Ketamine Blocks Morphine-Induced Conditioned Place Preference And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -

Euphoric Non-Fentanil Novel Synthetic Opioids on the Illicit Drugs Market
Forensic Toxicology (2019) 37:1–16 https://doi.org/10.1007/s11419-018-0454-5 REVIEW ARTICLE The search for the “next” euphoric non‑fentanil novel synthetic opioids on the illicit drugs market: current status and horizon scanning Kirti Kumari Sharma1,2 · Tim G. Hales3 · Vaidya Jayathirtha Rao1,2 · Niamh NicDaeid4,5 · Craig McKenzie4 Received: 7 August 2018 / Accepted: 11 November 2018 / Published online: 28 November 2018 © The Author(s) 2018 Abstract Purpose A detailed review on the chemistry and pharmacology of non-fentanil novel synthetic opioid receptor agonists, particularly N-substituted benzamides and acetamides (known colloquially as U-drugs) and 4-aminocyclohexanols, developed at the Upjohn Company in the 1970s and 1980s is presented. Method Peer-reviewed literature, patents, professional literature, data from international early warning systems and drug user fora discussion threads have been used to track their emergence as substances of abuse. Results In terms of impact on drug markets, prevalence and harm, the most signifcant compound of this class to date has been U-47700 (trans-3,4-dichloro-N-[2-(dimethylamino)cyclohexyl]-N-methylbenzamide), reported by users to give short- lasting euphoric efects and a desire to re-dose. Since U-47700 was internationally controlled in 2017, a range of related compounds with similar chemical structures, adapted from the original patented compounds, have appeared on the illicit drugs market. Interest in a structurally unrelated opioid developed by the Upjohn Company and now known as BDPC/bromadol appears to be increasing and should be closely monitored. Conclusions International early warning systems are an essential part of tracking emerging psychoactive substances and allow responsive action to be taken to facilitate the gathering of relevant data for detailed risk assessments. -

(19) United States (12) Patent Application Publication (10) Pub
US 20100227876A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0227876 A1 Rech (43) Pub. Date: Sep. 9, 2010 (54) METHODS OF REDUCING SIDE EFFECTS Publication Classi?cation OF ANALGESICS (51) Int CL A61K 31/485 (2006.01) A61K 31/40 (2006.01) (75) Inventor: Richard H. Rech, Okemos, MI A61K 31/445 (2006-01) (Us) A61K 31/439 (2006.01) (52) US. Cl. ........................ .. 514/282; 514/409; 514/329 (57) ABSTRACT Correspondence Address: The invention provides for compositions and methods of MARSHALL, GERSTEIN & BORUN LLP reducing pain in a subject by administering a combination of 233 SOUTH WACKER DRIVE, 6300 WILLIS mu-opioid receptor agonist, kappal-opioid receptor agonist TOWER and a nonselective opioid receptor antagonist in amounts CHICAGO, IL 60606-6357 (US) effective to reduce pain and ameliorate an adverse side effect of treatment combining opioid-receptor agonists. The inven tion also provides for methods of enhancing an analgesic effect of treatment With an opioid-receptor agonist in a sub (73) Assignee: RECHFENSEN LLP, RidgeWood, ject suffering from pain While reducing an adverse side effect NJ (US) of the treatment. The invention also provides for methods of reducing the hyperalgesic effect of treatment With an opioid receptor agonist in a subject suffering from pain While reduc ing an adverse side effect of the treatment. The invention (21) Appl. No.: 12/399,629 further provides for methods of promoting the additive anal gesia of pain treatment With an opioid-receptor agonist in a subject in need While reducing an adverse side effect of the (22) Filed: Mar. -

Opioid Receptorsreceptors
OPIOIDOPIOID RECEPTORSRECEPTORS defined or “classical” types of opioid receptor µ,dk and . Alistair Corbett, Sandy McKnight and Graeme Genes encoding for these receptors have been cloned.5, Henderson 6,7,8 More recently, cDNA encoding an “orphan” receptor Dr Alistair Corbett is Lecturer in the School of was identified which has a high degree of homology to Biological and Biomedical Sciences, Glasgow the “classical” opioid receptors; on structural grounds Caledonian University, Cowcaddens Road, this receptor is an opioid receptor and has been named Glasgow G4 0BA, UK. ORL (opioid receptor-like).9 As would be predicted from 1 Dr Sandy McKnight is Associate Director, Parke- their known abilities to couple through pertussis toxin- Davis Neuroscience Research Centre, sensitive G-proteins, all of the cloned opioid receptors Cambridge University Forvie Site, Robinson possess the same general structure of an extracellular Way, Cambridge CB2 2QB, UK. N-terminal region, seven transmembrane domains and Professor Graeme Henderson is Professor of intracellular C-terminal tail structure. There is Pharmacology and Head of Department, pharmacological evidence for subtypes of each Department of Pharmacology, School of Medical receptor and other types of novel, less well- Sciences, University of Bristol, University Walk, characterised opioid receptors,eliz , , , , have also been Bristol BS8 1TD, UK. postulated. Thes -receptor, however, is no longer regarded as an opioid receptor. Introduction Receptor Subtypes Preparations of the opium poppy papaver somniferum m-Receptor subtypes have been used for many hundreds of years to relieve The MOR-1 gene, encoding for one form of them - pain. In 1803, Sertürner isolated a crystalline sample of receptor, shows approximately 50-70% homology to the main constituent alkaloid, morphine, which was later shown to be almost entirely responsible for the the genes encoding for thedk -(DOR-1), -(KOR-1) and orphan (ORL ) receptors. -

