Hospital Outpatient Fee Schedule (HOFS)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Taylor Corporation Companies: U.S. Manufacturing Locations \ 507-625-2828 \ [email protected]
Taylor Corporation Companies: U.S. Manufacturing Locations www.taylorcorp.com \ 507-625-2828 \ [email protected] AMSTERDAM, NY Amsterdam Printing and Litho QUEENSBURY, NY PORTLAND, OR MINNESOTA Web Graphics PhotoCraft, Inc. {See Inset} CINCINNATI, OH Western Graphics & Data Garvey Products COLUMBIA, NJ Navitor Specialty Products REXBURG, ID COLUMBUS, OH Artco Vectra HARWOOD HEIGHTS, IL SAN FRANCISCO, CA MECHANICSBURG, PA The Ligature Cosco Industries/Navitor Complyright Distribution Services LAS VEGAS, NV BOULDER, CO WAYNESBORO, PA Nevada Color Litho Lifepics 123Print Los Angeles, CA FENTON, MO Cosco/Navitor BurdgeCooper Drawing Board Optima Graphics SUNMAN, IN OXNARD, CA COLORADO SPRINGS, CO McPhersons Complyright Distribution Services Current Paper Direct BLOOMINGTON, IL ALTO, GA ALEXANDRIA, VA VERNON, CA Cosco Industries/Navitor Navitor Marketing General Progressive Impressions The Ligature DULUTH, GA Original Smith Printing BALDWIN PARK, CA Curtis 1000 Corporate Graphics DALLAS, TX International REDLANDS, CA CardsDirect Curtis 1000 Virtual Images Venture Solutions WACO, TX Unlimited Tatex NEW BRIGHTON, MN LAKE MARY, FL Print Craft ARDEN HILLS, MN HOUSTON, TX Progressive Communications Venture Solutions Complyright Distribution Services MINNEAPOLIS, MN HUGO, MN POMPANO BEACH Heinrich Envelope Ad Graphics Progressive Impressions Red Stamp Curtis 1000 SUNRISE, FL International Everglades Direct BLOOMINGTON, MN WHITE BEAR LAKE, MN Flexo Impression Taylor Strategic Accounts Litho Tech/Custom Cover Taymark SAVAGE, MN INVER GROVE HEIGHTS, MN Travel Tags Flexo Impressions Soligie BYRON, MN Schmidt Printing NORTH MANKATO, MN Card Fulfillment Services MANKATO, MN Carlson Craft National Recognition Products Corporate Graphics International Thayer Publishing Corporate Graphics Commercial Cosco Fine Impressions LabelWorks Navitor NowDocs Pear Tree Greetings Precision Press Taylor Corporation Taylor Corporation Companies: International Manufacturing Locations www.taylorcorp.com \ 507-625-2828 \ [email protected] CANADA CCA Occasions, Ltd. -

Inspiring and Preparing Young People for Success
Inspiring and preparing young people for success 2017-2018 Mission Report Nathan Ziegler, principal of Hope Academy, and his students. Read his JA story on page 14. Dear Friends, As we reflect on this past year, we’re energized by what we’ve accomplished thanks to your investment. Junior Achievement has experienced incredible growth, innovation, and success. We’ve impacted more students, joined with more educators and schools, and partnered with more volunteers. We’ve piloted two new programs — JA Inspire and JA Meda Fellows — to equip students with the skills needed to succeed in the workforce and start a business. We inspired the creation of 74 student-run companies through JA Company Program, an increase of 23% over last year. We’re always looking for new ways to motivate young people to envision a successful future and to gain the skills needed to be contributing members of our community. Our partners are instrumental in keeping us relevant, innovative, and engaging! Today’s youth are our future; their success is our success. As we look forward, we’re excited by what’s ahead. In 2019, Junior Achievement will celebrate its 100th year. Very few organizations make it to 100 years, much less continue to grow and thrive as Junior Achievement has. Celebrate with us – watch our centennial video at https://youtu.be/fKAvHJ9vcek. Locally, Junior Achievement of the Upper Midwest is also experiencing a milestone next year. We’re moving our experiential learning center to St. Paul. The Junior Achievement James R. and Patricia Hemak Experiential Learning Center will have two experiential learning labs instead of one, allowing us to double the number of students participating in JA BizTown and JA Finance Park. -

