Ankylosis of Permanent First Molar: Diagnosis by Cone Beam
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Concurrent Occurrence of Bilateral Hypodontia and Microdontia in a Nonsyndromic Paediatric Patient: a Case Report
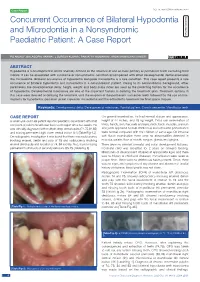
Case Report DOI: 10.7860/JCDR/2020/43540.14083 Concurrent Occurrence of Bilateral Hypodontia Dentistry Section and Microdontia in a Nonsyndromic Paediatric Patient: A Case Report PG ANJALI1, BALAGOpaL VARMA2, J SURESH KUMAR3, paRVATHY KUMARAN4, ARUN MAMACHAN XAVIER5 ABSTRACT Hypodontia is a developmental dental anomaly defined as the absence of one or more primary or permanent teeth excluding third molars. It can be associated with syndrome or nonsyndromic condition accompanied with other developmental dental anomalies like microdontia. Bilateral occurrence of hypodontia alongside microdontia is a rare condition. This case report presents a rare occurrence of bilateral hypodontia and microdontia in a nonsyndromic patient. Owing to its nonsyndromic background, other parameters like developmental delay, height, weight and body mass index are used as the predicting factors for the occurrence of hypodontia. Developmental milestones are one of the important factors in deriving the treatment plan. Treatment options in this case were directed at delaying the treatment until the eruption of the permanent successor teeth followed by the use of mini- implants for hypodontia, porcelain jacket crown for microdontia and the orthodontic treatment for final space closure. Keywords: Developmental delay, Developmental milestones, Familial pattern, Growth percentile, Mandibular teeth CASE REPORT On general examination, he had normal stature and appearance, A seven-year-old male patient reported paediatric department with chief height of 44 inches, and 18 kg weight. Extra oral examination of complaint of pain in the left lower back tooth region since two weeks. He limbs, hands, skin, hair, nails and eyes, neck, back, muscles, cranium was clinically diagnosed with multiple deep dental caries (74,75,84,85) and joints appeared normal. -

Ankylosed Primary Molars, Andlaw (1974) Described Surface Defects from Bicuspids Preceded by Non-Ankylosed 11 Molars
PEDIATRICDENTISTRY/Copyright (~) 1980 The AmericanAcademy of Pedodontics/Vol. 2, No, 1 Ankylosedprimary mola.rs: Results and treatment recommendat,onsfrom an eight-year longitudinal study Louise Brearley Messer,B.D.Sc., L.D.S., M.D.Sc. Jay T. Cline, D.D.S., M.A. Abstract continues concomitantly with vertical alveolar bone growth,~,3 and the tooth is immobile to manual rock- A total of 263 ankyloscd primarymolars in 107 ing.4,5 children aged three to 12 years was studied for four years. Forty-six children remainedin the study for eight years. The etiology of the condition remains unknown. Extrinsic causative factors implicated are local me- Observationof affected dentitions showedthat the con- ~ ~ dition waslikely to recur. Threeclinical pa~ternsfor the chanical trauma, disturbed local metabolism, local- condition are described. Typically, maxillary molars be- ized infection, 6 chemical or thermal irritation 7 and came ankylosed earlier and demonstrated more severe tooth reimplantation, s Intrinsic factors cited include a in[raocclusion than mandibularmolars. Mandibularfirst genetic or congenital gap in the periodontal liga- molars usually remainedslightly or moderatelyin#a- ment. Since both erupting and exfoliating teeth show occluded; mandibularsecond molars and maxillary first alternating periods of resorption and deposition of and second molars showedprogressively severe infra- bone and cementum,° aberrant deposition of these tis- occlusion. Followingeither extraction or ex~oliation of the suesI° may produce an area of ankylosing tissue.Z, affected molars, the succedaneousbicuspids did not differ In a summaryof studies reporting the prevalence of in either coronal morphologyor in distribution of enamel ankylosed primary molars, Andlaw (1974) described surface defects from bicuspids preceded by non-ankylosed 11 molars. -

