2.01.44 Dermatologic Applications of Photodynamic Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Pharmaceuticals As Environmental Contaminants
PharmaceuticalsPharmaceuticals asas EnvironmentalEnvironmental Contaminants:Contaminants: anan OverviewOverview ofof thethe ScienceScience Christian G. Daughton, Ph.D. Chief, Environmental Chemistry Branch Environmental Sciences Division National Exposure Research Laboratory Office of Research and Development Environmental Protection Agency Las Vegas, Nevada 89119 [email protected] Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Why and how do drugs contaminate the environment? What might it all mean? How do we prevent it? Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada This talk presents only a cursory overview of some of the many science issues surrounding the topic of pharmaceuticals as environmental contaminants Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada A Clarification We sometimes loosely (but incorrectly) refer to drugs, medicines, medications, or pharmaceuticals as being the substances that contaminant the environment. The actual environmental contaminants, however, are the active pharmaceutical ingredients – APIs. These terms are all often used interchangeably Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Office of Research and Development Available: http://www.epa.gov/nerlesd1/chemistry/pharma/image/drawing.pdfNational -

Photodynamic Therapy for the Treatment of Actinic Keratoses and Other Skin Lesions
Photodynamic Therapy for the Treatment of Actinic Keratoses and Other Skin Lesions Policy Number: Current Effective Date: MM.02.016 March 22, 2019 Lines of Business: Original Effective Date: HMO; PPO; QUEST Integration April 01, 2008 Place of Service: Precertification: Office Not Required I. Description Photodynamic therapy (PDT) refers to light activation of a photosensitizer to generate highly reactive intermediaries, which ultimately cause tissue injury and necrosis. Photosensitizing agents are being proposed for use with dermatologic conditions such as actinic keratoses and nonmelanoma skin cancers.For individuals who have nonhyperkeratotic actinic keratoses on the face or scalp who receive PDT, the evidence includes randomized controlled trials (RCTs). The relevant outcomes are symptoms, change in disease status, quality of life, and treatment-related morbidity. Evidence from multiple RCTs has found that PDT improves the net health outcome in patients with nonhyperkeratotic actinic keratoses on the face or scalp compared with placebo or other active interventions. The evidence is sufficient to determine that the technology results in a meaningful improvement in the net health outcome. For individuals who have low-risk basal cell carcinoma who receive PDT, the evidence includes RCTs and systematic reviews of RCTs. The relevant outcomes are symptoms, change in disease status, quality of life, and treatment-related morbidity. Systematic reviews of RCTs have found that PDT may not be as effective as surgery for superficial and nodular basal cell carcinoma. In the small number of trials available, PDT was more effective than placebo. The available evidence from RCTs has suggested that PDT has better cosmetic outcomes than surgery. -
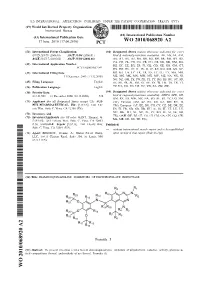
