IHS PROVIDER September 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evidenz Und Versorgungsrealität Von Kurzwirksamen Insulinanaloga in Der Behandlung Des Typ-2-Diabetes Mellitus
Evidenz und Versorgungsrealität von kurzwirksamen Insulinanaloga in der Behandlung des Typ-2-Diabetes mellitus – Eine Versorgungsanalyse auf der Basis von Sekundärdaten – Dissertation zur Erlangung des Doktorgrades der Naturwissenschaften vorgelegt beim Fachbereich 14 - Biochemie, Chemie und Pharmazie der Johann Wolfgang Goethe-Universität in Frankfurt am Main von Matthias S. Pfannkuche aus Brühl Frankfurt am Main, im Jahr 2009 vom Fachbereich 14 - Biochemie, Chemie und Pharmazie der Johann Wolfgang Goethe-Universität als Dissertation angenommen. Dekan: Prof. Dr. rer. nat. Dieter Steinhilber Gutachter: Prof. Dr. rer. nat. Theo Dingermann Prof. Dr. rer. nat. Gerd Glaeske (Universität Bremen) Datum der Disputation: 15. Februar 2010 Bildnachweis Titelseite: Insulin Hexamer: http://commons.wikimedia.org/wiki/File:Human-insulin-hexamer-3D-ribbons.png (letzter Zugriff: 11.06.2009) Non semper ea sunt, quae videntur. (Phädrus, fabulae 4, 2, 5) Danksagung Diese Dissertation sowie die hiermit in Verbindung stehenden Publikationen wären ohne die Anregungen und Unterstützung durch viele Kollegen, Freunde und Organisationen nicht möglich gewesen. Ihnen möchte ich an dieser Stelle danken. Mein besonderer Dank gilt Prof. Dr. rer. nat Gerd Glaeske und Prof. Dr. rer. nat. Theo Dingermann, die diese Arbeit in vielerlei Hinsicht erst ermöglichten. Überaus dankbar bin ich Prof. Dr. rer. nat. Gerd Glaeske für die freundliche Aufnahme in seine Arbeitsgruppe, die es mir ermöglichte weitere Einblicke in die Gesundheitsökonomie, Gesundheitspolitik und Versorgungsforschung zu nehmen. Für das Korrekturlesen der kompletten Arbeit, die zahlreichen Hinweise und konstruktiven Diskussionen sowie die zahlreichen Mittagspausen danke ich im besonderen Dr. P.H. Falk Hoffmann. Herzlicher Dank gilt auch dem gesamten Arbeitskreis in Bremen sowie den Projektbeteiligten Krankenkassen, allen voran der GEK, die mir durch den Zugriff auf ihre Daten erst viele Analysen ermöglichten. -
![LANTUS® (Insulin Glargine [Rdna Origin] Injection)](https://docslib.b-cdn.net/cover/0369/lantus%C2%AE-insulin-glargine-rdna-origin-injection-60369.webp)
LANTUS® (Insulin Glargine [Rdna Origin] Injection)
Rev. March 2007 Rx Only LANTUS® (insulin glargine [rDNA origin] injection) LANTUS® must NOT be diluted or mixed with any other insulin or solution. DESCRIPTION LANTUS® (insulin glargine [rDNA origin] injection) is a sterile solution of insulin glargine for use as an injection. Insulin glargine is a recombinant human insulin analog that is a long-acting (up to 24-hour duration of action), parenteral blood-glucose-lowering agent. (See CLINICAL PHARMACOLOGY). LANTUS is produced by recombinant DNA technology utilizing a non- pathogenic laboratory strain of Escherichia coli (K12) as the production organism. Insulin glargine differs from human insulin in that the amino acid asparagine at position A21 is replaced by glycine and two arginines are added to the C-terminus of the B-chain. Chemically, it is 21A- B B Gly-30 a-L-Arg-30 b-L-Arg-human insulin and has the empirical formula C267H404N72O78S6 and a molecular weight of 6063. It has the following structural formula: LANTUS consists of insulin glargine dissolved in a clear aqueous fluid. Each milliliter of LANTUS (insulin glargine injection) contains 100 IU (3.6378 mg) insulin glargine. Inactive ingredients for the 10 mL vial are 30 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, 20 mcg polysorbate 20, and water for injection. Inactive ingredients for the 3 mL cartridge are 30 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, and water for injection. The pH is adjusted by addition of aqueous solutions of hydrochloric acid and sodium hydroxide. LANTUS has a pH of approximately 4. CLINICAL PHARMACOLOGY Mechanism of Action: The primary activity of insulin, including insulin glargine, is regulation of glucose metabolism. -

