Wo 2007/101227 A2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Anti-UBXN11 Monoclonal Antibody, Clone 2C20 (DCABH-13904) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
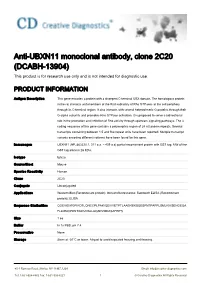
Anti-UBXN11 monoclonal antibody, clone 2C20 (DCABH-13904) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description This gene encodes a protein with a divergent C-terminal UBX domain. The homologous protein in the rat interacts with members of the Rnd subfamily of Rho GTPases at the cell periphery through its C-terminal region. It also interacts with several heterotrimeric G proteins through their G-alpha subunits and promotes Rho GTPase activation. It is proposed to serve a bidirectional role in the promotion and inhibition of Rho activity through upstream signaling pathways. The 3 coding sequence of this gene contains a polymoprhic region of 24 nt tandem repeats. Several transcripts containing between 1.5 and five repeat units have been reported. Multiple transcript variants encoding different isoforms have been found for this gene. Immunogen UBXN11 (NP_663320.1, 311 a.a. ~ 409 a.a) partial recombinant protein with GST tag. MW of the GST tag alone is 26 KDa. Isotype IgG2a Source/Host Mouse Species Reactivity Human Clone 2C20 Conjugate Unconjugated Applications Western Blot (Recombinant protein); Immunofluorescence; Sandwich ELISA (Recombinant protein); ELISA Sequence Similarities QGEVIDIRGPIRDTLQNCCPLPARIQEIVVETPTLAAERERSQESPNTPAPPLSMLRIKSENGEQA FLLMMQPDNTIGDVRALLAQARVMDASAFEIFS Size 1 ea Buffer In 1x PBS, pH 7.4 Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] -

Review UBX Domain Proteins: Major Regulators of the AAA Atpase
Cell. Mol. Life Sci. 65 (2008) 2360 – 2371 1420-682X/08/152360-12 Cellular and Molecular Life Sciences DOI 10.1007/s00018-008-8072-8 Birkhuser Verlag, Basel, 2008 Review UBX domain proteins: major regulators of the AAA ATPase Cdc48/p97 C. Schubertha,* and A. Buchbergerb,* a EMBL Heidelberg, Cell Biology and Biophysics Unit, Meyerhofstraße 1, 69117 Heidelberg (Germany), e-mail: [email protected] b Max Planck Institute of Biochemistry, Department of Molecular Cell Biology, Am Klopferspitz 18, 82152 Martinsried (Germany), e-mail: [email protected] Received 8 February 2008; received after revision 12 March 2008; accepted 14 March 2008 Online First 26 April 2008 Abstract. The highly conserved AAA ATPase Cdc48/ poral and spatial regulation of its activity. In combi- p97 acts on ubiquitylated substrate proteins in cellular nation with UBX-like proteins and other cofactors, processes as diverse as the fusion of homotypic they can assemble into a large variety of Cdc48/p97- membranes and the degradation of misfolded pro- cofactor complexes possessing distinct cellular func- teins. The Ubiquitin regulatory X (UBX) domain- tions. This review gives an overview of the different containing proteins constitute the so far largest family subfamilies of UBX proteins and their functions, and of Cdc48/p97 cofactors. UBX proteins are involved in discusses general principles of Cdc48/p97 regulation substrate recruitment to Cdc48/p97 and in the tem- by these cofactors. Keywords. AAA ATPase, valosin-containing protein (VCP), ubiquitin/proteasome system, protein degrada- tion, UBA domain, ubiquitin-like fold. Introduction UBX proteins in general are cofactors for Cdc48/p97 [6–9]. More than 10 years ago, a protein domain displaying Cdc48 (also known as p97 or VCP in mammals1) weak amino acid sequence homology to the small belongs to the family of AAA ATPases (ATPases protein modifier ubiquitin was identified in a number associated with various cellular activities) [10]. -