International Students Post-Graduation Employment Data
International Students Post-Graduation Employment Data 2014-2019 Major/Program Degree Employer City/State Job Title Accounting Master AdvisorNet Financial Minneapolis, MN Staff Accountant Accounting Master Anton Collins Mitchell LLP Greater Denver Area, CO Tax Associate Accounting Master Ashley Furniture Store Unknown Financial Analyst Accounting Master Bundeswehr wir. Dienen. Deutschland Munich Bavaria, Unknown Soldation in der Sportfordergruppe der Bundeswehr Accounting Bachelor Calix Inc Unknown Accountant Accounting Bachelor CBRE Mankato, MN Associate Real Estate Accountant Accounting Master Deloitte Canada Toronto, ON Staff Accountant Accounting Master Deloitte Tax LLP Minneapolis, MN Tax consultant Accounting Master Deloitte Tax LLP Minneapolis, MN Tax consultant Accounting Bachelor Dickeys Barbeque Corporate Office Dallas, TX Financial Analyst Accounting Master Divine Scherzer & Brody Ltd. Minneapolis, MN Tax Intern Accounting Bachelor Farmer Brothers Northlake, TX National Account Specialist Accounting Bachelor KPMG Jeddah, Unknown Assistant auditor Accounting Master KPMG LLP Seattle, WA Audit Associate Accounting Master LB Carlson, LLP Mankato, MN Senior Accounting Bachelor Midi Inn City am Kudamm Berlin, Brd, Unknown Receptionist Accounting Bachelor Minnesota State University Mankato Mankato, MN Student Payroll & Contracts Accounting Asst. Accounting Bachelor Obermeier & Associates, P.A. Burnsville, MN Tax Accountant Accounting Master PAN-CHINA CPA LIMITED Unknown Accountant Accounting Bachelor PwC Minneapolis, MN Assurance Associate -

Inleadership
IN LEADERSHIP How Minnesota’s Top 100 Public Companies Rank The 2009 Minnesota Census of Women in Corporate Leadership Report produced by St. Catherine University and the Minnesota Women’s Economic Roundtable A Statewide Wakeup Call The second annual Minnesota Census of Women in Corporate Leadership reveals that women remain an underutilized resource in the top ranks of public companies. Consider the evidence: Kudos and Contributions Twenty-seven of the top 100 public companies in This initiative has been made possible by many individuals • Minnesota have no women board members. and organizations. The report was underwritten by Spencer Stuart, St. Catherine University, and the Minnesota Women’s Forty-one of the top 100 public companies have only Economic Roundtable. • one woman on their boards. Support for both the report and the Forum was provided by Women hold only 15 percent of the Section 16b Twin Cities Business magazine and other sponsoring organiza- • (Securities and Exchange Commission) executive tions (see pages 26 to 28 of this report). Special thanks to the officer positions in Minnesota’s top 100 public volunteers who made up this year’s steering committee (see companies. the report’s final page). Without their tireless efforts, neither the report nor the Forum luncheon would have been possible. Nineteen of the top 100 public companies have no • women involved with leadership — either as directors Now, we turn to our readers — our state’s corporate and small- or executive officers. business leaders — to carry on this work, in the hope that future editions of The Minnesota Census will show progress We ask that women and men view this report as a wakeup on behalf of our state’s business climate and, subsequently, call, one whose findings deserve and demand to be shared all people in Minnesota. -