Diabetes Mellitus: Patterns of Pharmaceutical Use in Manitoba
Diabetes Mellitus: Patterns of Pharmaceutical Use in Manitoba by Kim¡ T. G. Guilbert A Thesis submitted to The Faculty of Graduate Studies in Partial Fulfillment of the Requirements for the Degree of MASTER OF SCIENCE Faculty of Pharmacy The University of Manitoba Winnipeg, Manitoba @ Kimi T.G. Guilbert, March 2005 TIIE UMYERSITY OF MANITOBA F'ACULTY OF GRADUATE STTJDIES +g+ù+ COPYRIGIIT PERMISSION PAGE Diabetes Mellitus: Patterns of Pharmaceutical Use in Manitoba BY Kimi T.G. Guilbert A ThesisÆracticum submitted to the Faculty of Graduate Studies of The University of Manitoba in partial fulfillment of the requirements of the degree of MASTER OF SCIENCE KIMI T.G. GTIILBERT O2()O5 Permission has been granted to the Library of The University of Manitoba to lend or sell copies of this thesis/practicum, to the National Library of Canada to microfïlm this thesis and to lend or sell copies of the film, and to University Microfilm Inc. to publish an abstract of this thesis/practicum. The author reserves other publication rights, and neither this thesis/practicum nor extensive extracts from it may be printed or otherwise reproduced without the author's written permission. Acknowledgements Upon initiation of this project I had a clear objective in mind--to learn more. As with many endeavors in life that are worthwhile, the path I have followed has brought me many places I did not anticipate at the beginning of my journey. ln reaching the end, it is without a doubt that I did learn more, and the knowledge I have been able to take with me includes a wider spectrum than the topic of population health and medication utilization. -

Think Medicines!
Think Issue 13 August 2016 MHRA Drug Safety SGLT2 inhibitors: updated advice on the risk of diabetic Medicines!Updates can be found ketoacidosis (DKA) at the following link. The MHRA are advising health care professionals to test for raised ketones in patients with ketoacidosis symptoms, who are taking SGLT2 inhibitors even if New higher strength Humalog® plasma glucose levels are near-normal. SGLT2 inhibitors include: Canagliflozin, 200 units/ml KwikPen™ Dapagliflozin and Empagliflozin. Serious, life-threatening, and fatal cases of In order to minimize medication DKA have been reported in patients taking an SGLT2 inhibitor. In several cases, errors. blood glucose levels were only moderately elevated (e.g. <14mmol/L) Insulin lispro 200 units/ml representing an atypical presentation for DKA, which could delay diagnosis and solution for injection should treatment. ONLY be administered using the Advice for health Care Professionals: Humalog 200 units/ml pre-filled Inform patients of the signs of diabetic ketoacidosis (DKA) and advise them to pen (KwikPen). seek immediate medical advice if they develop any of these symptoms (e.g. When switching from one rapid weight loss, feeling sick or being sick, stomach pain, fast and deep Humalog strength to another, breathing, sleepiness, a sweet smell to the breath, a sweet or metallic taste in the dose does not need to be the mouth, or a different odour to urine or sweat). converted. Unnecessary dose Discuss the risk factors of DKA with patients. conversion may lead to under/ Discontinue treatment with the SGLT2 inhibitor immediately if DKA is over dosing and resultant hyper/ suspected or diagnosed. -

A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D
Drugs 2005; 65 (3): 325-340 REVIEW ARTICLE 0012-6667/05/0003-0325/$39.95/0 2005 Adis Data Information BV. All rights reserved. A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D. Mooradian Division of Endocrinology, Department of Internal Medicine, Diabetes, and Metabolism, St Louis University School of Medicine, St Louis, Missouri, USA Contents Abstract ....................................................................................325 1. Physiology of Insulin Secretion .............................................................326 2. Conventional Insulin Preparations ..........................................................327 3. Insulin Analogues ........................................................................328 3.1 Rapid-Acting Insulin Analogues .......................................................328 3.1.1 Insulin Lispro ...................................................................328 3.1.2 Insulin Aspart ..................................................................329 3.1.3 Insulin Glulisine .................................................................329 3.1.4 Clinical Utility of Rapid-Acting Insulin Analogues ...................................330 3.2 Premixed Insulins and Insulin Analogues ................................................331 3.3 Basal Insulin Analogues ...............................................................331 3.3.1 Insulin Glargine ................................................................331 -