Wo 2010/065567 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 10 June 2010 (10.06.2010) WO 2010/065567 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 36/889 (2006.01) A61K 31/16 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 36/736 (2006.01) A61K 31/05 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, A61K 31/166 (2006.01) A61P 5/00 (2006.01) CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, PCT/US2009/066294 KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (22) International Filing Date: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 1 December 2009 (01 .12.2009) NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (25) Filing Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/1 18,945 1 December 2008 (01 .12.2008) US GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, (71) Applicant (for all designated States except US): LIFES¬ TM), European (AT, BE, BG, CH, CY, CZ, DE, DK, EE, PAN EXTENSION LLC [US/US]; 933 First Colonial ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, Road, Suite 114, Virginia Beach, VA 23454 (US). -

Global Patterns of Changes in the Gene Expression Associated with Genesis of Cancer a Dissertation Submitted in Partial Fulfillm
Global Patterns Of Changes In The Gene Expression Associated With Genesis Of Cancer A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy at George Mason University By Ganiraju Manyam Master of Science IIIT-Hyderabad, 2004 Bachelor of Engineering Bharatiar University, 2002 Director: Dr. Ancha Baranova, Associate Professor Department of Molecular & Microbiology Fall Semester 2009 George Mason University Fairfax, VA Copyright: 2009 Ganiraju Manyam All Rights Reserved ii DEDICATION To my parents Pattabhi Ramanna and Veera Venkata Satyavathi who introduced me to the joy of learning. To friends, family and colleagues who have contributed in work, thought, and support to this project. iii ACKNOWLEDGEMENTS I would like to thank my advisor, Dr. Ancha Baranova, whose tolerance, patience, guidance and encouragement helped me throughout the study. This dissertation would not have been possible without her ever ending support. She is very sincere and generous with her knowledge, availability, compassion, wisdom and feedback. I would also like to thank Dr. Vikas Chandhoke for funding my research generously during my doctoral study at George Mason University. Special thanks go to Dr. Patrick Gillevet, Dr. Alessandro Giuliani, Dr. Maria Stepanova who devoted their time to provide me with their valuable contributions and guidance to formulate this project. Thanks to the faculty of Molecular and Micro Biology (MMB) department, Dr. Jim Willett and Dr. Monique Vanhoek in embedding valuable thoughts to this dissertation by being in my dissertation committee. I would also like to thank the present and previous doctoral program directors, Dr. Daniel Cox and Dr. Geraldine Grant, for facilitating, allowing, and encouraging me to work in this project. -

Supplementary Data
SUPPLEMENTARY METHODS 1) Characterisation of OCCC cell line gene expression profiles using Prediction Analysis for Microarrays (PAM) The ovarian cancer dataset from Hendrix et al (25) was used to predict the phenotypes of the cell lines used in this study. Hendrix et al (25) analysed a series of 103 ovarian samples using the Affymetrix U133A array platform (GEO: GSE6008). This dataset comprises clear cell (n=8), endometrioid (n=37), mucinous (n=13) and serous epithelial (n=41) primary ovarian carcinomas and samples from 4 normal ovaries. To build the predictor, the Prediction Analysis of Microarrays (PAM) package in R environment was employed (http://rss.acs.unt.edu/Rdoc/library/pamr/html/00Index.html). When more than one probe described the expression of a given gene, we used the probe with the highest median absolute deviation across the samples. The dataset from Hendrix et al. (25) and the dataset of OCCC cell lines described in this manuscript were then overlaid on the basis of 11536 common unique HGNC gene symbols. Only the 99 primary ovarian cancers samples and the four normal ovary samples were used to build the predictor. Following leave one out cross-validation, a predictor based upon 126 genes was able to identify correctly the four distinct phenotypes of primary ovarian tumour samples with a misclassification rate of 18.3%. This predictor was subsequently applied to the expression data from the 12 OCCC cell lines to determine the likeliest phenotype of the OCCC cell lines compared to primary ovarian cancers. Posterior probabilities were estimated for each cell line in comparison to the following phenotypes: clear cell, endometrioid, mucinous and serous epithelial. -

