SGLT2 Inhibitors in Combination Therapy: from Mechanisms To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Think Medicines!
Think Issue 13 August 2016 MHRA Drug Safety SGLT2 inhibitors: updated advice on the risk of diabetic Medicines!Updates can be found ketoacidosis (DKA) at the following link. The MHRA are advising health care professionals to test for raised ketones in patients with ketoacidosis symptoms, who are taking SGLT2 inhibitors even if New higher strength Humalog® plasma glucose levels are near-normal. SGLT2 inhibitors include: Canagliflozin, 200 units/ml KwikPen™ Dapagliflozin and Empagliflozin. Serious, life-threatening, and fatal cases of In order to minimize medication DKA have been reported in patients taking an SGLT2 inhibitor. In several cases, errors. blood glucose levels were only moderately elevated (e.g. <14mmol/L) Insulin lispro 200 units/ml representing an atypical presentation for DKA, which could delay diagnosis and solution for injection should treatment. ONLY be administered using the Advice for health Care Professionals: Humalog 200 units/ml pre-filled Inform patients of the signs of diabetic ketoacidosis (DKA) and advise them to pen (KwikPen). seek immediate medical advice if they develop any of these symptoms (e.g. When switching from one rapid weight loss, feeling sick or being sick, stomach pain, fast and deep Humalog strength to another, breathing, sleepiness, a sweet smell to the breath, a sweet or metallic taste in the dose does not need to be the mouth, or a different odour to urine or sweat). converted. Unnecessary dose Discuss the risk factors of DKA with patients. conversion may lead to under/ Discontinue treatment with the SGLT2 inhibitor immediately if DKA is over dosing and resultant hyper/ suspected or diagnosed. -

IHS PROVIDER September 2017
September 2017 Volume 42 Number 9 Indian Health Service National Pharmacy and Therapeutics Committee SGLT-2 inhibitors (Update) NPTC Formulary Brief August Meeting 2017 Background: The FDA has currently approved three SGLT-2 inhibitors, two of which have completed FDA-mandated cardiovascular outcomes trials. Last year, in the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG), empagliflozin not only reduced cardiovascular events, but also mortality.1 This year, the Canagliflozin Cardiovascular Assessment Study (CANVAS) demonstrated equivocal cardiovascular benefits, no mortality benefit, and significant harms in those receiving canagliflozin.2 The DECLARE-TIMI 58 cardiovascular study of dapagliflozin will be completed in April 2019 (ClinicalTrials.gov Identifier: NCT01730534). Uncertainty remains regarding the current data, long- term benefits and harms, and differentiation among SGLT-2 inhibitors. Following a review of SGLT2 inhibitors at the August 2017 NPTC meeting on their cardiovascular outcomes, net benefit and place in therapy, no modifications were made to the National Core Formulary (NCF). Discussion: EMPA-REG enrolled 7,020 patients with Type 2 diabetes mellitus (T2DM) and HgbA1c values between 7.0-10.0%. All patients had established cardiovascular disease (CVD) and were observed for a median duration of 3.1 years. Empagliflozin reduced the primary outcome of cardiovascular (CV) death, nonfatal myocardial infarction (MI), or nonfatal cardiovascular accident (CVA) by 6.5 events per 1000 patient-years (pt-yrs). Mortality decreased by 9.2 events per 1000 pt-yrs, primarily driven by a reduction in CV mortality of 7.8 events per 1000 pt-yrs. Heart failure hospitalization decreased by 5.1 events per 1000 pt-yrs. -

