What Are the Treatments for Heroin Addiction?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Opioid Tolerance in Methadone Maintenance Treatment: Comparison
Gutwinski et al. Harm Reduction Journal (2016) 13:7 DOI 10.1186/s12954-016-0095-0 RESEARCH Open Access Opioid tolerance in methadone maintenance treatment: comparison of methadone and levomethadone in long-term treatment Stefan Gutwinski*, Nikola Schoofs, Heiner Stuke, Thomas G. Riemer, Corinde E. Wiers and Felix Bermpohl Abstract Background: This study aimed to investigate the development of opioid tolerance in patients receiving long-term methadone maintenance treatment (MMT). Methods: A region-wide cross-sectional study was performed focusing on dosage and duration of treatment. Differences between racemic methadone and levomethadone were examined. All 20 psychiatric hospitals and all 110 outpatient clinics in Berlin licensed to offer MMT were approached in order to reach patients under MMT fulfilling the DSM IV criteria of opiate dependence. In the study, 720 patients treated with racemic methadone or levomethadone gave information on the dosage of treatment. Out of these, 679 patients indicated the duration of MMT. Results: Treatment with racemic methadone was reported for 370 patients (54.5 %), with levomethadone for 309 patients (45.5 %). Mean duration of MMT was 7.5 years. We found a significant correlation between dosage and duration of treatment, both in a conjoint analysis for the two substances racemic methadone and levomethadone and for each substance separately. These effects remained significant when only patients receiving MMT for 1 year or longer were considered, indicating proceeding tolerance development in long-term treatment. When correlations were compared between racemic methadone and levomethadone, no significant difference was found. Conclusions: Our data show a tolerance development under long-term treatment with both racemic methadone and levomethadone. -

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -

Nitrous Oxide in Emergency Medicine Í O’ Sullivan, J Benger
214 ANALGESIA Emerg Med J: first published as 10.1136/emj.20.3.214 on 1 May 2003. Downloaded from Nitrous oxide in emergency medicine Í O’ Sullivan, J Benger ............................................................................................................................. Emerg Med J 2003;20:214–217 Safe and predictable analgesia is required for the identify these zones as there is considerable vari- potentially painful or uncomfortable procedures often ation between people. He also emphasised the importance of the patient’s pre-existing beliefs. If undertaken in an emergency department. The volunteers expect to fall asleep while inhaling characteristics of an ideal analgesic agent are safety, 30% N2O then a high proportion do so. An appro- predictability, non-invasive delivery, freedom from side priate physical and psychological environment increases the actions of N2O and may allow lower effects, simplicity of use, and a rapid onset and offset. doses to be more effective. Unlike many other Newer approaches have threatened the widespread use anaesthetic agents, N2O exhibits an acute toler- of nitrous oxide, but despite its long history this simple ance effect, whereby its potency is greater at induction than after a period of “accommoda- gas still has much to offer. tion”. .......................................................................... MECHANISM OF ACTION “I am sure the air in heaven must be this Some writers have suggested that N2O, like wonder-working gas of delight”. volatile anaesthetics, causes non-specific central nervous system depression. Others, such as 4 Robert Southey, Poet (1774 to 1843) Gillman, propose that N2O acts specifically by interacting with the endogenous opioid system. HISTORY N2O is known to act preferentially on areas of the Nitrous oxide (N2O) is the oldest known anaes- brain and spinal cord that are rich in morphine thetic agent. -

National Vital Statistics Report: Drugs Most Frequently Involved In
National Vital Statistics Reports Volume 67, Number 9 December 12, 2018 Drugs Most Frequently Involved in Drug Overdose Deaths: United States, 2011–2016 by Holly Hedegaard, M.D., M.S.P.H., and Brigham A. Bastian, B.S., National Center for Health Statistics; James P. Trinidad, M.P.H., M.S., U.S. Food and Drug Administration; Merianne Spencer, M.P.H., and Margaret Warner, Ph.D., National Center for Health Statistics Abstract overdose deaths involving methadone decreased from 1.4 per 100,000 in 2011 to 1.1 in 2016. The 10 most frequently Objective—This report identifies the specific drugs involved mentioned drugs often were found in combination with each most frequently in drug overdose deaths in the United States other. The drugs most frequently mentioned varied by the intent from 2011 through 2016. of the drug overdose death. In 2016, the drugs most frequently Methods—Record-level data from the 2011–2016 National mentioned in unintentional drug overdose deaths were fentanyl, Vital Statistics System–Mortality files were linked to electronic heroin, and cocaine, while the drugs most frequently mentioned files containing literal text information from death certificates. in suicides by drug overdose were oxycodone, diphenhydramine, Drug overdose deaths were identified using the International hydrocodone, and alprazolam. Classification of Diseases, Tenth Revision underlying cause- Conclusions—This report identifies patterns in the specific of-death codes X40–X44, X60–X64, X85, and Y10–Y14. Drug drugs most frequently involved in drug overdose deaths from mentions were identified by searching the literal text in three 2011 through 2016 and highlights the importance of complete fields of the death certificate: the causes of death from Part I, and accurate reporting in the literal text on death certificates. -

