Handbook of Peripheral Neuropathy DK1596 Half-Series-Title 7/6/05 1:55 PM Page B
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Richard Russell, the Senate Armed Services Committee & Oversight of America’S Defense, 1955-1968
BALANCING CONSENSUS, CONSENT, AND COMPETENCE: RICHARD RUSSELL, THE SENATE ARMED SERVICES COMMITTEE & OVERSIGHT OF AMERICA’S DEFENSE, 1955-1968 DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Joshua E. Klimas, M.A. * * * * * The Ohio State University 2007 Dissertation Committee: Approved by Professor David Stebenne, Advisor Professor John Guilmartin Advisor Professor James Bartholomew History Graduate Program ABSTRACT This study examines Congress’s role in defense policy-making between 1955 and 1968, with particular focus on the Senate Armed Services Committee (SASC), its most prominent and influential members, and the evolving defense authorization process. The consensus view holds that, between World War II and the drawdown of the Vietnam War, the defense oversight committees showed acute deference to Defense Department legislative and budget requests. At the same time, they enforced closed oversight procedures that effectively blocked less “pro-defense” members from influencing the policy-making process. Although true at an aggregate level, this understanding is incomplete. It ignores the significant evolution to Armed Services Committee oversight practices that began in the latter half of 1950s, and it fails to adequately explore the motivations of the few members who decisively shaped the process. SASC chairman Richard Russell (D-GA) dominated Senate deliberations on defense policy. Relying only on input from a few key colleagues – particularly his protégé and eventual successor, John Stennis (D-MS) – Russell for the better part of two decades decided almost in isolation how the Senate would act to oversee the nation’s defense. -

(Kir) Channels in Tick Salivary Gland Function Zhilin Li Louisiana State University and Agricultural and Mechanical College, [email protected]
Louisiana State University LSU Digital Commons LSU Master's Theses Graduate School 3-26-2018 Characterizing the Physiological Role of Inward Rectifier Potassium (Kir) Channels in Tick Salivary Gland Function Zhilin Li Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_theses Part of the Entomology Commons Recommended Citation Li, Zhilin, "Characterizing the Physiological Role of Inward Rectifier Potassium (Kir) Channels in Tick Salivary Gland Function" (2018). LSU Master's Theses. 4638. https://digitalcommons.lsu.edu/gradschool_theses/4638 This Thesis is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Master's Theses by an authorized graduate school editor of LSU Digital Commons. For more information, please contact [email protected]. CHARACTERIZING THE PHYSIOLOGICAL ROLE OF INWARD RECTIFIER POTASSIUM (KIR) CHANNELS IN TICK SALIVARY GLAND FUNCTION A Thesis Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Master of Science in The Department of Entomology by Zhilin Li B.S., Northwest A&F University, 2014 May 2018 Acknowledgements I would like to thank my family (Mom, Dad, Jialu and Runmo) for their support to my decision, so I can come to LSU and study for my degree. I would also thank Dr. Daniel Swale for offering me this awesome opportunity to step into toxicology filed, ask scientific questions and do fantastic research. I sincerely appreciate all the support and friendship from Dr. -