A Role of Ubiquitin Regulatory X-Domain Containing Proteins (UBXN6) in Antiviral Immunity
Touro Scholar NYMC Student Theses and Dissertations Students 8-31-2019 A Role of Ubiquitin Regulatory X-Domain Containing Proteins (UBXN6) in Antiviral Immunity Harshada Ketkar Harshada Ketkar New York Medical College Follow this and additional works at: https://touroscholar.touro.edu/nymc_students_theses Part of the Immunology of Infectious Disease Commons, Medicine and Health Sciences Commons, and the Virology Commons Recommended Citation Ketkar, Harshada and Ketkar, Harshada, "A Role of Ubiquitin Regulatory X-Domain Containing Proteins (UBXN6) in Antiviral Immunity" (2019). NYMC Student Theses and Dissertations. 24. https://touroscholar.touro.edu/nymc_students_theses/24 This Doctoral Dissertation - Open Access is brought to you for free and open access by the Students at Touro Scholar. It has been accepted for inclusion in NYMC Student Theses and Dissertations by an authorized administrator of Touro Scholar. For more information, please contact [email protected]. A Role of Ubiquitin Regulatory X-Domain Containing Proteins (UBXN6) in Antiviral Immunity Harshada Ketkar A Thesis in the Program in Basic Medical Sciences Submitted to the Faculty of the Graduate School of Basic Medical Sciences in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy at New York Medical College 2019 ii Acknowledgments I want to thank my mentor Dr. Penghua Wang for all his help, encouragement and guidance. I thank him for his thoughtful suggestions in science and life. The completion of my Ph.D. would not have been possible without his support. Most importantly I thank him for having trust in me and building my confidence. Thanks to my committee! I thank, Dr. -
Verfahren Zur Bestimmung Von Stress
(19) *DE102009043485A120110331* (10) DE 10 2009 043 485 A1 2011.03.31 (12) Offenlegungsschrift (21) Aktenzeichen: 10 2009 043 485.2 (51) Int Cl.8: C12Q 1/68 (2006.01) (22) Anmeldetag: 30.09.2009 (43) Offenlegungstag: 31.03.2011 (71) Anmelder: (72) Erfinder: Henkel AG & Co. KGaA, 40589 Düsseldorf, DE Weiß, Thomas, Dr., 40591 Düsseldorf, DE; Ghosh, Robin, Dr., 40215 Düsseldorf, DE; Briese, Melanie, 40597 Düsseldorf, DE; Özka, Yasmin, 40225 Düsseldorf, DE Die folgenden Angaben sind den vom Anmelder eingereichten Unterlagen entnommen (54) Bezeichnung: Verfahren zur Bestimmung von Stress (57) Zusammenfassung: Die Erfindung betrifft ein Verfah- ren zur Bestimmung von Stress, insbesondere chronischem Stress, durch die Analyse von biologischem Material aus Haarfollikeln. DE 10 2009 043 485 A1 2011.03.31 Beschreibung [0001] Die Erfindung betrifft ein Verfahren zur Bestimmung von Stress, insbesondere chronischem Stress, durch die Analyse von biologischem Material aus Haarfollikeln. [0002] Chronischer Stress kann zahlreiche Gesundheitsstörungen hervorrufen, wobei die Ausprägung man- nigfaltig ist: Migräne, Asthma, Tinnitus, Allergien, Burnout, Depressionen, Herz-Kreislauf-Erkrankungen, Stö- rungen des Immunsystems, des Bewegungsapparats und der Fortpflanzungsfunktionen, Magen-Darm-Erkran- kungen, Hauterkrankungen oder Schmerz- und Schlafstörungen sind nur einige von vielen möglichen Erkran- kungen, bei denen Stress ein wichtiger Einflussfaktor sein kann. [0003] Nicht selten treten derartige Funktionsstörungen unmerklich ein, da tägliche Belastungen -