Opioid Receptorsreceptors
OPIOIDOPIOID RECEPTORSRECEPTORS defined or “classical” types of opioid receptor µ,dk and . Alistair Corbett, Sandy McKnight and Graeme Genes encoding for these receptors have been cloned.5, Henderson 6,7,8 More recently, cDNA encoding an “orphan” receptor Dr Alistair Corbett is Lecturer in the School of was identified which has a high degree of homology to Biological and Biomedical Sciences, Glasgow the “classical” opioid receptors; on structural grounds Caledonian University, Cowcaddens Road, this receptor is an opioid receptor and has been named Glasgow G4 0BA, UK. ORL (opioid receptor-like).9 As would be predicted from 1 Dr Sandy McKnight is Associate Director, Parke- their known abilities to couple through pertussis toxin- Davis Neuroscience Research Centre, sensitive G-proteins, all of the cloned opioid receptors Cambridge University Forvie Site, Robinson possess the same general structure of an extracellular Way, Cambridge CB2 2QB, UK. N-terminal region, seven transmembrane domains and Professor Graeme Henderson is Professor of intracellular C-terminal tail structure. There is Pharmacology and Head of Department, pharmacological evidence for subtypes of each Department of Pharmacology, School of Medical receptor and other types of novel, less well- Sciences, University of Bristol, University Walk, characterised opioid receptors,eliz , , , , have also been Bristol BS8 1TD, UK. postulated. Thes -receptor, however, is no longer regarded as an opioid receptor. Introduction Receptor Subtypes Preparations of the opium poppy papaver somniferum m-Receptor subtypes have been used for many hundreds of years to relieve The MOR-1 gene, encoding for one form of them - pain. In 1803, Sertürner isolated a crystalline sample of receptor, shows approximately 50-70% homology to the main constituent alkaloid, morphine, which was later shown to be almost entirely responsible for the the genes encoding for thedk -(DOR-1), -(KOR-1) and orphan (ORL ) receptors. -

Adolescent Drug Terminology and Trends: 2017-18 Edition
Adolescent Drug Terminology and Trends: 2017-18 Edition Matthew Quinn, LCPC, CADC Community Relations Coordinator Vaping Term used to describe when a substance is heated to the point of releasing vapor but not combusted (lit on fire). • Increasing in popularity as a way to ingest nicotine and cannabis, often in an electronic device that looks like a pen • Usually relatively odorless and difficult to distinguish between nicotine and cannabis vape device Juul (pronounced jewel) Specific vaping product from Pax Labs similar to an e- cigarette used to ingest nicotine • Liquid contains nicotine salts extracted from the tobacco leaf (2x nicotine of previous e-cigs) • Variety of flavors • Cool mint • Mango • Crème brule Dabs Dabs is a highly concentrated butane hash oil (BHO) created in a process where high quality cannabis is blasted with butane and extracted. • Heated and inhaled • Contains 70-90% THC compared to 5-15% THC in regular cannabis • Wax, oil, shatter, crumble • Sauce, distillate Rig A rig is a device used to vaporize and inhale dabs. • Looks similar to a water pipe or bong • Usually a nail is heated with a hand- held torch to a high temperature and a small piece of the concentrate is ‘dabbed’ onto a nail • Vapor released is then inhaled through the pipe Edibles • Increasingly popular alternative to smoking marijuana • Produced to infuse marijuana into various ingestible forms • Problem is that effects are hard to predict and difficult to know dose Other Terms for Cannabis • Bud • Dank • Nug • Loud • Fire • Gas Bars (Ladders) Another name for the rectangular shaped Xanax (anti- anxiety medication) with three lines in them (typically 2mg per ‘bar’). -

