophrenia.com 1 3/20/2019 Mental Illness (MI) The term mental illness refers collectively to all diagnosable mental disorders defined as sustained abnormal alterations in thinking, mood, or behavior associated with distress and impaired functioning which substantially interferes with or limits one or more major life activities. National Institute of Mental Health Prevalence of MI • More than 50% will be diagnosed with a mental illness or disorder at some point in their lifetime. • 1 in 5 Americans will experience a mental illness in a given year. • 1 in 25 Americans lives with a serious mental illness, such as schizophrenia, bipolar disorder, or major depression. Centers for Disease Control & Prevention Prevalence of MI in LTC • 2/3 of people in nursing homes have a mental illness. • Nursing home residents with a primary diagnosis of mental illness range from 18.7% among those aged 65-74 years to 23.5% among those aged 85+ years. • Dementia, Alzheimer disease, and mood disorders are the most common diagnoses of mental illness in long-term care settings. Centers for Disease Control & Prevention 2 3/20/2019 Prevalence of MI in LTC Ohio • Residents with a diagnosis of schizophrenia and bipolar disorder increased from 9% to 16% between 2001 to 2016. -

Depression and Anxiety: a Review
DEPRESSION AND ANXIETY: A REVIEW Clifton Titcomb, MD OTR Medical Consultant Medical Director Hannover Life Reassurance Company of America Denver, CO [email protected] epression and anxiety are common problems Executive Summary This article reviews the in the population and are frequently encoun- overall spectrum of depressive and anxiety disor- tered in the underwriting environment. What D ders including major depressive disorder, chronic makes these conditions diffi cult to evaluate is the wide depression, minor depression, dysthymia and the range of fi ndings associated with the conditions and variety of anxiety disorders, with some special at- the signifi cant number of comorbid factors that come tention to post-traumatic stress disorder (PTSD). into play in assessing the mortality risk associated It includes a review of the epidemiology and risk with them. Thus, more than with many other medical factors for each condition. Some of the rating conditions, there is a true “art” to evaluating the risk scales that can be used to assess the severity of associated with anxiety and depression. Underwriters depression are discussed. The various forms of really need to understand and synthesize all of the therapy for depression are reviewed, including key elements contributing to outcomes and develop the overall therapeutic philosophy, rationale a composite picture for each individual to adequately for the choice of different medications, the usual assess the mortality risk. duration of treatment, causes for resistance to therapy, and the alternative approaches that The Spectrum of Depression may be employed in those situations where re- Depression represents a spectrum from dysthymia to sistance occurs.