Step Therapy
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2020 P 3086-9 Program Step Therapy – Diabetes Medications - SGLT2 Inhibitors Medication Farxiga (dapagliflozin)*, Glyxambi (empagliflozin/linagliptan), Invokana (canagliflozin)*, Invokamet (canagliflozin/metformin)*, Invokamet XR (canaglifloxin/metformin extended-release)*, Jardiance (empagliflozin), Qtern (dapagliflozin/saxagliptin)*, Segluromet (ertugliflozin/metformin)*, Steglatro (ertugliflozin)*, Steglujan (ertugliflozin/sitagliptin)*, Xigduo XR (dapagliflozin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 4/2018, 8/2018, 12/2018, 2/2019, 2/2020, 5/2020; 7/2020 Effective Date 10/1/2020; Oxford only: 10/1/2020 1. Background: Farxiga (dapagliflozin)*, Invokana (canagliflozin)*, Jardiance (empagliflozin) and Steglatro (ertugliflozin)* are sodium-glucose co-transporter 2 (SGLT2) inhibitors indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Farxiga*, Invokana* and Jardiance have additional indications. Farxiga* is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction. Invokana* is indicated to reduce the risk of major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction and nonfatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease (CVD), and to reduce the risk of end-stage kidney disease (ESKD), doubling of -

SGLT2 Inhibitors and Kidney Outcomes in Patients with Chronic Kidney Disease
Journal of Clinical Medicine Editorial SGLT2 Inhibitors and Kidney Outcomes in Patients with Chronic Kidney Disease Swetha R. Kanduri 1 , Karthik Kovvuru 1, Panupong Hansrivijit 2 , Charat Thongprayoon 3, Saraschandra Vallabhajosyula 4, Aleksandra I. Pivovarova 5 , Api Chewcharat 3, Vishnu Garla 6, Juan Medaura 5 and Wisit Cheungpasitporn 3,5,* 1 Department of Nephrology, Ochsner Medical Center, New Orleans, LA 70121, USA; [email protected] (S.R.K.); [email protected] (K.K.) 2 Department of Internal Medicine, University of Pittsburgh Medical Center Pinnacle, Harrisburg, PA 17105, USA; [email protected] 3 Division of Nephrology and Hypertension, Mayo Clinic, Rochester, MN 55905, USA; [email protected] (C.T.); [email protected] (A.C.) 4 Section of Interventional Cardiology, Division of Cardiovascular Medicine, Department of Medicine, Emory University School of Medicine, Atlanta, GA 30322, USA; [email protected] 5 Division of Nephrology, Department of Medicine, University of Mississippi Medical Center, Jackson, MS 39156, USA; [email protected] (A.I.P.); [email protected] (J.M.) 6 Department of Internal Medicine and Mississippi Center for Clinical and Translational Research, University of Mississippi Medical Center, Jackson, MS 39156, USA; [email protected] * Correspondence: [email protected] Received: 20 August 2020; Accepted: 20 August 2020; Published: 24 August 2020 Abstract: Globally, diabetes mellitus is a leading cause of kidney disease, with a critical percent of patients approaching end-stage kidney disease. In the current era, sodium-glucose co-transporter 2 inhibitors (SGLT2i) have emerged as phenomenal agents in halting the progression of kidney disease. Positive effects of SGLT2i are centered on multiple mechanisms, including glycosuric effects, tubule—glomerular feedback, antioxidant, anti-fibrotic, natriuretic, and reduction in cortical hypoxia, alteration in energy metabolism. -

Ertugliflozin 5Mg, 15Mg Film-Coated Tablet (Steglatro®) Merck Sharp & Dohme
1 www.scottishmedicines.org.uk SMC2102 ertugliflozin 5mg, 15mg film-coated tablet (Steglatro®) Merck Sharp & Dohme 7 December 2018 The Scottish Medicines Consortium (SMC) has completed its assessment of the above product and advises NHS Boards and Area Drug and Therapeutic Committees (ADTCs) on its use in NHSScotland. The advice is summarised as follows: ADVICE: following a full submission ertugliflozin (Steglatro®) is accepted for restricted use within NHSScotland. Indication under review: in adults aged 18 years and older with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: As monotherapy in patients for whom the use of metformin is considered inappropriate due to intolerance or contraindications. In addition to other medicinal products for the treatment of diabetes. SMC restriction: ertugliflozin is accepted for use as monotherapy and as add-on therapy. When used as monotherapy it is restricted to patients who would otherwise receive a dipeptidyl peptidase-4 inhibitor and in whom a sulphonylurea or pioglitazone is not appropriate. Ertugliflozin was superior to placebo in lowering HbA1c in adults with type 2 diabetes mellitus in phase III studies in monotherapy, dual therapy and triple therapy settings. Chairman Scottish Medicines Consortium Published 14 January 2019 1 Indication In adults aged 18 years and older with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: As monotherapy in patients for whom the use of metformin is considered inappropriate due to intolerance or contraindications. In addition to other medicinal products for the treatment of diabetes.1 Dosing Information The recommended starting dose is 5mg orally once daily which can, if tolerated, be increased to 15mg once daily if additional glycaemic control is needed. -