Pharmacology of Local Anesthesia
By Mohammad Hussein Zaki Lecturer Oral & Maxillofacial Surgery Faculty of Dentistry – Minia University . Impacted tooth. Failure of the tooth to fully erupt into the oral cavity within its expected developmental time period and can no longer reasonably be expected to do so. A tooth that can not, or will not, erupt into its normal functioning positions. Impacted tooth. An impacted tooth is one that is erupted, partially erupted or unerupted and will not eventually assume a normal arch relationship with the other teeth and tissues. Unerupted tooth. Includes impacted teeth and teeth that are in the process of erupting. Impacted teeth seen in the following order of frequency: 1. Mandibular third molars. 2. Maxillary third molars. 3. Maxillary canine. 4. Mandibular premolar. 5. Maxillary premolar. 6. Mandibular canine. 7. Maxillary central incisors. 8. Maxillary lateral incisors. Systemic factors: • Syndromes. Cleidocranial dysplasia. • Endocrine deficiencies. Hypothyroidism. • Irradiation. Local factors: • Obstruction for eruption. Irregularity in position of an adjacent tooth. Density of the overlying soft tissue or bone. Prolonged deciduous tooth retention. Supernumerary teeth. • Tooth ankylosis. • Dilaceration of roots. • Malposed tooth germs. Local factors: • Pathological lesions. • Cleft lip and palate. • Arch-length deficiency. Phylogenic theory. Mendelian theory. Clinical. Radiographic. • Periapical. Radiographic. • Periapical. Radiographic. • Occlusal. Radiographic. • Panorama. Radiographic. • Panorama. Radiographic. • CT. Radiographic. • CBCT. Impacted teeth other than third molars. Exposure. • A procedure that allows natural eruption of impacted teeth. • It should be done as soon as it is determined that the tooth is not going to erupt spontaneously. • Spontaneous eruption versus orthodontic assistance. Impacted teeth other than third molars. Exposure. Impacted teeth other than third molars. -

Eruption Abnormalities in Permanent Molars: Differential Diagnosis and Radiographic Exploration
DOI: 10.1051/odfen/2014054 J Dentofacial Anom Orthod 2015;18:403 © The authors Eruption abnormalities in permanent molars: differential diagnosis and radiographic exploration J. Cohen-Lévy1, N. Cohen2 1 Dental surgeon, DFO specialist 2 Dental surgeon ABSTRACT Abnormalities of permanent molar eruption are relatively rare, and particularly difficult to deal with,. Diagnosis is founded mainly on radiographs, the systematic analysis of which is detailed here. Necessary terms such as non-eruption, impaction, embedding, primary failure of eruption and ankylosis are defined and situated in their clinical context, illustrated by typical cases. KEY WORDS Molars, impaction, primary failure of eruption (PFE), dilaceration, ankylosis INTRODUCTION Dental eruption is a complex developmen- at 0.08% for second maxillary molars and tal process during which the dental germ 0.01% for first mandibular molars. More re- moves in a coordinated fashion through cently, considerably higher prevalence rates time and space as it continues the edifica- were reported in retrospective studies based tion of the root; its 3-dimensional pathway on orthodontic consultation records: 2.3% crosses the alveolar bone up to the oral for second molar eruption abnormalities as epithelium to reach its final position in the a whole, comprising 1.5% ectopic eruption, occlusion plane. This local process is regu- 0.2% impaction and 0.6% primary failure of lated by genes expressing in the dental fol- eruption (PFE) (Bondemark and Tsiopa4), and licle, at critical periods following a precise up to 1.36% permanent second molar iim- chronology, bilaterally coordinated with fa- paction according to Cassetta et al.6. cial growth. -