Congressional Mail Logs for the President (1)” of the John Marsh Files at the Gerald R
The original documents are located in Box 8, folder “Congress - Congressional Mail Logs for the President (1)” of the John Marsh Files at the Gerald R. Ford Presidential Library. Copyright Notice The copyright law of the United States (Title 17, United States Code) governs the making of photocopies or other reproductions of copyrighted material. Gerald R. Ford donated to the United States of America his copyrights in all of his unpublished writings in National Archives collections. Works prepared by U.S. Government employees as part of their official duties are in the public domain. The copyrights to materials written by other individuals or organizations are presumed to remain with them. If you think any of the information displayed in the PDF is subject to a valid copyright claim, please contact the Gerald R. Ford Presidential Library. r Digitized from Box 8 of The John Marsh Files at the Gerald R. Ford Presidential Library Presi dent's Mail - May 11, 1976 House 1. Augustus Hawkins Writes irr regard to his continuing · terest in meeting with the President to discuss the· tuation at the Equal Employment Opportunity Commission prior to the appoint ment of a successor to Chairman owell W. Perry. 2. Larry Pressler Says he will vote to sustain e veto of the foreign military assistance se he believes the $3.2 billion should be u ed for nior citizens here at horne. 3. Gus Yatron Writes on behalf of Mrs. adys S. Margolis concerning the plight of Mr. Mi ail ozanevich and his family in the Soviet Union. 4. Guy Vander Jagt Endorses request of the TARs to meet with the President during their convention in June. -
Toxicological Testing in Large Animals
Toxicological Testing in Large Animals Toxic causes of ill health and death in production animals are numerous. Toxin testing requires a specific toxin to be nominated as there is no suite of tests that covers all possibilities. Toxin testing is inherently expensive, requires specific sample types and false negatives can occur; for instance the toxin may have been eliminated from the body or be undetectable, but clinical signs may persist. Gribbles Veterinary Pathology can offer specific testing for a range of toxic substances, however it is important to consider the specific sample requirements and testing limitations for each toxin when advising your clients. Many tests are referred to external laboratories and may have extended turnaround times. Please contact the laboratory if you need testing for a specific toxin not listed here; we can often source unusual tests as needed from our network of referral laboratories. Clinicians should also consider syndromes which may mimic intoxication such as hypocalcaemia, hypoglycaemia, hepatic encephalopathy, peripheral neuropathies and primary CNS diseases. Examples of intoxicants that can be tested are provided below. See individual tests in the Pricelist for sample requirements and costs. Biological control agents Heavy metals • 1080 (fluoroacetate) • Arsenic • Strychnine • Lead • Synthetic pyrethroids • Copper • Organophosphates • Selenium • Organochlorines • Zinc • Carbamates • Metaldehyde • Anticoagulant rodenticides (warfarin, pindone, coumetetryl, bromadiolone, difenacoum, brodifacoum) -
Neuromuscular Disorders Neurology in Practice: Series Editors: Robert A
Neuromuscular Disorders neurology in practice: series editors: robert a. gross, department of neurology, university of rochester medical center, rochester, ny, usa jonathan w. mink, department of neurology, university of rochester medical center,rochester, ny, usa Neuromuscular Disorders edited by Rabi N. Tawil, MD Professor of Neurology University of Rochester Medical Center Rochester, NY, USA Shannon Venance, MD, PhD, FRCPCP Associate Professor of Neurology The University of Western Ontario London, Ontario, Canada A John Wiley & Sons, Ltd., Publication This edition fi rst published 2011, ® 2011 by Blackwell Publishing Ltd Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -

Information About Tick Paralysis? Adapted From: CDC
Peachtree Street NW, 15th Floor Atlanta, Georgia 30303-3142 Georgia Department of Public Health www.health.state.ga.us Tick Paralysis Q&A What is tick paralysis? Tick paralysis refers to acute onset of paralysis caused by a tick bite. The condition is primarily found in the Rocky Mountain and northwestern regions of the United States and is rare in Georgia. The number of cases per year is unknown because physicians are not required to report cases of tick paralysis to Public Health. How is tick paralysis spread? Tick paralysis results from a neurotoxin that is secreted in the saliva of certain ticks when they feed. The tick must be attached for several days. Person‐to‐person transmission of tick paralysis has not been documented. Who gets tick paralysis? Anyone who is bitten by a tick can get tick paralysis, but it most commonly affects children less than 10 years of age. What are the symptoms of tick paralysis? The symptoms of tick paralysis include weakness in the legs and arms, followed by paralysis beginning in the legs and moving upward. If unrecognized, tick paralysis may progress to respiratory failure and may be fatal in 10% of cases. What is the treatment for tick paralysis? Treatment for tick paralysis is simply removal of the tick. Once the tick is found and removed, the patient recovers fully, often within a matter of hours. It is often difficult to find the tick, which can be attached to the scalp and hidden in the hair. What can be done to prevent the spread of tick paralysis? There are no vaccines to prevent tick‐borne disease, so limiting exposure to ticks is very important. -

