Use of Naloxone for the Prevention of Opioid Overdose Deaths
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Substance Use Resources for Grades 7-12
1 Substance Use Resources for Grades 7-12 Online Resource Library Search: https://www.voa-dakotas.org/resource-library Addiction: page 1 Alcohol: page 1 Drugs: page 4 Vaping/tobacco: page 10 Addiction Addiction and the Human Brain o DVD, 2006, HRM, 27 minutes, Grades 7-12 o Drug addiction is a disease of the brain and teens are at highest risk for acquiring this disease. This DVD explains the changes to the brain caused by prolonged use of drugs and shows why voluntary drug use eventually becomes involuntary and compulsive. Studies indicate that drugs affect the developing brain more than the brain of someone more mature, thus putting teens at a higher risk of addiction. Interviews with recovering teen addicts, an addiction counselor, and brain experts and researchers provide sobering considerations to viewers. Pre- and Post-tests are included. How Addiction Hijacks the Brain o DVD, 2016, HRM, CC, 24 minutes, Grades 7-College o This film drives home the message that drug and alcohol addiction are a disease of the brain and that teens are at highest risk for acquiring this disease. Leading scientists detail how drugs like heroin, nicotine, cocaine and marijuana change the brain, subvert the way it registers pleasure, and corrupt learning and motivation. Young recovering addicts provide a human face to the effects of drugs and alcohol as they describe how addiction involves intense craving for a drug and loss of control over its use. Viewers also learn that the brain’s plasticity, or ability to change, offers hope for addicts that they can turn their lives around. -

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -
Opioid Overdose – Use of Naloxone
CHAPTER: 41.3.1 Page 1 of 4 NEW ORLEANS POLICE DEPARTMENT OPERATIONS MANUAL CHAPTER: 41.3.1 TITLE: OPIOID OVERDOSE – USE OF NALOXONE EFFECTIVE: 10/22/2017 REVISED: 06/24/2018 PURPOSE The purpose of this policy is to set forth guidelines with respect to the appropriate field administration of Naloxone (Narcan) kits by members of New Orleans Police Department in suspected opiate / opioid overdose incidents. POLICY STATEMENT 1. Commissioned members of the NOPD are often the first emergency responders to the scene of a medical, suspected medical and overdose incident. Recognizing this, the NOPD has adopted this Chapter with the following goals: (a) To provide a framework for training in the field use of Naloxone, (b) To provide a framework on the proper field administration of Naloxone, and (c) To facilitate life-saving intervention in suspected opiate / opioid overdose incidents where NOPD officers are the first to arrive on the scene. 2. All commissioned and/or civilian members who have been trained in the use and administration of the department’s Naloxone nasal administration kits for suspected opiate / opioid overdose incidents are authorized to carry, use and administer the kits. 3. All members responding to medical calls, including suspected opioid overdoses, shall use universal precautions. DEFINITIONS: Definitions related to this Chapter include: Administration—Nasal administration of approved Naloxone 2mg kits with atomizer; 1mg (1/2 dose) to be administered in each nostril. Naloxone—A narcotic analgesic antagonist, used in the reversal of acute narcotic analgesic respiratory depression. Naloxone is effectively an antidote to opioid overdose and may completely reverse the effects of an opioid overdose if administered in time. -