SCHEDULE 14A Proxy Statement Pursuant to Section 14(A) of the Securities Exchange Act of 1934
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 SCHEDULE 14A Proxy Statement Pursuant to Section 14(a) of the Securities Exchange Act of 1934 Filed by the Registrant x Filed by a Party other than the Registrant ¨ Check the appropriate box: ¨ Preliminary Proxy Statement ¨ Confidential, for use of the Commission only (as permitted by Rule 14a-6(e)(2)) x Definitive Proxy Statement ¨ Definitive Additional Materials ¨ Soliciting Material under Rule 14a-12 ManTech International Corporation (Name of Registrant as Specified In Its Charter) (Name of Person(s) Filing Proxy Statement, if other than the Registrant) Payment of Filing Fee (Check the appropriate box) x No fee required. ¨ Fee computed on table below per Exchange Act Rules 14a-6(i)(4) and 0-11. (1) Title of each class of securities to which transaction applies: (2) Aggregate number of securities to which transaction applies: (3) Per unit price or other underlying value of transaction computed pursuant to Exchange Act Rule 0-11 (Set forth the amount on which the filing fee is calculated and state how it was determined.): (4) Proposed maximum aggregate value of transaction: (5) Total fee paid: ¨ Fee paid previously with preliminary materials. ¨ Check box if any part of the fee is offset as provided by Exchange Act Rule 0-11(a)(2) and identify the filing for which the offsetting fee was paid previously. Identify the previous filing by registration statement number, or the Form or Schedule and the date of its filing. (1) Amount Previously Paid: (2) Form, Schedule or Registration Statement No.: (3) Filing Party: (4) Date Filed: 12015 Lee Jackson Highway Fairfax, VA 22033-3300 April 1, 2010 Dear Stockholder: You are cordially invited to attend the 2010 Annual Meeting of Stockholders of ManTech International Corporation, which will be held at The Hyatt Fair Lakes, 12777 Fair Lakes Circle, Fairfax, VA 22033, on Wednesday, May 12, 2010, at 11 am (EDT). -
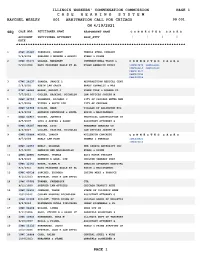
Combined ARB Callsheets Aprwk4 2021Revised
ILLINOIS WORKERS' COMPENSATION COMMISSION PAGE 1 C A S E H E A R I N G S Y S T E M RAYCHEL WESLEY 001 ARBITRATION CALL FOR CHICAGO 99 001 ON 4/19/2021 RAYCHEL WESL SEQ CASE NBR PETITIONER NAME RESPONDENT NAME C O N N E C T E D C A S E S ACCIDENT PETITIONER ATTORNEY RESP_ATTY ↓ ↓ ↓ ↓ DATE ************************************************************************ 1 05WC 45685 FRANKLIN, ROBERT TEMPLE STEEL COMPANY 5/6/2008 SHELDON I MINKOW & ASSOCI EVANS & DIXON 2 06WC 03171 GALADA, MARGARET INTERNATIONAL TRUCK & C O N N E C T E D C A S E S 5/10/2008 KATZ FRIEDMAN EAGLE ET AL NYHAN BAMBRICK KINZI 10WC015479 06WC023853 09WC048659 06WC010239 09WC019542 08WC007193 08WC005514 3 07WC 18137 ZAWADA, JANICE L RESURRECTION MEDICAL CENT 5/9/2002 RUBIN LAW GROUP BRADY CONNOLLY & MAS 4 07WC 38683 MOORE, DWIGHT J VOGUE TYRE & RUBBER CO 7/7/2012 CULLEN, HASKINS, NICHOLSO LAW OFFICES JOSEPH M 5 08WC 32755 PALMERIN, RICHARD J CITY OF CHICAGO WATER MGM 8/7/2003 VITELL & SPITZ LTD CITY OF CHICAGO 6 08WC 51988 DILLON, MARK VILLAGE OF ARLINGTON HTS 8/6/2006 RATHBUN CSEVENYAK & KOZOL RUSIN & MACIOROWSKI 7 08WC 53917 WALKER, JOHNNIE TECHNICAL CONSTRUCTION IN 8/5/2007 LUIS A ACEVES & ASSOC ASSISTANT ATTORNEY G 8 09WC 04287 MEDINA, LUIS FREEDMAN SEATING CO 8/3/2027 CULLEN, HASKINS, NICHOLSO LAW OFFICES JOSEPH M 9 09WC 06884 MEYER, LORRIN MILLENIUM CONCRETE C O N N E C T E D C A S E S 8/7/2008 HEALY LAW FIRM THOMAS & PORTELA 10WC032821 10WC026152 10 09WC 22055 NEELY, SELONGE THE SPORTS AUTHORITY INC 9/5/2005 DWORKIN AND MACIARIELLO EVANS & DIXON 11 09WC 30991 HAMMONS, -

Internship Sites by Department from 2015 First Destinations
Internship Sites by Department from 2015 First Destinations College of Arts & Sciences Ceridian Twin Cities Public Television Biology Ceridian Corporation University of St. Thomas 3M Children's Heartlink University of St. Thomas Development Cities 97 City of Minneapolis Office HCMC Committee Films University of St. Thomas Student Diversity and Inclusion Services Maplewood Dental Comunidades Latinas Unidas En Servicio University of St. Thomas Web Services Medical College of Wisconsin Concerned Veterans for America USA Racquetball Mille Lacs Health System Ctv North Suburbs Visit Saint Paul Oklahoma State University Direct Travel Wedding Shoppe, Inc. University of St. Thomas Biology European Wax Center Department EVINE Live Computer & Information Science University of St. Thomas Student Finnegans Brew Co. Ameriprise Financial Research FIS Global Buffalo Wild Wings University of St. Thomas Wellness Center Ghost Communication Great River Energy Wuxi AppTec Greenspring Media Group Navegate Catholic Studies IheartMedia Symantec Corporation Augustana Health Care Center Mpls Jostens University of St. Thomas Catholic Charities Northside Child KARE 11 University of St. Thomas Enrollment and Development Center Catholic Studies KARE11 Voya Financial Catholic Rural Life Student Kids in Need Foundation Economics Fraser Lifeworks Services, Inc. Ameriprise Maternity of Mary Parish Minnesota Children's Museum Minnesota Historical Society Ameriprise Financial Minnesota Connected Enterprise Disney Smiths Medical ASD Minnesota United FC Federal Reserve Bank -