What Are the Treatments for Heroin Addiction?
How is heroin linked to prescription drug abuse? See page 3. from the director: Research Report Series Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a devastating impact on society and cost billions of dollars each year. Although heroin use in the general population is rather low, the numbers of people starting to use heroin have been steadily rising since 2007.1 This may be due in part to a shift from abuse of prescription pain relievers to heroin as a readily available, cheaper alternative2-5 and the misperception that highly pure heroin is safer than less pure forms because it does not need to be injected. Like many other chronic diseases, addiction can be treated. Medications HEROIN are available to treat heroin addiction while reducing drug cravings and withdrawal symptoms, improving the odds of achieving abstinence. There are now a variety of medications that can be tailored to a person’s recovery needs while taking into account co-occurring What is heroin and health conditions. Medication combined with behavioral therapy is particularly how is it used? effective, offering hope to individuals who suffer from addiction and for those around them. eroin is an illegal, highly addictive drug processed from morphine, a naturally occurring substance extracted from the seed pod of certain varieties The National Institute on Drug Abuse (NIDA) has developed this publication to Hof poppy plants. -

Table of Contents
TheJournalof VOLUME271 PHARMACOLOGY NUMBER 3 AND EXPERIMENTAL THERAPEUTICS Contents ANTI-INFLAMMATORIES Lecithinized Superoxide Dismutase Enhances Its R. Igarashi, J. Hoshino, A. Ochiai, 1672 Pharmacologic Potency by Increasing Its Cell Membrane Y. Morizawa and Y. Mizushima Affinity ANALGESICS Role of Endogenous Cholecystokinin in the Facilitation of Mu- Florence Noble, Claire Smadja and 1127 Mediated Antinociception by Delta.Opioid Agonists Bernard P. Roques Downloaded from GBR12909 Attenuates Cocaine-Induced Activation of Michael H. Baumann, George U. Char, 1216 Mesolimbic Dopamine Neurons in the Rat Brian R. Dc Costa, Kenner C. Rice and Richard B. Rothman Substance P N-Terminal Metabolites and Nitric Oxide Mediate Julie S. Kreeger, Kelley F. Kitto and 1281 Capsaicin-Induced Antinociception in the Adult Mouse Alice A. Larson Antinociceptive Actions of Dexmedetomidine and the Kappa- Juhana J. Idanpaan-Heikkila, Eija A. Kalso 1306 jpet.aspetjournals.org Opioid Agonist U.5O,488H against Noxious Thermal, and Timo Seppala Mechanical and Inflammatory Stimuli Involvement of NMDA Receptors in Naloxone-Induced Rustam Yu. Yukhananov and 1365 Contractions of the Isolated Guinea Pig ileum after Alice A. Larson Preincubation with Morphine Development of Cross-Tolerance between - Fang Fan, David R. Compton, Susan Ward, 1383 Tetrahydrocannabinol, CP 55,940 and WIN 55,212 Lawrence Melvin and Billy R. Martin at ASPET Journals on October 2, 2021 Antinociceptive and Response Rate-Altering Effects of Kappa Raymond C. Pitts and Linda A. Dykstra 1501 Opioid Agonists, Spiradoline, Enadoline and U69,593, Alone and in Combination with Opioid Antagonists in Squirrel Monkeys The Influence of Pharmacogenetics on Opioid Analgesia: Jim Cleary, Gerd Mikus, Andrew Somogyi 1528 Studies with Codeine and Oxycodone in the Sprague-Dawley/ and Felix Bochner Dark Agouti Rat Model Selective Antagonism of Opioid Analgesia by a Sigma System Chih-Cheng Chien and 1583 Gavril W. -
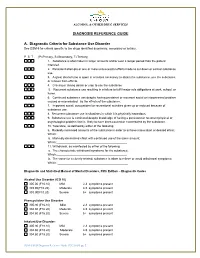
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b. -
BBC Program 2016.Pages
March 5-6, 2016 La Quinta Inn & Suites Medical Center San Antonio, TX Behavior, Biology, and Chemistry: Translational Research in Addiction BBC 2016 BBC Publications BBC 2011 Stockton Jr SD and Devi LA (2012) Functional relevance of μ–δ opioid receptor heteromerization: A Role in novel signaling and implications for the treatment of addiction disorders: From a symposium on new concepts in mu-opioid pharmacology. Drug and Alcohol Dependence Mar 1;121(3):167-72. doi: 10.1016/j.drugalcdep.2011.10.025. Epub 2011 Nov 23 Traynor J (2012) μ-Opioid receptors and regulators of G protein signaling (RGS) proteins: From a sym- posium on new concepts in mu-opioid pharmacology. Drug and Alcohol Dependence Mar 1;121(3): 173-80. doi: 10.1016/j.drugalcdep.2011.10.027. Epub 2011 Nov 29 Lamb K, Tidgewell K, Simpson DS, Bohn LM and Prisinzano TE (2012) Antinociceptive effects of herkinorin, a MOP receptor agonist derived from salvinorin A in the formalin test in rats: New concepts in mu opioid receptor pharmacology: From a symposium on new concepts in mu-opioid pharma- cology. Drug and Alcohol Dependence Mar 1;121(3):181-8. doi: 10.1016/j.drugalcdep.2011.10.026. Epub 2011 Nov 26 Whistler JL (2012) Examining the role of mu opioid receptor endocytosis in the beneficial and side-ef- fects of prolonged opioid use: From a symposium on new concepts in mu-opioid pharmacology. Drug and Alcohol Dependence Mar 1;121(3):189-204. doi: 10.1016/j.drugalcdep.2011.10.031. Epub 2012 Jan 9 BBC 2012 Zorrilla EP, Heilig M, de Wit, H and Shaham Y (2013) Behavioral, biological, and chemical perspectives on targeting CRF1 receptor antagonists to treat alcoholism. -