1 Title Page Pharmacological Comparison of Mitragynine and 7
JPET Fast Forward. Published on December 31, 2020 as DOI: 10.1124/jpet.120.000189 This article has not been copyedited and formatted. The final version may differ from this version. JPET-AR-2020-000189R1: Obeng et al. Pharmacological Comparison of Mitragynine and 7-Hydroxymitragynine: In Vitro Affinity and Efficacy for Mu-Opioid Receptor and Morphine-Like Discriminative-Stimulus Effects in Rats. Title Page Pharmacological Comparison of Mitragynine and 7-Hydroxymitragynine: In Vitro Affinity and Efficacy for Mu-Opioid Receptor and Opioid-Like Behavioral Effects in Rats Samuel Obeng1,2,#, Jenny L. Wilkerson1,#, Francisco León2, Morgan E. Reeves1, Luis F. Restrepo1, Lea R. Gamez-Jimenez1, Avi Patel1, Anna E. Pennington1, Victoria A. Taylor1, Nicholas P. Ho1, Tobias Braun1, John D. Fortner2, Morgan L. Crowley2, Morgan R. Williamson1, Victoria L.C. Pallares1, Marco Mottinelli2, Carolina Lopera-Londoño2, Christopher R. McCurdy2, Lance R. McMahon1, and Takato Hiranita1* Downloaded from Departments of Pharmacodynamics1 and Medicinal Chemistry2, College of Pharmacy, University of Florida jpet.aspetjournals.org #These authors contributed equally Recommended section: Behavioral Pharmacology at ASPET Journals on September 29, 2021 Correspondence: *Takato Hiranita, Ph.D. Department of Pharmacodynamics, College of Pharmacy, University of Florida 1345 Center Drive, Gainesville, FL 32610 Email: [email protected] Phone: +1.352.294.5411 Fax: +1.352.273.7705 Keywords: kratom, mitragynine, 7-hydroxymitragynine, morphine, opioid, discriminative stimulus Conflicts of Interests or Disclaimers: None Manuscript statistics: Number of text pages: 56 Number of tables: 7 Number of figures: 10 Number of supplementary Tables: 4 Number of supplementary figures: 7 1 JPET Fast Forward. Published on December 31, 2020 as DOI: 10.1124/jpet.120.000189 This article has not been copyedited and formatted. -
Naloxone FAQ What Is Naloxone?
1 Naloxone FAQ What is naloxone? An FDA approved opioid antagonist prescription medication that reverses opioid overdoses. Two of the most common ways that naloxone is administered are intranasally (nasal spray) and the auto-injector. Naloxone is available under the names of” naloxone,” an injectable that, with attachments can also be used as a nasal spray; “NARCAN,” an already assembled and easy to administer nasal spray; and, finally “EVZO,” a prefilled auto-injector. How does it work? It stops or reverses the effects of an opioid overdose and restores breathing within two (2) to eight (8) minutes. The naloxone effect lasts from 20 to 90 minutes, and can be safely readministered as indicated. Is it safe? Yes. It cannot be used to get high and it is non-addictive . Where do I find an approved training? Free in-person NARCAN administration training is available at Prevention Point Philadelphia. Where do I find an approved online training and how long does training take? www.getnaloxonenow.org https://www.pavtn.net/act-139-training http://prescribetoprevent.org/patient-education/videos/ Training takes approximately 20 minutes. Does Act 139 under Provision of Good Samaritan cover provider agencies? Yes. How do we obtain naloxone? Providers will have to purchase by prescription. Individuals may do so by prescription or by standing order issued by Pennsylvania’s Physician General, Dr. Rachel Levine. Some pharmacies keep this standing order on file. NALOXONE/NARCAN FAQ Page 1 2 Naloxone FAQ (continued) Does Medical Assistance require prior authorization for any of the naloxone products? The Evzio Auto-Injector is covered by Medical Assistance, but requires prior authorization. -

Opioid Receptorsreceptors
OPIOIDOPIOID RECEPTORSRECEPTORS defined or “classical” types of opioid receptor µ,dk and . Alistair Corbett, Sandy McKnight and Graeme Genes encoding for these receptors have been cloned.5, Henderson 6,7,8 More recently, cDNA encoding an “orphan” receptor Dr Alistair Corbett is Lecturer in the School of was identified which has a high degree of homology to Biological and Biomedical Sciences, Glasgow the “classical” opioid receptors; on structural grounds Caledonian University, Cowcaddens Road, this receptor is an opioid receptor and has been named Glasgow G4 0BA, UK. ORL (opioid receptor-like).9 As would be predicted from 1 Dr Sandy McKnight is Associate Director, Parke- their known abilities to couple through pertussis toxin- Davis Neuroscience Research Centre, sensitive G-proteins, all of the cloned opioid receptors Cambridge University Forvie Site, Robinson possess the same general structure of an extracellular Way, Cambridge CB2 2QB, UK. N-terminal region, seven transmembrane domains and Professor Graeme Henderson is Professor of intracellular C-terminal tail structure. There is Pharmacology and Head of Department, pharmacological evidence for subtypes of each Department of Pharmacology, School of Medical receptor and other types of novel, less well- Sciences, University of Bristol, University Walk, characterised opioid receptors,eliz , , , , have also been Bristol BS8 1TD, UK. postulated. Thes -receptor, however, is no longer regarded as an opioid receptor. Introduction Receptor Subtypes Preparations of the opium poppy papaver somniferum m-Receptor subtypes have been used for many hundreds of years to relieve The MOR-1 gene, encoding for one form of them - pain. In 1803, Sertürner isolated a crystalline sample of receptor, shows approximately 50-70% homology to the main constituent alkaloid, morphine, which was later shown to be almost entirely responsible for the the genes encoding for thedk -(DOR-1), -(KOR-1) and orphan (ORL ) receptors. -