There Are 1393 Genes Significant by SAM with 90Th Percentile Confidence, the False Discovery Rate Among the 1393 Significant Genes Is 0.09968
Class 1 (NPM1 wild-type); Class 2 (NPM1 mutation). There are 1393 genes significant by SAM With 90th percentile confidence, the false discovery rate among the 1393 significant genes is 0.09968 . The delta value used to identify the significant genes is 0.78224 . The fudge factor for standard deviation is computed as 0.06115 . if ratio is >1 gene expression lower in NPM1mut 307 overlapping genes (overlap of genes lower expressed in NPM1mut and putative target genes) if ratio is <1 gene expression higher in NPM1mut rank, based Geom mean of Geom mean of Ratio of on p- ratios in class ratios in class geom Map value 1=wt 2=mut means Clone gene symbol_1 gene symbol_2 Description UG cluster Location 1 1,750 0,395 4,427 IMAGE:382787 TRH TRH TRH || Thyrotropin-releasing hormone || Hs.182231 || AA069596 || || 7200 || 98655 Hs.182231 3 MLLT3 || Myeloid/lymphoid or mixed-lineage leukemia (trithorax homolog, Drosophila); translocated to, 3 || 2 1,689 0,551 3,068 IMAGE:783998 MLLT3 MLLT3 Hs.493585 || AA443284 || || 4300 || 116155 Hs.591085 9 P2RY5 || Purinergic receptor P2Y, G-protein coupled, 5 || Hs.123464 || R91539 || purinergic receptor 3 1,866 0,497 3,754 IMAGE:196488 P2RY5 P2RY5 P2Y5=RB intorn-encoded putative G-protei || 10161 || 112029 Hs.123464 13 4 1,678 0,497 3,375 IMAGE:49923 BAALC BAALC BAALC || Brain and acute leukemia, cytoplasmic || Hs.533446 || H28986 || || 79870 || 311379 Hs.533446 8 5 1,611 0,612 2,634 IMAGE:416374 TSPAN13 TM4SF13 TM4SF13 || Tetraspanin 13 || Hs.364544 || W86201 || || 27075 || 226071 Hs.364544 7 6 1,770 0,557 3,179 -

A Systematic Proteomic Approach to the VCP/P97-Cofactor Interaction Landscape Reveals P97 Functions in Stress Response Signaling
A systematic proteomic approach to the VCP/p97-cofactor interaction landscape reveals p97 functions in stress response signaling Inaugural-Dissertation zur Erlangung des Doktorgrades Dr. rer. nat. der Fakultät für Biologie an der Universität Duisburg-Essen vorgelegt von Julia Hülsmann aus Lüdinghausen Dezember 2018 Die der vorliegenden Arbeit zugrunde liegenden Experimente wurden in der Abteilung für Molekularbiologie I am Zentrum für Medizinische Biotechnologie der Universität Duisburg- Essen durchgeführt. 1. Gutachter: Prof. Dr. Hemmo Meyer 2. Gutachter: Prof. Dr. Michael Ehrmann Vorsitzender des Prüfungsausschusses: Prof. Dr. Stefan Westermann Tag der mündlichen Prüfung: 11. März 2019 Diese Dissertation wird über DuEPublico, dem Dokumenten- und Publikationsserver der Universität Duisburg-Essen, zur Verfügung gestellt und liegt auch als Print-Version vor. DOI: 10.17185/duepublico/70049 URN: urn:nbn:de:hbz:464-20200317-124816-9 Alle Rechte vorbehalten. 2 Table of contents Table of contents List of figures 5 List of tables 7 Summary 8 Zusammenfassung 9 1 Introduction 11 1.1 Protein homeostasis 11 1.1.1 The integrated stress response 12 1.2 The ubiquitin proteasome system 15 1.3 The AAA+ ATPase p97 18 1.3.1 Structure and mechanism of p97 19 1.3.2 p97 inhibitors 20 1.3.3 Cellular processes associated with p97 and specific cofactors 21 1.3.4 The p97 cofactor system 26 1.3.4.1 Identification of distinct p97-cofactor complexes and substrate candidates based on proteomic studies 29 1.3.4.2 Basic principles of p97-cofactor complex assembly 30 -