212102Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 212102Orig1s000 OTHER REVIEW(S) Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research | Office of Surveillance and Epidemiology (OSE) Epidemiology: ARIA Sufficiency Date: June 29, 2020 Reviewer: Silvia Perez-Vilar, PharmD, PhD Division of Epidemiology I Team Leader: Kira Leishear, PhD, MS Division of Epidemiology I Division Director: CAPT Sukhminder K. Sandhu, PhD, MPH, MS Division of Epidemiology I Subject: ARIA Sufficiency Memo for Fenfluramine-associated Valvular Heart Disease and Pulmonary Arterial Hypertension Drug Name(s): FINTEPLA (Fenfluramine hydrochloride, ZX008) Application Type/Number: NDA 212102 Submission Number: 212102/01 Applicant/sponsor: Zogenix, Inc. OSE RCM #: 2020-953 The original ARIA memo was dated June 23, 2020. This version, dated June 29, 2020, was amended to include “Assess a known serious risk” as FDAAA purpose (per Section 505(o)(3)(B)) to make it consistent with the approved labeling. The PMR development template refers to the original memo, dated June 23, 2020. Page 1 of 13 Reference ID: 46331494640015 EXECUTIVE SUMMARY (place “X” in appropriate boxes) Memo type -Initial -Interim -Final X X Source of safety concern -Peri-approval X X -Post-approval Is ARIA sufficient to help characterize the safety concern? Safety outcome Valvular Pulmonary heart arterial disease hypertension (VHD) (PAH) -Yes -No X X If “No”, please identify the area(s) of concern. -Surveillance or Study Population X X -Exposure -Outcome(s) of Interest X X -Covariate(s) of Interest X X -Surveillance Design/Analytic Tools Page 2 of 13 Reference ID: 46331494640015 1. -