Epidemic of Prescription Drug Overdose in Ohio
EPIDEMIC OF PRESCRIPTION There were more deaths in 2008 and 2009 in Ohio from D RUG OVERDOSE IN OHIO unintentional drug overdose than from DID YOU KNOW? motor vehicle In 2007, unintentional drug poisoning became the leading crashes! cause of injury death in Ohio, surpassing motor vehicle crashes and suicide for the first time on record. This trend continued in 2009. (See Figure 1) Among the leading causes of injury death (see below), unintentional poisonings increased from the cause of the fewest number of annual deaths in 1999 (369 deaths) to the greatest in 2009 (1,817).i (See Figure 2) From 1999 to 2009, Ohio’s death rate due to unintentional drug poisonings increased 335 percent, and the increase in deaths has been driven largely by prescription drug overdoses. In Ohio, there were 327 fatal unintentional drug overdoses in 1999 growing to 1,423 annual deaths in 2009. On average, from 2006 to 2009, approximately four people died each day in Ohio due to drug overdose.v Figure 1. Number of deaths from MV traffic Figure 2 . Percent change in the number of deaths for and unintentional drug poisonings by year, the leading causes of injury, Ohio 1999-20091,2 Ohio, 2000-20091,2 1800 all unintentional 39% 1600 firearm related 15% 1400 1200 homicide 34% 1000 unintentional suicide 17% 800 poisoning 600 unintentional poisoning 301% unt MV traffic Number of deathsNumber 400 unt MV traffic -31% 200 unintentional falls 100% 0 -100% 0% 100% 200% 300% 400% Percent change from 2000-2009 Year 1Source: Ohio Department of Health, Office of Vital Statistics; 2 Unintentional Poisoning includes non-drug and drug-related poisoning. -

Safety Notice 009/20 Acetylfentanyl and Fentanyl In
Safety Notice 009/20 Acetylfentanyl and fentanyl in non-opioid illicit drugs 16 October 2020 Background Distributed to: A cluster of hospitalisations due to unexpected opioid toxicity recently occured on • Chief Executives the Central Coast of NSW. Acetylfentanyl and fentanyl are circulating in NSW and • Directors of Clinical Governance may be misrepresented as or be adulterants in illicit cocaine or ketamine. • Director Regulation and Acetylfentanyl has a similar potency to fentanyl, both may cause serious harm and Compliance Unit death. People who do not use opioids regularly (‘opioid naïve’) may be unintentionally exposed and are at high risk of overdose. Even people who Action required by: regularly use opioids are at risk due to the relatively high potency of fentanyl and • Chief Executives acetylfentanyl. • Directors of Clinical Changes in illicit drug use in 2020, as well as variations in purity and alternative Governance ingredients, may be associated with unusual presentations and overdose. • Director Regulation and Compliance Unit Case management • We recommend you also Have a high index of suspicion for illicit fentanyl and fentanyl analogues in inform: suspected opioid overdose. This includes people who deny opioid use or • Drug and Alcohol Directors report use of other non-opioid illicit drugs including ketamine or stimulants and staff such as cocaine, but who present clinically with signs of an opioid • All Service Directors overdose. • Emergency Department • Intensive Care Unit • Airway management, oxygenation, and ventilation support take precedence • Toxicology Units over naloxone, where appropriate. • Ambulance • Cases may require titrated doses of naloxone with a higher total dose of • All Toxicology Staff 800 micrograms or more. -

ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update
The ASAM NATIONAL The ASAM National Practice Guideline 2020 Focused Update Guideline 2020 Focused National Practice The ASAM PRACTICE GUIDELINE For the Treatment of Opioid Use Disorder 2020 Focused Update Adopted by the ASAM Board of Directors December 18, 2019. © Copyright 2020. American Society of Addiction Medicine, Inc. All rights reserved. Permission to make digital or hard copies of this work for personal or classroom use is granted without fee provided that copies are not made or distributed for commercial, advertising or promotional purposes, and that copies bear this notice and the full citation on the fi rst page. Republication, systematic reproduction, posting in electronic form on servers, redistribution to lists, or other uses of this material, require prior specifi c written permission or license from the Society. American Society of Addiction Medicine 11400 Rockville Pike, Suite 200 Rockville, MD 20852 Phone: (301) 656-3920 Fax (301) 656-3815 E-mail: [email protected] www.asam.org CLINICAL PRACTICE GUIDELINE The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update 2020 Focused Update Guideline Committee members Kyle Kampman, MD, Chair (alpha order): Daniel Langleben, MD Chinazo Cunningham, MD, MS, FASAM Ben Nordstrom, MD, PhD Mark J. Edlund, MD, PhD David Oslin, MD Marc Fishman, MD, DFASAM George Woody, MD Adam J. Gordon, MD, MPH, FACP, DFASAM Tricia Wright, MD, MS Hendre´e E. Jones, PhD Stephen Wyatt, DO Kyle M. Kampman, MD, FASAM, Chair 2015 ASAM Quality Improvement Council (alpha order): Daniel Langleben, MD John Femino, MD, FASAM Marjorie Meyer, MD Margaret Jarvis, MD, FASAM, Chair Sandra Springer, MD, FASAM Margaret Kotz, DO, FASAM George Woody, MD Sandrine Pirard, MD, MPH, PhD Tricia E. -

What Are the Treatments for Heroin Addiction?
How is heroin linked to prescription drug abuse? See page 3. from the director: Research Report Series Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a devastating impact on society and cost billions of dollars each year. Although heroin use in the general population is rather low, the numbers of people starting to use heroin have been steadily rising since 2007.1 This may be due in part to a shift from abuse of prescription pain relievers to heroin as a readily available, cheaper alternative2-5 and the misperception that highly pure heroin is safer than less pure forms because it does not need to be injected. Like many other chronic diseases, addiction can be treated. Medications HEROIN are available to treat heroin addiction while reducing drug cravings and withdrawal symptoms, improving the odds of achieving abstinence. There are now a variety of medications that can be tailored to a person’s recovery needs while taking into account co-occurring What is heroin and health conditions. Medication combined with behavioral therapy is particularly how is it used? effective, offering hope to individuals who suffer from addiction and for those around them. eroin is an illegal, highly addictive drug processed from morphine, a naturally occurring substance extracted from the seed pod of certain varieties The National Institute on Drug Abuse (NIDA) has developed this publication to Hof poppy plants. -

Suicides Due to Alcohol And/Or Drug Overdose
Suicides Due to Alcohol and/or Drug Overdose A Data Brief from the National Violent Death Reporting System National Center for Injury Prevention and Control Division of Violence Prevention Background Suicide occurs when a person ends his or her own life. It is the 11th leading cause of death among NVDRS is a state-based system for Americans, and every year more than 33,000 providing detailed information about people end their own lives. Suicide is found in violent deaths, such as when, where, every age, racial, and ethnic group to differing and how they happen and other possible degrees (1). contributing factors. This information can be used to monitor homicides and There are a number of factors that increase the suicides and design and evaluate prevention likelihood a person will take his or her own life; strategies. Benefits of NVDRS include the one of these is abusing substances such as alcohol following: and drugs (1). Alcohol and drug abuse are second only to depression and other mood disorders as• Linked records describing the detailed the most frequent risk factors for suicidal behavior circumstances that may contribute to a (2, 3). Alcohol and some drugs can result in a loss violent death of inhibition, may increase impulsive behavior, can lead to changes in the brain that result in • Identification of violent deaths occurring depression over time, and can be disruptive to together to help describe the circumstance relationships— resulting in alienation and a loss of multiple homicides or homicide- of social connection (4). Furthermore, excessive suicides acute drug and/or alcohol ingestion could result in death. -
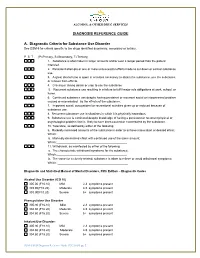
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b.