Skin Manifestations of Illicit Drug Use Manifestações Cutâneas
RevABDV81N4.qxd 12.08.06 13:10 Page 307 307 Educação Médica Continuada Manifestações cutâneas decorrentes do uso de drogas ilícitas Skin manifestations of illicit drug use Bernardo Gontijo 1 Flávia Vasques Bittencourt 2 Lívia Flávia Sebe Lourenço 3 Resumo: O uso e abuso de drogas ilícitas é um problema significativo e de abrangência mun- dial. A Organização das Nações Unidas estima que 5% da população mundial entre os 15 e 64 anos fazem uso de drogas pelo menos uma vez por ano (prevalência anual), sendo que meta- de destes usam regularmente, isto é, pelo menos uma vez por mês. Muitos dos eventos adver- sos das drogas ilícitas surgem na pele, o que torna fundamental que o dermatologista esteja familiarizado com essas alterações. Palavras-chave: Drogas ilícitas; Drogas ilícitas/história; Drogas ilícitas/efeitos adversos; Pele; Revisão Abstract: Illicit drug use and abuse is a major problem all over the world. The United Nations estimates that 5% of world population (aged 15-64 years) use illicit drugs at least once a year (annual prevalence) and half of them use drugs regularly, that is, at least once a month. Many adverse events of illicit drugs arise on the skin and therefore dermatologists should be aware of these changes. Keywords: Street drugs; Street drugs/history; Street drugs/adverse effects; Skin; Review HISTÓRICO Há mais de cinco mil anos na Mesopotâmia, minorar o sofrimento dos condenados. região onde hoje se situa o Iraque, os poderes cal- Provavelmente seja o ópio a droga nephente à qual mantes, soníferos e anestésicos do ópio (do latim Homero se referia como “o mais poderoso destrui- opium, através do grego opion, ‘seiva, suco’) já eram dor de mágoas”.1,2 conhecidos pelos sumérios. -
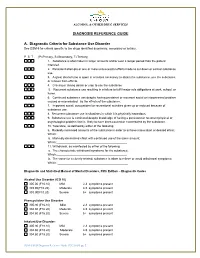
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b. -
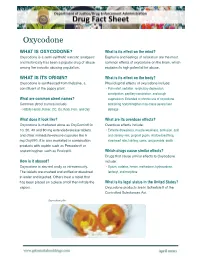
Drug Fact Sheet: Oxycodone
Oxycodone WHAT IS OXYCODONE? What is its effect on the mind? Oxycodone is a semi-synthetic narcotic analgesic Euphoria and feelings of relaxation are the most and historically has been a popular drug of abuse common effects of oxycodone on the brain, which among the narcotic abusing population. explains its high potential for abuse. WHAT IS ITS ORIGIN? What is its effect on the body? Oxycodone is synthesized from thebaine, a Physiological effects of oxycodone include: constituent of the poppy plant. • Pain relief, sedation, respiratory depression, constipation, papillary constriction, and cough What are common street names? suppression. Extended or chronic use of oxycodone Common street names include: containing acetaminophen may cause severe liver • Hillbilly Heroin, Kicker, OC, Ox, Roxy, Perc, and Oxy damage What does it look like? What are its overdose effects? Oxycodone is marketed alone as OxyContin® in Overdose effects include: 10, 20, 40 and 80 mg extended-release tablets • Extreme drowsiness, muscle weakness, confusion, cold and other immediate-release capsules like 5 and clammy skin, pinpoint pupils, shallow breathing, mg OxyIR®. It is also marketed in combination slow heart rate, fainting, coma, and possible death products with aspirin such as Percodan® or acetaminophen such as Roxicet®. Which drugs cause similar effects? Drugs that cause similar effects to Oxycodone How is it abused? include: Oxycodone is abused orally or intravenously. • Opium, codeine, heroin, methadone, hydrocodone, The tablets are crushed and sniffed or dissolved fentanyl, and morphine in water and injected. Others heat a tablet that has been placed on a piece of foil then inhale the What is its legal status in the United States? vapors. -

NIDA Modified ASSIST (Pdf)
1 NIDA Quick Screen V1.0F Name: ......................................................................... Sex ( ) F ( ) M Age....... Interviewer........................................ Date ....../....../...... Introduction (Please read to patient) Hi, I’m __________, nice to meet you. If it’s okay with you, I’d like to ask you a few questions that will help me give you better medical care. The questions relate to your experience with alcohol, cigarettes, and other drugs. Some of the substances we’ll talk about are prescribed by a doctor (like pain medications). But I will only record those if you have taken them for reasons or in doses other than prescribed. I’ll also ask you about illicit or illegal drug use––but only to better diagnose and treat you. Instructions: For each substance, mark in the appropriate column. For example, if the patient has used cocaine monthly in the past year, put a mark in the “Monthly” column in the “illegal drug” row. NIDA Quick Screen Question: In the past year, how often have you used the following? Daily Twice Never Almost Almost Weekly Daily or Once or Monthly Alcohol • For men, 5 or more drinks a day • For women, 4 or more drinks a day Tobacco Products Prescription Drugs for Non-Medical Reasons Illegal Drugs . If the patient says “NO” for all drugs in the Quick Screen, reinforce abstinence. Screening is complete. If the patient says “Yes” to one or more days of heavy drinking, patient is an at-risk drinker. Please see NIAAA website “How to Help Patients Who Drink Too Much: A Clinical Approach” http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm, for information to Assess, Advise, Assist, and Arrange help for at risk drinkers or patients with alcohol use disorders . -