PRODUCT INFORMATION Ipragliflozin Item No
PRODUCT INFORMATION Ipragliflozin Item No. 22287 CAS Registry No.: 761423-87-4 OH Formal Name: (1S)-1,5-anhydro-1-C-[3-(benzo[b]thien- 2-ylmethyl)-4-fluorophenyl]-D-glucitol OH Synonym: ASP1941 O MF: C21H21FO5S FW: 404.5 S OH Purity: ≥98% OH UV/Vis.: λmax: 231, 267 nm Supplied as: A crystalline solid F Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Ipragliflozin is supplied as a crystalline solid. A stock solution may be made by dissolving the ipragliflozin in the solvent of choice. Ipragliflozin is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide, which should be purged with an inert gas. The solubility of ipragliflozin in these solvents is approximately 30 mg/ml. Ipragliflozin is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, ipragliflozin should first be dissolved in ethanol and then diluted with the aqueous buffer of choice. Ipragliflozin has a solubility of approximately 0.13 mg/ml in a 1:7 solution of ethanol:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. Description Ipragliflozin is a sodium-glucose cotransporter 2 (SGLT2) inhibitor (IC50 = 7.4 nM in CHO cells expressing the human cotransporter).1 It is selective for SGLT2 over SGLT1, SGLT3, SGLT4, SGLT5, and SGLT6 (IC50s = 1.9, 30.4, 15.9, 0.46, and 10.4 µM, respectively). Ipragliflozin (0.1-3 mg/kg) decreases plasma levels of insulin and glucose in an oral glucose tolerance test in a mouse model of diabetes induced by high-fat diet, streptozotocin (STZ; Item No. -

SGLT2) Inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM
Sodium-glucose cotransporter-2 (SGLT2) inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM) There are currently four SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin and ertugliflozin) licensed in the UK for the management of adults with T2DM. No head to head trials between the SGLT2 inhibitors have been conducted. As at December 2019, clinical outcome data is available for three of the four SGLT2 inhibitors around their cardiovascular effects in people with T2DM. Ertugliflozin is still to report on this data. This document summarises the key prescribing considerations. NICE Technology Appraisal Recommendation NICE makes recommendations for when SGLT2 inhibitors can be considered in adults with T2DM; Hertfordshire Medicines Management Committee Recommendations are in line with NICE guidance: Monotherapy NICE TA 390: Canagliflozin, Dapagliflozin and Empagliflozin and NICE TA 572: Ertugliflozin as monotherapies for treating T2DM Monotherapy recommended as option in adults for whom metformin is contraindicated or not tolerated and when diet & exercise alone do not provide adequate glycaemic control, only if: •a DPP‑4 inhibitor would otherwise be prescribed and •a sulfonylurea or pioglitazone is not appropriate. Dual therapy NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin, TA 572: Ertugliflozin as combination therapies for treating T2DM In a dual therapy regimen in combination with metformin is recommended as an option, only if: •a sulfonylurea is contraindicated or not tolerated or •the person is at significant risk of hypoglycaemia or its consequences. In combination with insulin NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option. -
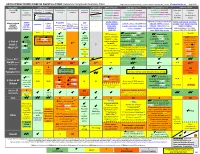
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis. -