(12) Patent Application Publication (10) Pub. No.: US 2011/0245287 A1 Holaday Et Al
US 20110245287A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0245287 A1 Holaday et al. (43) Pub. Date: Oct. 6, 2011 (54) HYBRD OPOD COMPOUNDS AND Publication Classification COMPOSITIONS (51) Int. Cl. A6II 3/4748 (2006.01) C07D 489/02 (2006.01) (76) Inventors: John W. Holaday, Bethesda, MD A6IP 25/04 (2006.01) (US); Philip Magistro, Randolph, (52) U.S. Cl. ........................................... 514/282:546/45 NJ (US) (57) ABSTRACT Disclosed are hybrid opioid compounds, mixed opioid salts, (21) Appl. No.: 13/024,298 compositions comprising the hybrid opioid compounds and mixed opioid salts, and methods of use thereof. More particu larly, in one aspect the hybrid opioid compound includes at (22) Filed: Feb. 9, 2011 least two opioid compounds that are covalently bonded to a linker moiety. In another aspect, the hybrid opioid compound relates to mixed opioid salts comprising at least two different Related U.S. Application Data opioid compounds or an opioid compound and a different active agent. Also disclosed are pharmaceutical composi (60) Provisional application No. 61/302,657, filed on Feb. tions, as well as to methods of treating pain in humans using 9, 2010. the hybrid compounds and mixed opioid salts. Patent Application Publication Oct. 6, 2011 Sheet 1 of 3 US 2011/0245287 A1 Oral antinociception of morphine, oxycodone and prodrug combinations in CD1 mice s Tigkg -- Morphine (2.80 mg/kg (1.95 - 4.02, 30' peak time -- (Oxycodone (1.93 mg/kg (1.33 - 2,65)) 30 peak time -- Oxy. Mor (1:1) (4.84 mg/kg (3.60 - 8.50) 60 peak tire --MLN 2-3 peak, effect at a hors 24% with closes at 2.5 art to rigg - D - MLN 2-45 (6.60 mg/kg (5.12 - 8.51)} 60 peak time Figure 1. -

Opioid Use Disorders
AD APTING YOUR PRACTIC E Recommendations for the Care of Homeless Patients with Opioid Use Disorders Opioid Use Disorders March 2014 ADAPTING YOUR PRACTICE Recommendations for the Care of Homeless Patients with Opioid Use Disorders Health Care for the Homeless Clinicians’ Network March 2014 Health Care for the Homeless Clinicians’ Network Adapting Your Practice: Recommendations for the Care of Homeless Patients with Opioid Use Disorders was developed with support from the Bureau of Primary Health Care, Health Resources and Services Administration, U.S. Department of Health and Human Services. All material in this document is in the public domain and may be used and reprinted without special permission. Citation as to source, however, is appreciated. Suggested citation: Meges D, Zevin B, Cookson E, Bascelli L, Denning P, Little J, Doe-Simkins M, Wheeler E, Watlov Phillips S, Bhalla P, Nance M, Cobb G, Tankanow J, Williamson J, Post P (Ed.). Adapting Your Practice: Recommendations for the Care of Homeless Patients with Opioid Use Disorders. 102 pages. Nashville: Health Care for the Homeless Clinicians' Network, National Health Care for the Homeless Council, Inc., 2014. DISCLAIMER This publication was made possible by grant number U30CS09746 from the Health Resources & Services Administration, Bureau of Primary Health Care. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Health Resources & Services Administration. i ADAPTING YOUR PRACTICE Recommendations for the Care of Homeless Patients with Opioid Use Disorders Health Care for the Homeless Clinicians’ Network PREFACE Clinicians experienced in homeless health care routinely adapt their practice to foster better outcomes for their patients. -
HHS Guide for Clinicians on the Appropriate Dosage Reduction Or
This HHS Guide for Clinicians on the Appropriate Dosage HHS Guide for Clinicians on the Reduction or Discontinuation of Long-Term Opioid Analgesics provides advice to clinicians who are contemplating or initiating a reduction in opioid dosage or discontinuation Appropriate Dosage Reduction of long-term opioid therapy for chronic pain. In each case the clinician should review the risks and benefits of the or Discontinuation of current therapy with the patient, and decide if tapering is appropriate based on individual circumstances. Long-Term Opioid Analgesics After increasing every year for more than a decade, annual needs.2,3,4 Coordination across the health care team is critical. opioid prescriptions in the United States peaked at 255 million in Clinicians have a responsibility to provide or arrange for 2012 and then decreased to 191 million in 2017.i More judicious coordinated management of patients’ pain and opioid-related opioid analgesic prescribing can benefit individual patients as problems, and they should never abandon patients.2 More well as public health when opioid analgesic use is limited to specific guidance follows, compiled from published guidelines situations where benefits of opioids are likely to outweigh risks. (the CDC Guideline for Prescribing Opioids for Chronic Pain2 At the same time opioid analgesic prescribing changes, such and the VA/DoD Clinical Practice Guideline for Opioid Therapy as dose escalation, dose reduction or discontinuation of long- for Chronic Pain3) and from practices endorsed in the peer- term opioid analgesics, have potential to harm or put patients at reviewed literature. risk if not made in a thoughtful, deliberative, collaborative, and measured manner.