Wo 2010/068920 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 17 June 2010 (17.06.2010) WO 2010/068920 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 239/78 (2006.01) A61P 31/04 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/51 7 (2006.01) A61P 35/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) Number: International Application DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2009/067749 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 11 December 2009 ( 11.12.2009) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (26) Publication Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/121,965 12 December 2008 (12.12.2008) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): AUS- ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, PEX PHARMACEUTICAL, INC. -
Aacr Cancer Progress Report
AACR CANCER PROGRESS REPORT CANCER PROGRESS AACR 615 Chestnut Street, 17th Floor, Philadelphia, PA 19106-4404 2017 AACR CANCER PROGRESS REPORT 2017 Harnessing Research Discoveries to Save Lives AACR.org CancerProgressReport.org #CancerProgress17 For your FREE copy of the full report, go to www.CancerProgressReport.org AACR CANCER PROGRESS REPORT 2017 Harnessing Research Discoveries to Save Lives AACR.org CancerProgressReport.org #CancerProgress17 Please cite this report as: cancerprogressreport.org [Internet]. Philadelphia: American Association for Cancer Research; ©2017 [cited year month date]. Available from http://www.cancerprogressreport.org/. HARNESSING RESEARCH TABLE OF DISCOVERIES TO SAVE LIVES 48 Biomedical Research 48 CONTENTS Progress across the Clinical Cancer Care Continuum 54 Cancer Prevention, Detection, and Diagnosis 54 Simplifying the HPV Vaccination Schedule 54 Enhancing Cancer Detection AACR CANCER PROGRESS and Diagnosis with Technology 54 REPORT 2017 STEERING COMMITTEE iii Treatment with Surgery, Radiotherapy, and Cytotoxic Chemotherapy 56 AACR STAFF iv Improving Outcomes by Combining Existing Treatments 56 Reducing the Adverse Effects of Surgery 56 A MESSAGE FROM THE AACR 1 Tailoring Radiotherapy: Less Is Sometimes More 57 EXECUTIVE SUMMARY 3 Treatment with Molecularly Targeted Therapeutics 57 Cancer in 2017 3 Adding Precision to Treatment for Acute Myeloid Leukemia 61 Targeting Soft Tissue Sarcoma 62 Preventing Cancer: Understanding Risk Factors 4 Increasing Options for Patients with Ovarian Cancer 64 Screening for -

United States Patent 19 11 Patent Number: 5,409,690 Howell Et Al
USOO5409690A United States Patent 19 11 Patent Number: 5,409,690 Howell et al. (45) Date of Patent: Apr. 25, 1995 54 TREATMENT OF MULTIDRUG RESISTANT Primary Examiner-Raymond Henley, III DISEASES IN CANCER CELL BY Assistant Examiner-T. J. Criares POTENTATING WITH MASOPROCOL Attorney, Agent, or Firm-Weiser & Associates 75) Inventors: Stephen Howell, Del Mar, Calif.; Atul Khandwala, Edgewater, N.J.; Om P. 57 ABSTRACT Sachdev, New City, N.Y.; Charles G. Disclosed are: a method for reversing multidrug resis Smith, Rancho Santa Fe, Calif. tance in a mammal; and a composition to reverse multi 73) Assignee: Chemex Pharmaceuticals, Inc., Fort drug resistance comprising: Lee, N.J. 21 Appl. No.: 81,663 is is , is R9 22 Filed: Jun. 23, 1993 R1O g--- 51) Int. Cl. ..................... A61K 48/00; A61K 31/70; R10 R11 R12 R13 R8 A61K 31/045 R2O R7 52 U.S. C. ........................................ 424/10; 514/34; 514/727; 514/731 wherein 58 Field of Search ......................... 514/34, 7. R1 and R2 are independently H, lower alkyl or lower acyl; (56) References Cited R3, R4 and R5 are independently H or lower alkyl; U.S. PATENT DOCUMENTS R7, R8 and R9 are independently H, hydroxy, lower alkoxy or lower acyloxy; and 5,008,294 4/1991 Jordan et al. ....................... 514/73 R10, R11,y R12 and R13yIOXy are independently H or lower OTHER PUBLICATIONS alkyl, in a pharmaceutically acceptable vehicle. Carter et al; Chemotherapy of Cancer, Second Edition, A Wiley Medical Publication, 1981 pp. 361-365. 22 Claims, No Drawings 5,409,690 1. 2 brew tea which was the basis for a folk remedy that TREATMENT OF MULTIDRUG RESISTANT called for drinking the tea to cure colds, rheumatism DISEASES IN CANCER CELL BY POTENTIATING and other ailments. -