CONGRESSIONAL RECORD - SENATE March 31 of Staff; Without Amendment (Rept
3144 CONGRESSIONAL RECORD - SENATE March 31 of Staff; without amendment (Rept. No. to the Committee on Post Ofiice and Civil H. Con. Res. 206. Concurrent resolution 1666). Referred to the House Calendar. Service. favoring the granting of the status of per Mr. SABATH: C9mmittee on Rules. House By Mr. STOCKMAN: inanent residence to certain aliens; to the Resolution 532. Resolution to direct the H. R. 7297. A bill to prevent Federal dam Committee on the Judiciary. Committee on Education and Labor to con and reservoir projects from interfering with duct an investigation of the Wage Stabili sustained-yield timber operations; to the zation Board; with amendment (Rept. No. Committee on Public Works. PETITIONS, ETC. 1667). Referred to the House Calendar. By Mr. WILLIAMS of Mississippi: Mr. SABATH: Committee on Rules. House H. R. 7298. A bill to authorize the consoli Under clause 1 of rule XXII, petitions Resolution 520. Resolution creating a se dation of the area of Vicksburg National Mili and papers were laid on the Clerk's desk lect committee to conduct an investiga tary Park, in the State of Mississippi, and for and referred as follows: tion and study of offensive and undesirable other purposes; to the Committee on Interior 658. By Mr. SMITH of Wisconsin: Petition books and radio and television programs; and Insular Affairs. of the Milwaukee Cooperative Milk Produc without amendment (Rept. No. 1668). Re ers. Over 1,000 people were present at the ferred to the House Calendar. annual meeting on March 11, 1952, to go on Mr. MADDEN: Committee on Rules. House MEMORIALS record opposing universal military service as Resolution 591. -

The Boeing Company and the Militarymetropolitanindustrial
1/3/2017 Center for the Study of the Pacific Northwest About Us Events Classroom Materials Pacific Northwest Resources Quarterly The Boeing Company and the MilitaryMetropolitanIndustrial Complex, 19451953 Richard S. Kirkendall Pacific Northwest Quarterly 85:4 (Oct. 1994), p. 137149 This Boeing bomber embodies the transition to jet aircraft and the dependence on military that characterized company operations during the years following World War II. (Special Collections, University of Washington Libraries, Negative #10703. Photo by Boeing Company) The years of Harry Truman's presidency were crucial to the success of the Boeing Airplane Company. The president himself did not have close ties with the firm or great confidence in air power, but one part of the American state the air forcerecognized Boeing's ability to serve air force interests and was in a stronger position than ever before to pursue those interests. Furthermore, the company now had another ally willing to enter the political arena on its behalf. This was Seattle. The people there had a new commitment to Boeing. Taking advantage of cold war fears, air force leaders lobbied for funds to be spent on bombers, and Seattle people worked to draw that money to their city by way of Boeing. As a consequence of the successes of these two groups in the Truman years, the company acquired the resources it needed to become the world leader in building commercial jets. In battling for Boeing, Seattle participated in what President Dwight D. Eisenhower later called the "military industrial complex." A historian, Roger Lotchin, recently proposed "metropolitanmilitary complex" as a substitute for Eisenhower's term. -

Tick Paralysis
April 26, 1996 / Vol. 45 / No. 16 325 Tick Paralysis — Washington, 1995 326 Update: Influenza Activity — United States and Worldwide, 1995–96 Season, and Composition of the 1996–97 Influenza Vaccine 330 Multidrug-Resistant Tuberculosis Outbreak on an HIV Ward — Madrid, Spain, 1991–1995 333 Adult Blood Lead Epidemiology and Surveillance — United States, Fourth Quarter, 1995 335 Notice to Readers Tick Paralysis — Washington, 1995 Tick Paralysisparalysis (tick— Continued toxicosis)—one of the eight most common tickborne diseases in the United States (1 )—is an acute, ascending, flaccid motor paralysis that can be con- fused with Guillain-Barré syndrome, botulism, and myasthenia gravis. This report summarizes the results of the investigation of a case of tick paralysis in Washington. On April 10, 1995, a 2-year-old girl who resided in Asotin County, Washington, was taken to the emergency department of a regional hospital because of a 2-day history of unsteady gait, difficulty standing, and reluctance to walk. Other than a recent his- tory of cough, she had been healthy and had not been injured. On physical examina- tion, she was afebrile, alert, and active but could stand only briefly before requiring assistance. Cranial nerve function was intact. However, she exhibited marked extrem- ity and mild truncal ataxia, and deep tendon reflexes were absent. She was admitted with a tentative diagnosis of either Guillain-Barré syndrome or postinfectious polyradiculopathy. Within several hours of hospitalization, she had onset of drooling and tachypnea. A nurse incidentally detected an engorged tick on the girl’s hairline by an ear and re- moved the tick. -