2005 Annual Report
The Carlson School 2005 Annual Report Insight Experience Opportunity The Carlson School 2 Letter 4 Insight 12 Experience 20 Opportunity 24 The year in focus 26 Financial report 28 Enrollment, tuition, and student profiles 29 Rankings and employment 30 Faculty roster Cover photo: 33 Board of overseers Xiaodong Zhang, Professor Rob Kauffman, Ashley Burlage Carlson School of Management Insight, experience, and opportunity Undergraduate expansion Our planned undergrad- Every day, students enter our doors with high expectations. Some are uate expansion will allow the Carlson School young people with only a faint notion of their future career. Others to serve at least 50 per- are seasoned business leaders on a continuous quest. cent more students by 2008 and meet growing business demand. New They come to the Carlson School of Management for insight, to facility construction could start in fall 2006. expand their understanding of business. For experience, to put We’ll also expand fac- ulty, student and career insight into practice. For opportunity, to apply their leadership skills services, and scholar- ships. Funding from the in the larger community. Insight, experience, and opportunity are the state legislature, along with additional support three tenets of our mission. from our alumni and friends, will turn our new Every year, more than 4,000 students pass through our doors and building into reality and make our highly-ranked into the world. Learn where insight, experience, and opportunity Undergraduate program even stronger. took them this year. And see how we are working to meet the needs of tomorrow’s leaders and the next generation of business. -

Empowering Young People to Own Their Economic Success
Empowering young people to own their economic success Mission Report 2012-2013 Inspiring and preparing young people to succeed in a global economy. Dear Partner, As our nation focuses its attention on ways to create jobs and spur economic growth, Junior Achievement (JA) continues to expand the depth and reach of its programs. We have done so by providing 149,500 young people with relevant, experiential learning opportunities centered on financial literacy, college and career readiness and entrepreneurship. JA’s unique approach relies on volunteers from the community who deliver our curriculum while sharing their experiences with students. The dynamic interaction between students, educators and volunteers promotes active learning while bringing theory to life. The JA experience establishes the foundation on which young people can build the skills and attitudes necessary to succeed in a fast-paced world. The case for JA has never been stronger and we are excited to build on the success of this past year with a focus for the future on the following: • Strengthen economic literacy by delivering elementary programs sequentially with school districts committed to long-term partnerships. • Accelerate growth of our high school programs to enhance student skills in financial literacy, college and career readiness and entrepreneurship. • Partner to reach students out of school, expanding the learning day and providing students with experiences that promote their roles as citizens, consumers and workers. • Grow our capstone programs (JA BizTown, JA Finance Park, JA Company Program, JA Job Shadow and JA Titan) to equip students with 21st century skills that will benefit them in the real world. -

JA Report 2012.WEB.Indd
Financial Literacy | College and Career Readiness | Entrepreneurship Annual Report 2011-2012 Read Max Goldman’s inspiring JA story inside. Inspiring and preparing young people to succeed in a global economy. jaum.org Junior Achievement of the Upper Midwest 1800 White Bear Avenue North, Maplewood, MN 55109 tel: 651.255.0055 | fax: 651.255.0460 | www.jaum.org Design: Richard Hart Design | Printing: AFPI www.jaum.org Dear Partner: This past school year, thousands of community volunteers donated their time and expertise in the classroom, working with teachers and students to teach personal finance, college and career readiness and entrepreneurship. As a result, students in grades K-12 learned real-world skills that will help them succeed in school and beyond. Thank you! In light of the painful economic lessons recently learned by governments, families and businesses, there is an even greater need to educate our youth about how to effectively manage money and prepare for their future. JA programs teach 21st century skills and offer real-world experiences. In the coming year, JAUM is focusing on the following strategies to keep our organization relevant: • Integrate STEM (Science, Technology, Engineering, Math) careers at JA BizTown and introduce STEM into our K-12 curriculum • Educate students of different backgrounds and ethnicities about financial literacy, college and career readiness and entrepreneurship • Incorporate innovative teaching methods into our learning facility and into our curriculum such as smart board technology, video lessons and personal devices • Offer real-life experiences (job shadows, competitions, capstone projects) to expose students to opportunities beyond their classroom • Conduct local evaluations to validate learning and JAUM’s impact on student motivation As we embark on another exciting year, we look to you for continued support to help connect students with educators and business people to build a more fiscally savvy community. -