(12) Patent Application Publication (10) Pub. No.: US 2002/0010208A1 Shashoua Et Al
US 2002001 0208A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2002/0010208A1 Shashoua et al. (43) Pub. Date: Jan. 24, 2002 (54) DHA-PHARMACEUTICAL AGENT Related U.S. Application Data CONJUGATES OF TAXANES (63) Continuation of application No. 09/135,291, filed on (76) Inventors: Victor Shashoua, Brookline, MA (US); Aug. 17, 1998, now abandoned, which is a continu Charles Swindell, Merion, PA (US); ation of application No. 08/651,312, filed on May 22, Nigel Webb, Bryn Mawr, PA (US); 1996, now Pat. No. 5,795,909. Matthews Bradley, Layton, PA (US) Publication Classification Correspondence Address: Edward R. Gates, Esq. (51) Int. Cl." ............................................ A61K 31/337 Wolf, Greenfield & Sacks, P.C. (52) U.S. Cl. .............................................................. 514/449 600 Atlantic Avenue Boston, MA 02210 (US) (57) ABSTRACT The invention provides conjugates of cis-docosahexaenoic (21) Appl. No.: 09/846,838 acid and pharmaceutical agents useful in treating noncentral nervous System conditions. Methods for Selectively target 22) Filled: Mayy 1, 2001 ingg pharmaceuticalp agents9. to desired tissues are pprovided. Patent Application Publication Jan. 24, 2002 Sheet 1 of 14 US 2002/0010208A1 1 OO 5 O -5OO - 1 OO-9 -8 -7 -6 -5 -4 LOG-10 OF SAMPLE CONCENTRATION (MOLAR) CCRF-CEM-o- SR ----- RPM-8226----- K-562- - -A - - HL-60 (TB) -g- - MOLT4: ... O Fig. 1 1 OO 5 O -5OO -1 O O -8 -7 -6 -5 -4 -- 9 LOGo OF SAMPLE CONCENTRATION (MOLAR) A549/ATCC-o-NS326. NCEKVX 28. --Q-- NCI-H322M-...-a---Eidsf8::... NC-H522--O-- HOP-62---Fig. 2 a-- NC-H460.-------- Patent Application Publication Jan. -

Pharmaceutical Compositions and Dosage Forms of Thalidomide
(19) & (11) EP 2 277 512 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 26.01.2011 Bulletin 2011/04 A61K 9/48 (2006.01) A61K 9/20 (2006.01) A61K 31/454 (2006.01) (21) Application number: 10175930.6 (22) Date of filing: 13.11.2003 (84) Designated Contracting States: (72) Inventor: D’Angio, Paul AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Basking Ridge, NJ 07929 (US) HU IE IT LI LU MC NL PT RO SE SI SK TR Designated Extension States: (74) Representative: Ritter, Thomas Kurt AL LT LV MK Jones Day Prinzregentenstraße 11 (30) Priority: 14.11.2002 US 426016 P 80538 München (DE) (62) Document number(s) of the earlier application(s) in Remarks: accordance with Art. 76 EPC: This application was filed on 09-09-2010 as a 03783567.5 / 1 562 556 divisional application to the application mentioned under INID code 62. (71) Applicant: CELGENE CORPORATION Summit New Jersey 07901 (US) (54) Pharmaceutical compositions and dosage forms of thalidomide (57) Pharmaceutical compositions and single unit not limited to, leprosy, chronic graft-vs-host disease, dosage forms of thalidomide and pharmaceutically ac- rheumatoid arthritis, sarcoidosis, an inflammatory condi- ceptable prodrugs, salts, solvates, hydrates, or clath- tion, inflammatory bowel disease, and cancer using the rates are disclosed. Also disclosed are methods of treat- novel dosage forms disclosed herein. ing and preventing diseases and conditions such as, but EP 2 277 512 A2 Printed by Jouve, 75001 PARIS (FR) EP 2 277 512 A2 Description [0001] This application claims priority to provisional application no. -