Cost-Effectiveness of Empagliflozin Versus Canagliflozin, Dapagliflozin
Emerging technologies, pharmacology and therapeutics Open access Original research BMJ Open Diab Res Care: first published as 10.1136/bmjdrc-2020-001313 on 3 May 2021. Downloaded from Cost-effectivenessofempagliflozin versuscanagliflozin,dapagliflozin,or standardofcareinpatientswithtype2 diabetesandestablished cardiovasculardisease Odette S Reifsnider ,1 Anuraag R Kansal,1 Pranav K Gandhi,2 Lael Cragin,1 Sarah B Brand,1 Egon Pfarr,3 Kyle Fahrbach,4 Anastasia Ustyugova3 To cite: Reifsnider OS, ABSTRACT Kansal AR, Gandhi PK, Introduction Empagliflozin, a sodium- glucose co- Significance of this study et al. Cost- effectiveness transporter-2 (SGLT-2) inhibitor, is approved in the USA of empagliflozin versus to reduce risk of cardiovascular (CV) death in adults What is already known about this subject? canagliflozin, dapagliflozin, with type 2 diabetes mellitus (T2DM) and established CV ► The sodium glucose co- transporter-2 inhibitor (SGLT- or standard of care in 2) empagliflozin is Food and Drug Administration patients with type 2 disease, based on EMPA-REG OUTCOME (Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes (FDA) approved to reduce the risk of cardiovascular diabetes and established (CV) death in adults with type 2 diabetes mellitus cardiovascular disease. Mellitus Patients) trial results. Empagliflozin reduced major (T2DM) and established CV disease (CVD) based BMJ Open Diab Res Care adverse CV event (MACE) by 14%, CV death by 38%, and 2021;9:e001313. doi:10.1136/ hospitalization for heart failure (HHF) by 35% vs placebo, on the EMPA- REG OUTCOME trial, which showed a bmjdrc-2020-001313 each on top of standard of care (SoC). -

Effect of Ipragliflozin, an SGLT2 Inhibitor, on Cardiac Histopathological T Changes in a Non-Diabetic Rat Model of Cardiomyopathy ⁎ Toshiyuki Takasu , Shoji Takakura
Life Sciences 230 (2019) 19–27 Contents lists available at ScienceDirect Life Sciences journal homepage: www.elsevier.com/locate/lifescie Effect of ipragliflozin, an SGLT2 inhibitor, on cardiac histopathological T changes in a non-diabetic rat model of cardiomyopathy ⁎ Toshiyuki Takasu , Shoji Takakura Drug Discovery Research, Astellas Pharma Inc., Tsukuba-shi, Ibaraki, Japan ARTICLE INFO ABSTRACT Keywords: Aims: We investigated the effect of the selective sodium-dependent glucose cotransporter 2 (SGLT2) inhibitor Sodium-dependent glucose cotransporter 2 ipragliflozin on cardiac dysfunction and histopathology in a non-diabetic rat model of cardiomyopathy. Ipragliflozin L-proline (PubChem CID: Main methods: Ipragliflozin was mixed with chow (0.01%, w/w) and administered to male DahlS.Z-Leprfa/Leprfa 57339444) (DS/obese) rats for 8 weeks. Male DahlS.Z-Lepr+/Lepr+ (DS/lean) rats of the same age were used as controls. Cardio-protective effect Systolic blood pressure (SBP) and heart rate (HR) were measured every 4 weeks. After 8 weeks of treatment, echocardiography and histopathological examinations were performed. Further, the effect of ipragliflozin on blood and urine parameters were investigated. Key findings: In the DS/obese rats, ipragliflozin delayed the age-related increase in SBP without affecting HR, reduced left ventricular (LV) mass and intraventricular septal thickness in echocardiography, and ameliorated hypertrophy of cardiomyocytes and LV fibrosis in histopathological examination. Although ipragliflozin sig- nificantly increased both urine volume and urinary glucose excretion in DS/obese rats, it did not alterplasma glucose levels. Significance: Ipragliflozin prevented LV hypertrophy and fibrosis in non-diabetic DS/obese rats without affecting plasma glucose levels. These findings suggest that SGLT2 inhibitors have a cardio-protective effect in non-dia- betic patients with cardiomyopathy. -