Tick-Borne Disease Prevention Program
Tick-Borne Disease Prevention Program INTRODUCTION Hudson Valley Community College employees working outdoors, especially in areas with tall grasses, shrubs, low hanging branches, or leaf mold are susceptible to being bitten by a tick. There are several diseases which can be carried by ticks, with the most well-known in this area being Lyme disease. This document provides information about tick-borne illnesses, how to prevent tick bites and what to do if you find a tick on you. BACKGROUND Lyme Disease is a bacterial infection that can be caused by the transmission of the Borrelia burgdorferi bacteria from the bite of an infected deer tick. Deer ticks primarily transmit the Lyme Disease bacteria in the late Spring or early Summer while they are in their nymphal stage of development, but they can carry the bacteria in their larval, nymph, or adult stages at almost any time of the year. Ticks are picked up when a person’s clothing or hair brushes a leaf or other object they are on. Ticks do not jump, crawl, or fall onto a person. Once picked up, they will crawl until they find a favorable site to feed. Often they will find a spot at the back of a knee, near the hairline, or behind the ears. Deer ticks are much smaller than common dog ticks. The nymphal stage tick is usually not much larger than the head of a pin and can easily go unnoticed if attached to a person. Not all deer ticks are infected with the bacteria that cause Lyme disease. -

An Outbreak of Suspected Tick Paralysis in One
Retour au menu ENTOMOLOGIE An outbreak of suspected tick paralysis M.T. Musa l in one-humped camels (Camelus O.M. Osman 2 I dromecfarius) in the Sudan MUSA (M.T.), OSMAN (O.M.). Suspicion d’un foyer de paralysie due HISTORY a,ux tiques chez le dromadaire (Camelus dromedarius) au Soudan. Revue Elev. Méd. vét. Pays trop., 1990,43 (4) : 505-510 Before the drought years 1983-l 984, came1 nomads used Un foyer de paralysie, probablement due aux tiques, a été découvert to spend the rainy seasons further north in the semi-arid sur des dromadaires (Camelus dromedurius) dans la région de Darfur, zone. As a result of drought pressures, the traditional au Soudan. entre les latitudes 11-12” N et les lonaitudes 24-25” E. Les movement belts shifted further south. Thus, the outbreak troupeauxse trouvaient dans des zones infestéesde tiques. Dix trou- peaux, totalisant 251 animaux d’âges différents, ont été concernés, sites were adopted as dry season grazing areas by the avec une mortalité de 34,3 p. 100. 6Ïr a noté les symptômes suivants : came1 nomads and other herders. incoordination, démarche hésitante et décubitus, suivis soit par la mort, soit par la guérison. Des adultes de Zfyulomma et des nymphes, In 1987, because of the poor rains in the north, the came1 et des adultes de Rhipicephalus ont été suspectés comme agents res- nomads returned to their usual dry season residences ponsable de la maladie. Des tiques nourries expérimentalement sur exceptionnally earlier (mid-October), shortly after late cobaye ont provoqué chez ce dernier une paralysie temporaire. -
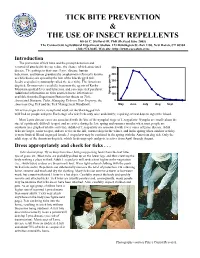
Tick Bite Prevention & the Use of Insect Repellents
TICK BITE PREVENTION & THE USE OF INSECT REPELLENTS Kirby C. Stafford III, PhD (Revised June 2005) The Connecticut Agricultural Experiment Station, 123 Huntington St.-Box 1106, New Haven, CT 06504 (203) 974-8485, Web site: http://www.caes.state.ct.us Introduction The prevention of tick bites and the prompt detection and removal of attached ticks can reduce the chance of tick-associated 500 disease. The pathogens that cause Lyme disease, human babesiosis, and human granulocytic anaplasmosis (formerly known 400 as ehrlichiosis) are spread by the bite of the blacklegged tick, Ixodes scapularis (commonly called the deer tick). The American 300 dog tick, Dermacentor variabilis, transmits the agents of Rocky 200 Mountain spotted fever and tularemia, and can cause tick paralysis. Additional information on ticks and tick-borne infections is ha per Nymphs 100 available from the Experiment Station fact sheets on Tick- Associated Diseases, Ticks, Managing Ticks on Your Property, the 0 American Dog Tick and the Tick Management Handbook. May June July Aug Sept All active stages (larva, nymph and adult) of the blacklegged tick will feed on people and pets. Each stage of a tick feeds only once and slowly; requiring several days to ingest the blood. Most Lyme disease cases are associated with the bite of the nymphal stage of I. scapularis. Nymphs are small (about the size of a pinhead), difficult to spot, and are active during the late spring and summer months when most people are outdoors (see graph of relative activity). Adults of I. scapularis are associated with fewer cases of Lyme disease.