Download Supplementary
Supplementary table 1: List of drugs and their binding energies to ACE1 and ACE2. Human ACE1 Human ACE2 Binding energy Binding energy Ligand (kcal/mol) (kcal/mol) (S)-NICARDIPINE -8.6 -6.0 (S)-NITRENDIPINE -7.5 -6.5 17-BETA ESTRADIOL -8.2 -5.7 4-AMINOPYRIDINE -3.9 -4.0 4-PHENYLAMINO-3-QUINOLINECARBONITRILE -8.2 -6.5 ABACAVIR -8.2 -6.3 ABARELIX -6.0 -4.4 ABEMACICLIB -9.1 -6.7 ABIRATERONE ACETATE -9.8 -7.0 ACALABRUTINIB -9.6 -7.2 ACAMPROSATE -5.7 -4.5 ACARBOSE -8.2 -6.0 ACEBUTOLOL -7.3 -5.6 ACETAMINOPHEN -5.5 -5.6 ACETAZOLAMIDE -6.2 -5.1 ACETOHEXAMIDE -8.6 -6.3 ACETOHYDROXAMIC ACID -3.9 -3.5 ACETOPHENAZINE -8.0 -6.2 ACETYLCHOLINE -4.3 -3.5 ACETYLCYSTEINE -4.7 -3.9 ACETYLDIGITOXIN -10.0 -7.1 ACRISORCIN -5.9 -5.8 ACYCLOVIR -6.7 -5.2 ADAPALENE -9.2 -7.3 ADEFOVIR DIPIVOXIL -7.6 -4.8 ADENOSINE -7.0 -5.5 ALATROFLOXACIN -10.6 -6.4 ALBENDAZOLE -6.9 -5.2 ALBUTEROL -6.6 -5.2 ALCAFTADINE -9.0 -5.8 ALCLOMETASONE DIPROPIONATE -8.6 -6.5 ALFENTANIL -7.4 -4.9 ALFUZOSIN -7.7 -5.6 ALISKIREN -7.5 -5.9 ALITRETINOIN -7.4 -5.6 ALLOPURINOL -5.6 -5.1 ALMOTRIPTAN -7.0 -6.0 ALOSETRON -8.3 -6.4 ALPELISIB -8.7 -6.6 ALPHA-TOCOPHEROL -7.4 -5.8 ALPHA-TOCOPHEROL ACETATE -7.8 -5.6 ALPRAZOLAM -8.6 -5.9 ALPROSTADIL -6.2 -5.3 ALTRETAMINE -5.1 -4.1 ALVIMOPAN -8.3 -6.4 AMANTADINE -5.5 -4.6 AMBENONIUM -7.6 -5.5 AMBRISENTAN -7.8 -5.2 AMCINONIDE -10.7 -7.4 AMDINOCILLIN -7.1 -5.8 AMIFAMPRIDINE -4.1 -4.2 AMIFOSTINE -4.8 -3.8 AMIKACIN -7.2 -5.4 AMILORIDE -6.4 -5.9 AMINOCAPROIC ACID -4.9 -4.4 AMINOGLUTETHIMIDE -7.4 -5.7 AMINOLEVULINIC ACID -4.7 -5.3 AMINOMETHYLBENZOIC ACID -6.4 -3.9 -

(12) United States Patent (10) Patent No.: US 9.468,603 B2 Mcchesney Et Al
USOO9468603B2 (12) United States Patent (10) Patent No.: US 9.468,603 B2 McChesney et al. (45) Date of Patent: Oct. 18, 2016 (54) NANOPARTICULATE COMPOSITIONS FOR A61 K3I/7076 (2013.01); A61K 45/06 TARGETED DELIVERY OF ACID LABILE, (2013.01); A61K 47/48061 (2013.01) LIPOPHILIC PRODRUGS OF CANCER (58) Field of Classification Search CHEMOTHERAPEUTICS AND THEIR CPC ........... A61K 47/48061; A61K 45/06; A61 K PREPARATION 9/0019; A61K 9/5123; C07D 305/14: CO7D 314/24: CO7D 407/12: C07D 487/04; C07D (71) Applicant: Arbor Therapeutics, LLC, Etta, MS 491/14: CO7D 493/06; C07D 493/08: C07D (US) 519700 See application file for complete search history. (72) Inventors: James D. McChesney, Etta, MS (US); Igor Nikoulin, San Diego, CA (US); (56) References Cited Steve J. Bannister, Tampa, FL (US); Douglas L. Rodenburg, Thaxton, MS U.S. PATENT DOCUMENTS (US) 4,762,720 A * 8/1988 Jizomoto ............. A61K9/1277 264/4.1 (73) Assignee: ARBOR THERAPEUTICS, LLC, 8.440,714 B2 * 5/2013 McChesney ......... CO7D 305,14 Etta, MS (US) 514,449 2004/0213837 A1* 10/2004 Mantripragada ...... A61K 9,127 424/450 (*) Notice: Subject to any disclaimer, the term of this 2011 0077291 A1* 3, 2011 Chen .................... A61K9/0019 patent is extended or adjusted under 35 514,449 U.S.C. 154(b) by 0 days. 2012/030861.6 A1* 12/2012 Liu ...................... A61K9/0019 424/400 (21) Appl. No.: 14/485,713 2012/0309819 A1 12/2012 McChesney 2015,0297749 A1* 10, 2015 Hahn ................. A61K 49, 1839 (22) Filed: Sep. 13, 2014 424, 1.37 (65) Prior Publication Data FOREIGN PATENT DOCUMENTS US 2015/OO79189 A1 Mar. -

Emerging Strategies for Cancer Immunoprevention