Oral Pathology and Oral Microbiology
3.3.2 SYLLABUS ( Including Teaching Hours.) MUST KNOW 109 HRS 1 Developmental Disturbances of oral and paraoral structures 03 HRS Developmental disturbances of hard tissues: -dental arch relations, -disturbances related to - -size,shape,number and structure of teeth, -disturbances related to eruption and shedding. Developmental disturbances of soft tissues: Lip,palate,oral mucosa,gingival,tongue and salivary glands Craniofacial anomalies 2 Benign and Malignant tumors of oral cavity 25 HRS Potentially Malignant Disorders of epithelial tissue origin. -Definitions and nomenclature -Epithelial dysplasia -Lesions and conditions:leukoplakia, erythroplakia,oral lichen planus and oral submucous fibrosis. Benign tumors of epithelial tissue origin. - Squamous papilloma, Oral nevi. Malignant tumors of epithelial tissue origin. -Oral squamous cell carcinoma: Definition and nomenclature,etiopathogenesis, TNM staging ,Broder’s and Bryne’s grading systems. -Verrucous carcinoma -Basal cell carcinoma: Definition etiopathogenesis and histopathology -Malignant melanoma: Definition etiopathogenesis and histopathology Benign and malignant tumors of connective tissue -Fibroblast origin:oral fibromas and fibromatosis,peripheral ossifying fibroma peripheral giant cell granuloma, pyogenic granuloma and Fibrosarcoma -Adipose tissue origin:Lipoma -Endothelial origin(blood and lymphatics: Hemangiomas and lymphangiomas, Hereditary hemorrhagic telangiactasia, Kaposi’s sarcoma Bone and cartilage: Chondroma,osteoma,osteoid osteoma, benign osteoblastoma, osteosarcoma, -

Section I the Patient BLUK133-Jacobsen December 7, 2007 16:38
BLUK133-Jacobsen December 7, 2007 16:38 Section I The Patient BLUK133-Jacobsen December 7, 2007 16:38 “I’m ready when you are.” 2 BLUK133-Jacobsen December 7, 2007 16:38 Chapter 1 The Patient – His Limitations and Expectations Section I The provision of high-quality restorative dentistry depends upon the dentist: Making an accurate diagnosis Devising a comprehensive and realistic treatment plan Executing the treatment plan to a high technical standard Providing subsequent continuing care There is a very strong tendency, particularly in the and here re-education is often necessary to bring him field of fixed prosthodontics, for the dentist to become down to the practical and feasible. over-interested in the technical execution of treat- It might be that the dentist has the skills and tech- ment. There is a vast range of materials and equip- nical facilities to perform advanced procedures, but ment to stimulate this interest and compete for his before he puts bur to tooth, he must stop and ask attention. It is perhaps inevitable that dentists can be- whether this is really what this patient needs and come obsessive about types of bur or root canal file, wants. If the answer is no, then to proceed is an act the pros and cons of various materials and the precise of pure selfishness that might also be regarded as techniques of restoration. negligent! This is not to decry such interest because a high Certainly the dentist may have certain treatment standard of technical execution is essential for the goals for all his patients – no pain or caries, healthy longevity of restorations. -
Gracis S. a Simplified Method to Develop An
CLINICAL RESEARCH A simplified method to develop an interdisciplinary treatment plan: an esthetically and functionally driven approach in three steps Stefano Gracis, DMD, MSD Private Practice, Milan, Italy Correspondence to: Dr Stefano Gracis Via Brera 28/a, 20121 Milan, Italy; Tel: +39 02 72094471; Email: [email protected] 76 | The International Journal of Esthetic Dentistry | Volume 16 | Number 1 | Spring 2021 GRACIS Abstract typically required. This article provides a practical step- by-step approach to planning comprehensive interdis- Many clinicians are unsure of how to develop a com- ciplinary treatment focused primarily on the teeth as prehensive plan of treatment for patients who present they relate to each other and to the structures that with multiple problems and pathologies. In order to surround them. The approach is based on the answers efficiently plan appropriate treatment for such com- to six questions that are grouped into three steps: 1) plex patient cases, the clinician needs to either have or evaluation of the teeth relative to the face and lips; develop the necessary knowledge of evidence-based 2) assessment of anterior tooth dimensions; and 3) information on the predictability of available clinical analysis of the anteroposterior and maxillomandibular procedures. The clinician also needs to understand relationships. The information obtained must then be the correct sequence in which such treatment is ap- related to the patient’s skeletal framework, periodontal plied, and perfect the skills required for carrying out status, caries susceptibility, and biomechanical risk as- that treatment. Since most clinicians have not ac- sessment in order to formulate a clear and complete quired all the knowledge and skills necessary for this plan of treatment. -