COMPANY COMPANY2 STREET CITY STATE ZIP Cloverdale
COMPANY COMPANY2 STREET CITY STATE ZIP Cloverdale Healthcare Inc Cloverdale Manor 412 W Cloverdale Rd Scottsboro AL 35768 Lozier Corporation 401 TAYLOR STREET SCOTTSBORO AL 35768 Lowes Home Centers Inc 481 130 Cox Creek Pkwy S Florence AL 35630 Wenzel Metal Spinning Inc Scottsboro Industrial Par Scottsboro AL 35768 Ajax Tocco Magnethermic Corp Tim Stracener 1506 Industrial Blvd Boaz AL 35957 Lowes Home Centers Inc 606 2671 Ross Clark Cir Dothan AL 36301 Monarch Steel of Alabama Inc 1425 Red Hat Rd Decatur AL 35601 Lowes Home Centers Inc 1726 5291 Highway 280 Birmingham AL 35242 Dothan-Hostn Cty Mntl Retardation Bd. Inc. Vaughn Blumberg Center 2715 Flynn Rd Dothan AL 36303 Meridian Rail Acquisition Greenbrier Rail Services 1200 Corporate Dr Ste 450 Birmingham AL 35242 J L S International Inc 24063 County Road 71 Robertsdale AL 36567 Proshot Concrete Inc 4158 Musgrove Dr Florence AL 35630 Lowes Home Centers Inc 313 1717 Cherokee Ave SW Cullman AL 35055 Utility Trailer Mfg Co HWY 84 & 84 BYP ENTERPRISE AL 36330 Coca-Cola Bottling Co. Consolidated Coca-Cola 4530 Starkey Dr Florence AL 35630 Rainsville Technology Inc Jeremy Lasseter 189 RTI DRIVE Rainsville AL 35986 E & H Steel Corporation 3635 E Hywy 134 Midland City AL 36350 Crowne Investments Inc Parkwood Healthcare Facility 3301 Stadium Dr Phenix City AL 36867 Terex Utilities 4120 Lewisburg Rd Birmingham AL 35207 Ggnsc Winfield LLC 144 County Hghway 14 Winfield AL 35594 Pemco Corporation 100 Pemco Dr Leesburg AL 35983 Hart & Cooley Inc 4910 Moores Mill Rd Huntsville AL 35811 National Healthcare -

COUNCIL MINUTES August 17, 2020
COUNCIL MINUTES August 17, 2020 Pursuant to due call and notice thereof, a regular meeting of the North Mankato City Council was held in the Municipal Building Council Chambers on August 17, 2020. City Administrator Harrenstein on March 31, 2020, under MN Statute Section 13D.02 l, declared the use of electronic meetings due to the COVID-19 pandemic. Mayor Dehen called the meeting to order at 7:00 p.m., asking that everyone join in the Pledge of Allegiance. The following were present remotely through Zoom for roll call: Council Members Whitlock, Oachs and Steiner, City AttorneyKennedy, Finance Director McCann, Community Development Director Fischer, and Public Works Director Host, present in the Council Chambers forroll call: Council Member Norland, Mayor Dehen, City Administrator Harrenstein, and City Clerk Van Genderen. Citizen participation was available through teleconferenceand live stream of the meeting. Approval of Agenda Council Member Norland moved, seconded by Council Member Steiner, to approve the agenda. Vote on the motion: Whitlock, Steiner, Norland, Oachs, and Dehen aye; no nays. Motion carried. Approval Council Minutes from the August 3, 2020, Council Meeting. Council Member Norland moved, seconded by Council Member Oachs, to approve the minutes of the Council meeting of August 3, 2020. Vote on the motion: Whitlock, Steiner, Norland, Oachs, and Dehen aye; no nays. Motion carried. Approval of Council Work Session Minutes from the August 10, 2020, Council Work Session. Council Member Oachs moved, seconded by Council Member Norland, to approve the minutes of the Council Work Session Meeting of August 10, 2020. Vote on the motion: Whitlock, Steiner, Norland, Oachs, and Dehen aye; no nays.