Oncogene (2015) 34, 6029–6039 © 2015 Macmillan Publishers Limited All rights reserved 0950-9232/15 www.nature.com/onc REVIEW Emerging strategies for cancer immunoprevention JC Roeser1, SD Leach2 and F McAllister3 The crucial role of the immune system in the formation and progression of tumors has been widely accepted. On one hand, the surveillance role of the immune system plays an important role in endogenous tumor prevention, but on the other hand, in some special circumstances such as in chronic inflammation, the immune system can actually contribute to the formation and progression of tumors. In recent years, there has been an explosion of novel targeted immunotherapies for advanced cancers. In the present manuscript, we explore known and potential various types of cancer prevention strategies and focus on nonvaccine- based cancer preventive strategies targeting the immune system at the early stages of tumorigenesis. Oncogene (2015) 34, 6029–6039; doi:10.1038/onc.2015.98; published online 14 September 2015 INTRODUCTION Differences between chemoprevention and immunoprevention. As cancer is a collection of multiple complex individual diseases Whereas immunoprevention focuses on directly or indirectly that happen in different sites of the body and progress in different targeting the immune system, chemopreventive strategies utilize ways, a large amount of information is required to understand drugs or natural compounds to prevent cancer development.3 how to prevent each cancer type. Existing interventions for cancer Less than a dozen chemopreventive agents have been FDA prevention focus on the use of chemopreventive agents or approved: tamoxifen and raloxifene for breast cancer fi prevention,4,5 celecoxib for colorectal polyps prevention in vaccines designed and tested for prevention of speci c cancer 6,7 8,9 types. -

Review Article
Review Article Photodynamic therapy in dermatology Chitra S. Nayak Department of Dermatology, BYL Nair Hospital and TN Medial College, Mumbai, India Address for correspondence: Chitra S. Nayak, 302, Arun, 6th Road, Santacruz East, Mumbai - 400055, India. E-mail: [email protected] ABSTRACT Photodynamic therapy is a new modality of therapy being used for the diagnosis and treatment of many tumors. It is now being increasingly used for skin tumors and other dermatological disorders. With its range of application it is certainly the therapy of the future. Its mechanism of action is by the Type II photo-oxidative reaction. The variables are the photosensitizer, the tissue oxygenation and the light source. It has been used to treat various disorders including Bowen’s disease, actinic keratoses, squamous cell carcinomas, basal cell carcinomas, and mycosis fungoides. The side-effects are fortunately mild and transient. Newer photosensitisers like methyl aminolevulinate hold a lot of promise for better therapy. Key Words: Photosensitizer, Light source, Aminolevulinate HISTORY in the target cells followed by selective irradiation of the lesion with visible light. The drug and light are The use of sunlight for the treatment of various skin individually non-toxic, but in combination destroy disorders (heliotherapy) was known to ancient Indians tissues. and Greeks. In the modern era, Oscar Raab, a German medical student first reported the death of Paramecium MECHANISM OF ACTION caudatum (a protozoan) after light exposure in the presence of acridine orange in the year 1900.[1] His The efficacy of PDT depends on all the following professor, von Tappeiner, coined the term mechanisms which are inter-linked: direct cytotoxicity, “photodynamic” to describe oxygen-consuming vascular damage, inflammation and immune host chemical reactions in vivo.