Iatrogenic Mandibular Fractures Following Removal of Impacted Third
Iatrogenic mandibular IN BRIEF • Serves as a reminder of a rare but significant complication. PRACTICE fractures following removal • Highlights timing and presentation of the event. • Summarises potential risk factors and measures to minimise them. of impacted third molars: • Describes the treatment options. • Illustrates the role of the dentist in an analysis of 130 cases the management. M. Ethunandan,1 D. Shanahan2 and M. Patel3 VERIFIABLE CPD PAPER Immediate and late mandibular fractures are a rare complication of third molar removal. We analysed 130 cases of mandibular fractures following removal of impacted third molars reported in the literature, including four managed in the maxillofacial unit and identified potential risk factors. Its occurrence is likely to be multi-factorial, with age, gender, angulation, laterality, extent and degree of impaction and associated pathologies contributing to the risk of fracture. Postoperative fractures were more common than intra-operative fractures (2.7:1) and occurred most frequently in the second and third weeks (57%). A ‘cracking’ noise was the most frequent presentation (77%). Intra-operative fractures were more frequent among females (M:F – 1:1.3), and differed from postoperative fractures (M:F – 3.9:1). This study analyses the results, providing suggestions to minimise the risk and to manage a mandibular fracture following removal of a third molar. INTRODUCTION seek to identify potential risk factors and Removal of third molars is a common preventive measures. surgical procedure carried out by a den- tal surgeon and can result in a variety MATERIALS AND METHODS complications, which include dry socket, We undertook a Medline search cover- bleeding, infection, trismus and nerve ing the period 1970–2011 and identified damage.1–3 Mandibular fracture is rare, English articles in the literature, which but a very serious complication following reported the occurrence of mandibu- Fig. -

An Investigation Into the Role of Rankl and Sclerostin in Dentoalveolar Ankylosis
AN INVESTIGATION INTO THE ROLE OF RANKL AND SCLEROSTIN IN DENTOALVEOLAR ANKYLOSIS A thesis submitted in partial fulfilment of the requirements for the degree of Doctor of Clinical Dentistry (Orthodontics) Dr Shelley Coburn, BDS (University of Otago) Orthodontic Unit School of Dentistry Faculty of Health Science The University of Adelaide South Australia AUSTRALIA June 2015 1 CONTENTS 1.1 Table of Contents 1 CONTENTS .............................................................................................................. 2 1.1 Table of Contents ............................................................................................... 2 1.2 List of Figures .................................................................................................... 5 1.3 List of Tables ...................................................................................................... 6 1.4 List of abbreviations ........................................................................................... 8 2 ACKNOWLEDGEMENTS ....................................................................................... 10 3 THESIS DECLARATION ........................................................................................ 11 4 ABSTRACT ............................................................................................................ 12 5 LITERATURE REVIEW .......................................................................................... 15 5.1 The Periodontal Complex ................................................................................ -