Step Therapy
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2020 P 3086-9 Program Step Therapy – Diabetes Medications - SGLT2 Inhibitors Medication Farxiga (dapagliflozin)*, Glyxambi (empagliflozin/linagliptan), Invokana (canagliflozin)*, Invokamet (canagliflozin/metformin)*, Invokamet XR (canaglifloxin/metformin extended-release)*, Jardiance (empagliflozin), Qtern (dapagliflozin/saxagliptin)*, Segluromet (ertugliflozin/metformin)*, Steglatro (ertugliflozin)*, Steglujan (ertugliflozin/sitagliptin)*, Xigduo XR (dapagliflozin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 4/2018, 8/2018, 12/2018, 2/2019, 2/2020, 5/2020; 7/2020 Effective Date 10/1/2020; Oxford only: 10/1/2020 1. Background: Farxiga (dapagliflozin)*, Invokana (canagliflozin)*, Jardiance (empagliflozin) and Steglatro (ertugliflozin)* are sodium-glucose co-transporter 2 (SGLT2) inhibitors indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Farxiga*, Invokana* and Jardiance have additional indications. Farxiga* is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction. Invokana* is indicated to reduce the risk of major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction and nonfatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease (CVD), and to reduce the risk of end-stage kidney disease (ESKD), doubling of -

Ertugliflozin 5Mg, 15Mg Film-Coated Tablet (Steglatro®) Merck Sharp & Dohme
1 www.scottishmedicines.org.uk SMC2102 ertugliflozin 5mg, 15mg film-coated tablet (Steglatro®) Merck Sharp & Dohme 7 December 2018 The Scottish Medicines Consortium (SMC) has completed its assessment of the above product and advises NHS Boards and Area Drug and Therapeutic Committees (ADTCs) on its use in NHSScotland. The advice is summarised as follows: ADVICE: following a full submission ertugliflozin (Steglatro®) is accepted for restricted use within NHSScotland. Indication under review: in adults aged 18 years and older with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: As monotherapy in patients for whom the use of metformin is considered inappropriate due to intolerance or contraindications. In addition to other medicinal products for the treatment of diabetes. SMC restriction: ertugliflozin is accepted for use as monotherapy and as add-on therapy. When used as monotherapy it is restricted to patients who would otherwise receive a dipeptidyl peptidase-4 inhibitor and in whom a sulphonylurea or pioglitazone is not appropriate. Ertugliflozin was superior to placebo in lowering HbA1c in adults with type 2 diabetes mellitus in phase III studies in monotherapy, dual therapy and triple therapy settings. Chairman Scottish Medicines Consortium Published 14 January 2019 1 Indication In adults aged 18 years and older with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: As monotherapy in patients for whom the use of metformin is considered inappropriate due to intolerance or contraindications. In addition to other medicinal products for the treatment of diabetes.1 Dosing Information The recommended starting dose is 5mg orally once daily which can, if tolerated, be increased to 15mg once daily if additional glycaemic control is needed. -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -
Effects of Basal Insulin Analog and Metformin on Glycaemia Control and Weight As Risk &Factors for Endothelial Dysfunction
EFFECTS OF BASAL INSULIN ANALOG AND METFORMIN ON GLYCAEMIA CONTROL AND WEIGHT AS RISK &FACTORS FOR ENDOTHELIAL DYSFUNCTION Belma Aščić – Buturović¹*, Mirsad Kacila² ¹ Clinic of Endocrinology, Diabetes Mellitus and Metabolic Diseases, University of Sarajevo Clinics Centre, Bolnička , Sarajevo, Bosnia and Herzegovina ² Center for Heart Diseases, University of Sarajevo Clinics Centre, Bolnička , Sarajevo, Bosnia and Herzegovina * Corresponding author Abstract Obese patients with type diabetes and impaired glucose tolerance are at increased risk of develop- ment of cardiovascular diseases. Endothelial dysfunction may be a reason for development of ath- erosclerosis and cardiovascular diseases. Lifestyle modifi cation, increased physical activity, weight reduction, energy restricted diet and good glycaemia control can be useful for the endothelial func- tion improvement and may decrease the risk of cardiovascular diseases. Th e aim of this study was to evaluate the eff ects of basal insulin analog and metformin on glycaemia control and weight as risk factors of endothelial dysfunction. Total of patients ( male and female) with type dia- betes were studied. Th e patients were monitored over six months period. Glycated hemoglobin (HbAc), fasting plasma glucose (FPG), postprandial plasma glucose (PPG), and body mass index (BMI) were observed. Mean age of the subjects was , ± , years. Mean diabetes duration was , ± , years. At the end of the study mean body mass index decreased from , ± , kg/m to , ±, kg/m. In this study we included diabetic patients with fasting glycaemia over mmol/ dm, postmeal glycaemia over , mmol/dm and glycated hemoglobin over . Prior to the study, the patients were treated with premix insulin divided in two daily doses and metformin after the lunch, which did not result in suffi cient regulation of glycaemia. -