EFFECTS of RADIATION EXPOSURE on LUNG CARCINOGENESIS APPROVED by SUPERVISORY COMMITTEE Jerry W. S
EFFECTS OF RADIATION EXPOSURE ON LUNG CARCINOGENESIS APPROVED BY SUPERVISORY COMMITTEE ______________________________ Jerry W. Shay, Ph.D. Professor of Cell Biology ______________________________ David A. Boothman, Ph.D. Professor Simmons Cancer Center ______________________________ John D. Minna, M.D. Professor of Internal Medicine ______________________________ Michael D. Story, Ph.D. Associate professor of Radiation Oncology DEDICATION Dedicated to my lovely wife Nikki for all of her love and support. EFFECTS OF RADIATION EXPOSURE ON LUNG CARCINOGENESIS by OLIVER DELGADO DISSERTATION Presented to the Faculty of the Graduate School of Biomedical Sciences The University of Texas Southwestern Medical Center at Dallas In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY The University of Texas Southwestern Medical Center at Dallas Dallas, Texas December, 2009 Copyright by OLIVER DELGADO, 2009 All Rights Reserved ACKNOWLEDGEMENTS I would like to acknowledge and thank first and foremost my mentors, Jerry Shay and Woody Wright. The complementarity of your distinctive thoughts and approaches provided me with an unparalleled environment to learn and mature as a young scientist. I would like to thank my thesis committee: Dr. David Boothman, Dr. John Minna, and Dr. Michael Story for their comments and support throughout the years. In addition, thank you to Dr. James Richardson who taught me to see the order within an H&E section. Thanks to all the current and former Shay/Wright lab members that have made my time in the lab both enjoyable and challenging. In particular, I would like to thank David Minna, Suzie Hight, Kimberly Batten, Erin Kitten, Phil Smiraldo, Andres Roig, Richard MacDonnell, Gail Marian, and Aadil Kaisani for their help and/or advice with one or all of my projects. -

A Dataset for the Analysis of Gene Expression and Alternative Splicing Events in Colon Disease Wilfrido Mojica1, Lesleyann Hawthorn2*
Mojica and Hawthorn BMC Genomics 2010, 11:5 http://www.biomedcentral.com/1471-2164/11/5 RESEARCH ARTICLE Open Access Normal colon epithelium: a dataset for the analysis of gene expression and alternative splicing events in colon disease Wilfrido Mojica1, Lesleyann Hawthorn2* Abstract Background: Studies using microarray analysis of colorectal cancer have been generally beleaguered by the lack of a normal cell population of the same lineage as the tumor cell. One of the main objectives of this study was to generate a reference gene expression data set for normal colonic epithelium which can be used in comparisons with diseased tissues, as well as to provide a dataset that could be used as a baseline for studies in alternative splicing. Results: We present a dependable expression reference data set for non-neoplastic colonic epithelial cells. An enriched population of fresh colon epithelial cells were obtained from non-neoplastic, colectomy specimens and analyzed using Affymetrix GeneChip EXON 1.0 ST arrays. For demonstration purposes, we have compared the data derived from these cells to a publically available set of tumor and matched normal colon data. This analysis allowed an assessment of global gene expression alterations and demonstrated that adjacent normal tissues, with a high degree of cellular heterogeneity, are not always representative of normal cells for comparison to tumors which arise from the colon epithelium. We also examined alternative splicing events in tumors compared to normal colon epithelial cells. Conclusions: The findings from this study represent the first comprehensive expression profile for non-neoplastic colonic epithelial cells reported. Our analysis of splice variants illustrate that this is a very labor intensive procedure, requiring vigilant examination of the data. -

WO 2010/065567 A3 10 June 2010 (10.06.2010) PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2010/065567 A3 10 June 2010 (10.06.2010) PCT (51) International Patent Classification: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, A61K36/889 (2006.01) A61K31/16 (2006.01) DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, A61K36/736 (2006.01) A61K31/05 (2006.01) HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, A61K31/166 (2006.01) A61P5/00 (2006.01) KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (21) International Application Number: NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, PCT/US2009/066294 SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (22) International Filing Date: TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. 1 December 2009 (01.12.2009) (84) Designated States (unless otherwise indicated, for every (25) Filing Language: English kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (26) Publication Language: English ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, TM), European (AT, BE, BG, CH, CY, CZ, DE, DK, EE, (30) Priority Data: 61/118,945 1 December 2008 (01.12.2008) US ES, FI, FR, GB, GR, HR, HU, IE, IS, ΓΓ, LT, LU, LV, MC, MK, MT, NL, NO, PL, PT, RO, SE, SI, SK, SM, (71) Applicant (for all designated States except US): LIFES TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, PAN EXTENSION LLC [US/US]; 933 First Colonial ML, MR, NE, SN, TD, TG).