Statistical Analysis Plan
Cover Page for Statistical Analysis Plan Sponsor name: Novo Nordisk A/S NCT number NCT03061214 Sponsor trial ID: NN9535-4114 Official title of study: SUSTAINTM CHINA - Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Document date: 22 August 2019 Semaglutide s.c (Ozempic®) Date: 22 August 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL Clinical Trial Report Status: Final Appendix 16.1.9 16.1.9 Documentation of statistical methods List of contents Statistical analysis plan...................................................................................................................... /LQN Statistical documentation................................................................................................................... /LQN Redacted VWDWLVWLFDODQDO\VLVSODQ Includes redaction of personal identifiable information only. Statistical Analysis Plan Date: 28 May 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL UTN:U1111-1149-0432 Status: Final EudraCT No.:NA Page: 1 of 30 Statistical Analysis Plan Trial ID: NN9535-4114 Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Author Biostatistics Semaglutide s.c. This confidential document is the property of Novo Nordisk. No unpublished information contained herein may be disclosed without prior written approval from Novo Nordisk. Access to this document must be restricted to relevant parties.This -

CHAPTER 21 Adult Interdisciplinary Therapy: Diagnosis and Treatment 575
CHAPTER 21 Adult Interdisciplinary Therapy: Diagnosis and Treatment 575 A B C D E F G H I J K L M FIGURE 21-6 Clinical example of adult treatment objective 3: redistribution of occlusal and incisal forces. A, No natural tooth stops in a 45-year-old woman. The initial tooth contact in centric rela- tion was between the mandibular first premolar and the maxillary second premolar.B, Anteriorly, the mandible fits within the maxillary arch. C, No tooth contact on the left side. D, Soft tissue indentations indicate the location of lower incisor contact with the palate. E, Severe maxillary pro- trusion. A Hawley bite plane was used to locate centric relation at the acceptable vertical. F, After maxillary and mandibular alignment, a splint was placed before maxillary segmental osteotomy. The osteotomy positioned the maxillary canines axially to contact the lower dentition bilaterally. G, After surgery, occlusal platforms placed on the maxillary canines support the vertical dimension. H, Three years post treatment. I, Lower anteriors bonded with composite resin as a form of reten- tion. J, Pretreatment. K, Three years post treatment. L, Pretreatment cephalogram. Acceptable vertical dimension. M, One year post treatment. can be reduced with the high-speed handpiece; as the tooth 4. Improvement or correction of mucogingival and osseous is erupted orthodontically (the same amount of bone will defects. Proper repositioning of prominent teeth in the arch remain on the clinical root), the ratio of crown to root will will improve gingival topography (Fig. 21-12). In adoles- be improved (Fig. 21-11).12 cents, the brackets are placed to level marginal ridges and A B C D E F G H I J K L M FIGURE 21-7 Clinical example of adult treatment objective 4: adequate embrasure space and proper root position. -

Eruption of Teeth Assistant Professor Aseel Haidar
Lec. 3 Eruption of teeth Assistant Professor Aseel Haidar Lec.3 Pedodontics Forth stage Assistant Professor Aseel Haidar Early Eruption (NATAL AND NEONATAL TEETH) Natal teeth are (teeth present at birth) and neonatal teeth (teeth that erupt during the first 30 days) prevalence is low. About 85% of natal or neonatal teeth are mandibular primary incisors, and only small percentages are supernumerary teeth. It is common for natal and neonatal teeth to occur in pairs. Natal and neonatal molars are rare. Most studies suggest that the etiology for the premature eruption or the appearance of natal and neonatal teeth is multifactorial. A possible factor involving the early eruption of primary teeth seems to be familial, due to inheritance as an autosomal-dominant trait. A radiograph should be made to determine the amount of root development and the relationship of a prematurely erupted tooth to its adjacent teeth. One of the parents can hold the x-ray film in the infant’s mouth during the exposure. Most prematurely erupted teeth (immature type) are hypermobile because of limited root development. 1. If the tooth is extremely mobile to the extent that there is danger of displacement of the tooth and possible aspiration, so the treatment indicated in such a case is the removal of the tooth. 2. If the tooth has sharp incisal edge that may cause laceration of the lingual surface of the tongue, so treatment is the removal of the tooth. The preferable approach, however, is to leave the tooth in place and to explain to the parents the desirability of maintaining this tooth in the mouth because of its importance in the growth and uncomplicated eruption of the adjacent teeth.