The Effects of the Morphine Analogue Levorphanol on Leukocytes: Metabolic Effects at Rest and During Phagocytosis
The effects of the morphine analogue levorphanol on leukocytes: Metabolic effects at rest and during phagocytosis Nancy Wurster, … , Penelope Pettis, Sharon Lebow J Clin Invest. 1971;50(5):1091-1099. https://doi.org/10.1172/JCI106580. Studies on bacteria have suggested that morphine-like drugs have effects on the cell membrane. To determine the effect of this class of drugs on a mammalian cell, we selected the rabbit peritoneal exudate granulocyte, which undergoes striking membrane changes during phagocytosis. We examined the effect in vitro of the morphine analogue, levorphanol on phagocytosis and metabolism by granulocytes incubated with and without polystyrene particles or live Escherichia coli. Levorphanol (1 or 2 mmoles/liter) decreased: (a) acylation of lysolecithin or lysophosphatidylethanolamine in the medium (which is stimulated about two-fold during phagocytosis) both at rest (40%) and during phagocytosis (60%); (b) uptake of latex particles and Escherichia coli, as judged by electron microscopy; (c) killing of live Escherichia coli (10-fold); (d) 14 14 + CO2 production from glucose-1- C during phagocytosis by at least 80%; (e) K content of granulocytes (35%); (f) oxidation of linoleate-1-14C by 50%, and its incorporation into triglyceride by more than 80%. However, levorphanol stimulated 2 to 3-fold the incorporation of linoleate-1-14C or palmitate-1-14C into several phospholipids. Glucose uptake, lactate production, and adenosine triphosphate (ATP) content are not affected by the drug. Thus, levorphanol does not appear to exert its effects through generalized metabolic suppression. Removal of levorphanol by twice resuspending the granulocytes completely reverses all inhibition. In line with observations on bacteria, it appears that the complex effects of levorphanol on […] Find the latest version: https://jci.me/106580/pdf The Effects of the Morphine Analogue Levorphanol on Leukocytes METABOLIC EFFECTS AT REST AND DURING PHAGOCYTOSIS NANcY WuRsTE, PETER ELSBACH, ERIc J. -

Surveillance of Drug Abuse Trends in the State of Ohio January - June 2019
OSAMOSAM OhioOhio Substance Substance Abuse Abuse Monitoring Monitoring Network Network SurveillanceSurveillance of of Drug Drug Abuse Abuse Trends Trends in the State of Ohio January - June 2019 Lake Ashtabula Fulton Lucas Williams Ottawa Geauga Cuyahoga Defiance Henry Wood Sandusky Erie Lorain Trumbull Huron Summit Portage Paulding Seneca Medina Putnam Hancock Mahoning Van Wert Wyandot Crawford Ashland Wayne Stark Columbiana Allen Richland Hardin Marion Mercer Auglaize Holmes Carroll Morrow Tuscarawas Jefferson Logan Knox Shelby Union Delaware Coshocton Harrison Champaign Darke Licking Miami Guernsey Belmont Franklin Muskingum Clark Madison Montgomery Preble Fairfield Perry Noble Monroe Greene Pickaway Fayette Morgan Hocking Washington Butler Warren Clinton Ross Athens Vinton Hamilton Highland Clermont Pike Meigs Jackson Brown Adams Scioto Gallia Lawrence Legend Akron-Canton region Columbus region Athens region Dayton region Cincinnati region Toledo region Cleveland region Youngstown region Ohio Substance Abuse Monitoring Network Surveillance of Drug Abuse Trends in the State of Ohio January - June 2019 Prepared by: Ohio Department of Mental Health and Addiction Services Office of Quality, Planning and Research R. Thomas Sherba, OSAM Principal Investigator — PhD, MPH, LPCC Sarah Balser, OSAM Coordinator — MPH, MSW, LSW, CHES Jessica Linley, OSAM Quantitative Data Analyst — PhD, MSW, LSW Table of Contents OSAM-O-Gram....................................................................................................................................................................3