Identification of SGLT2 Inhibitor Ertugliflozin As a Treatment
bioRxiv preprint doi: https://doi.org/10.1101/2021.06.18.448921; this version posted June 18, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Identification of SGLT2 inhibitor Ertugliflozin as a treatment for COVID-19 using computational and experimental paradigm Shalini SaxenaA, Kranti MeherC, Madhuri RotellaC, Subhramanyam VangalaC, Satish ChandranC, Nikhil MalhotraB, Ratnakar Palakodeti B, Sreedhara R Voleti A*, and Uday SaxenaC* A In Silico Discovery Research Academic Services (INDRAS) Pvt. Ltd. 44-347/6, Tirumalanagar, Moula Ali, Hyderabad – 500040, TS, India B Tech Mahindra Gateway Building, Apollo Bunder, Mumbai-400001, Maharashtra, India C Reagene Innovation Pvt. Ltd. 18B, ASPIRE-BioNEST, 3rd Floor, School of Life Sciences, University of Hyderabad, Gachibowli, Hyderabad – 500046, TS, India *Corresponding Authors email address: [email protected] [email protected] Abstract Drug repurposing can expedite the process of drug development by identifying known drugs which are effective against SARS-CoV-2. The RBD domain of SARS-CoV-2 Spike protein is a promising drug target due to its pivotal role in viral-host attachment. These specific structural domains can be targeted with small molecules or drug to disrupt the viral attachment to the host proteins. In this study, FDA approved Drugbank database were screened using a virtual screening approach and computational chemistry methods. Five drugs were short listed for further profiling based on docking score and binding energies. Further these selected drugs were tested for their in vitro biological activity. -

Sodium–Glucose Cotransporter 2 Inhibitors and the Risk of Fractures
Diabetes Care e1 Sodium–Glucose Cotransporter Devin Abrahami,1,2 Antonios Douros,1,3,4 Hui Yin,1 2 Inhibitors and the Risk of Fractures Oriana H.Y. Yu,1,5 and Among Patients With Type 2 Diabetes Laurent Azoulay1,2,6 https://doi.org/10.2337/dc19-0849 The association between sodium–glucose (alternate metformin indication) at the initiation before 2013; i.e., prevalent cotransporter 2 (SGLT2) inhibitors and the time of the first-ever prescription of an use); and 4) other treatments. Current risk of fractures is controversial. In the antidiabetic drug. Using this base and new use DPP-4 inhibitors served as Canagliflozin Cardiovascular Assessment cohort, we then assembled a study the reference group. For all exposure Study (CANVAS) Program, canagliflozin cohort of individuals who initiated a new categories, exposed person-time was de- was associated with a significant in- antidiabetic drug class as of 2013 (year fined by the prescription duration plus a creased risk of fractures compared with the first SGLT2 inhibitor was intro- 90-day grace period to allow for a poten- placebo (hazard ratio [HR] 1.26, 95% CI duced in the U.K.). Cohort entry was tial latent exposure effect on the out- 1.04–1.52) (1). Possible mechanisms may defined by the date of this new pre- come. Time-dependent Cox proportional involve elevated serum phosphate levels scription. We excluded individuals hazards models were used to calculate or reductions in bone mineral density (2). with a diagnosis of Paget disease, HRs, adjusted for 45 covariates (Table 1), To date, three recent observational stud- osteomalacia, or hyperparathyroid- including smoking status, BMI, medica- ies investigated this association, but ism, rare risk factors associated with tions, and duration of treated diabetes.