SGLT2) Inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM
Sodium-glucose cotransporter-2 (SGLT2) inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM) There are currently four SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin and ertugliflozin) licensed in the UK for the management of adults with T2DM. No head to head trials between the SGLT2 inhibitors have been conducted. As at December 2019, clinical outcome data is available for three of the four SGLT2 inhibitors around their cardiovascular effects in people with T2DM. Ertugliflozin is still to report on this data. This document summarises the key prescribing considerations. NICE Technology Appraisal Recommendation NICE makes recommendations for when SGLT2 inhibitors can be considered in adults with T2DM; Hertfordshire Medicines Management Committee Recommendations are in line with NICE guidance: Monotherapy NICE TA 390: Canagliflozin, Dapagliflozin and Empagliflozin and NICE TA 572: Ertugliflozin as monotherapies for treating T2DM Monotherapy recommended as option in adults for whom metformin is contraindicated or not tolerated and when diet & exercise alone do not provide adequate glycaemic control, only if: •a DPP‑4 inhibitor would otherwise be prescribed and •a sulfonylurea or pioglitazone is not appropriate. Dual therapy NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin, TA 572: Ertugliflozin as combination therapies for treating T2DM In a dual therapy regimen in combination with metformin is recommended as an option, only if: •a sulfonylurea is contraindicated or not tolerated or •the person is at significant risk of hypoglycaemia or its consequences. In combination with insulin NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option. -

SGLT2 Inhibitors in Combination Therapy: from Mechanisms To
Diabetes Care Volume 41, August 2018 1543 Michael¨ J.B. van Baar, SGLT2 Inhibitors in Combination Charlotte C. van Ruiten, Marcel H.A. Muskiet, Therapy: From Mechanisms to Liselotte van Bloemendaal, Richard G. IJzerman, and PERSPECTIVES IN CARE Clinical Considerations in Type 2 Daniel¨ H. van Raalte Diabetes Management Diabetes Care 2018;41:1543–1556 | https://doi.org/10.2337/dc18-0588 The progressive nature of type 2 diabetes (T2D) requires practitioners to periodically evaluate patients and intensify glucose-lowering treatment once glycemic targets are not attained. With guidelines moving away from a one-size-fits-all approach toward setting patient-centered goals and allowing flexibility in choosing a second-/ third-line drug from the growing number of U.S. Food and Drug Administration– approved glucose-lowering agents, keen personalized management in T2D has become a challenge for health care providers in daily practice. Among the newer generation of glucose-lowering drug classes, sodium–glucose cotransporter 2 inhibitors (SGLT2is), which enhance urinary glucose excretion to lower hyper- glycemia, have made an imposing entrance to the T2D treatment armamentarium. Given their unique insulin-independent mode of action and their favorable efficacy– to–adverse event profile and given their marked benefits on cardiovascular-renal outcome in moderate-to-high risk T2D patients, which led to updates of guidelines and product monographs, the role of this drug class in multidrug regimes is promising. However, despite many speculations based on pharmacokinetic and pharmacodynamic properties, physiological reasoning, and potential synergism, the effects of these agents in terms of glycemic and pleiotropic efficacy when combined with other glucose-lowering drug classes are largely understudied. -
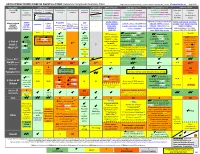
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis.