Annex XV Report PROPOSAL for IDENTIFICATION of A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
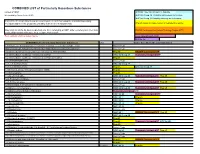
COMBINED LIST of Particularly Hazardous Substances
COMBINED LIST of Particularly Hazardous Substances revised 2/4/2021 IARC list 1 are Carcinogenic to humans list compiled by Hector Acuna, UCSB IARC list Group 2A Probably carcinogenic to humans IARC list Group 2B Possibly carcinogenic to humans If any of the chemicals listed below are used in your research then complete a Standard Operating Procedure (SOP) for the product as described in the Chemical Hygiene Plan. Prop 65 known to cause cancer or reproductive toxicity Material(s) not on the list does not preclude one from completing an SOP. Other extremely toxic chemicals KNOWN Carcinogens from National Toxicology Program (NTP) or other high hazards will require the development of an SOP. Red= added in 2020 or status change Reasonably Anticipated NTP EPA Haz list COMBINED LIST of Particularly Hazardous Substances CAS Source from where the material is listed. 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide Acutely Toxic Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- Acutely Toxic 1-(2-Chloroethyl)-3-(4-methylcyclohexyl)-1-nitrosourea (Methyl-CCNU) Prop 65 KNOWN Carcinogens NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) IARC list Group 2A Reasonably Anticipated NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) (Lomustine) Prop 65 1-(o-Chlorophenyl)thiourea Acutely Toxic 1,1,1,2-Tetrachloroethane IARC list Group 2B 1,1,2,2-Tetrachloroethane Prop 65 IARC list Group 2B 1,1-Dichloro-2,2-bis(p -chloropheny)ethylene (DDE) Prop 65 1,1-Dichloroethane -

Detection of Estrogen Receptor Endocrine Disruptor Potency of Commonly Used Organochlorine Pesticides Using the LUMI-CELL ER Bioassay
DEVELOPMENTAL AND REPRODUCTIVE TOXICITY Detection of Estrogen Receptor Endocrine Disruptor Potency of Commonly Used Organochlorine Pesticides Using The LUMI-CELL ER Bioassay John D. Gordon1, Andrew C: Chu1, Michael D. Chu2, Michael S. Denison3, George C. Clark1 1Xenobiotic Detection Systems, Inc., 1601 E. Geer St., Suite S, Durham, NC 27704, USA 2Alta Analytical Perspectives, 2714 Exchange Drive, Wilmington, NC 28405, USA 3Dept. of Environmental Toxicology, Meyer Hall, Univ. of California, Davis; Davis, CA 95616 USA Introduction Organochlorine pesticides are found in many ecosystems worldwide as result of agricultural and industrial activities and exist as complex mixtures. The use of these organochlorine pesticides has resulted in the contamination of lakes and streams, and eventually the animal and human food chain. Many of these pesticides, such as pp ’-DDT, pp ’-DDE, Kepone, Vinclozolin, and Methoxychlor (a substitute for the banned DDT), have been described as putative estrogenic endocrine disruptors, and act by mimicking endogenous estrogen 1-3 . Estrogenic compounds can have a significant detrimental effect on the endocrine and reproductive systems of both human and other animal populations 4 . Previous studies have shown a strong association between several EDCs (17p-Estradiol, DES, Zeralanol, Zeralenone, Coumestrol, Genistein, Biochanin A, Diadzein, Naringenin, Tamoxifin) and estrogenic activity via uterotropic assay, cell height, gland number, increased lactoferrin, and a transcriptional activity assay using BG1Luc4E2 cells4 . Some other examples of the effects of these EDCs are: decreased reproductive success and feminization of males in several wildlife species; increased hypospadias along with reductions in sperm counts in men; increase in the incidence of human breast and prostate cancers; and endometriosis 3-5 . -

WO 2012/148799 Al 1 November 2012 (01.11.2012) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2012/148799 Al 1 November 2012 (01.11.2012) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 9/107 (2006.01) A61K 9/00 (2006.01) kind of national protection available): AE, AG, AL, AM, A 61 47/10 (2006.0V) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, PCT/US2012/034361 HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, (22) International Filing Date: KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, 20 April 2012 (20.04.2012) MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, (26) Publication Language: English TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/480,259 28 April 201 1 (28.04.201 1) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (71) Applicant (for all designated States except US): BOARD UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, OF REGENTS, THE UNIVERSITY OF TEXAS SYS¬ TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, TEM [US/US]; 201 West 7th St., Austin, TX 78701 (US). -

Prenatal Testosterone Supplementation Alters Puberty Onset, Aggressive Behavior, and Partner Preference in Adult Male Rats
J Physiol Sci (2012) 62:123–131 DOI 10.1007/s12576-011-0190-7 ORIGINAL PAPER Prenatal testosterone supplementation alters puberty onset, aggressive behavior, and partner preference in adult male rats Cynthia Dela Cruz • Oduvaldo C. M. Pereira Received: 26 October 2011 / Accepted: 19 December 2011 / Published online: 11 January 2012 Ó The Physiological Society of Japan and Springer 2012 Abstract The objective of this study was to investigate because pregnant women exposed to hyperandrogenemia whether prenatal exposure to testosterone (T) could change and then potentially exposing their unborn children to ele- the body weight (BW), anogenital distance (AGD), ano- vated androgen levels in the uterus can undergo alteration of genital distance index (AGDI), puberty onset, social normal levels of T during the sexual differentiation period, behavior, fertility, sexual behavior, sexual preference, and T and, as a consequence, affect the reproductive and behavior level of male rats in adulthood. To test this hypothesis, patterns of their children in adulthood. pregnant rats received either 1 mg/animal of T propionate diluted in 0.1 ml peanut oil or 0.1 ml peanut oil, as control, Keywords Aggressive behavior Á Male rats Á on the 17th, 18th and 19th gestational days. No alterations in Prenatal testosterone Á Puberty onset Á Sexual behavior Á BW, AGD, AGDI, fertility, and sexual behavior were Sexual differentiation observed (p [ 0.05). Delayed onset of puberty (p \ 0.0001), increased aggressive behavior (p [ 0.05), altered pattern of sexual preference (p \ 0.05), and reduced T plasma level Introduction (p \ 0.05) were observed for adult male rats exposed pre- natally to T. -

California Proposition 65 (Prop65)
20 NOVEMBER 2018 To Whom It May Concern: Certificate of Compliance California Proposition 65 California’s Proposition 65 entitles California consumers to special warnings for products that contain chemicals known to the state of California to cause cancer and birth defects or other reproductive harm if those products expose consumers to such chemicals above certain threshold levels. This is to certify that Alliance Memory comply with Safe Drinking Water and Toxic Enforcement Act of 1986, commonly known as California Proposition 65, that are ‘known to the state to cause cancer or reproductive toxicity’ as of December 29, 2017, by following the labelling guidelines set out therein. Alliance Memory labelling system clearly states a ‘Prop65 warning’ as and when necessary, on product packaging that is destined for the state of California, USA. This document certifies that to the best of our current knowledge and belief and under normal usage, Alliance Memory’s IC products are in compliance with California Proposition 65 – The Safe Drinking Water and Toxic Enforcement Act, 1986) and do not contain chemical elements of those listed within the California Proposition 65 chemical listing as shown below. Signature : Date: 20 November 2018 Name : Kim Bagby Title : Director QRA Department/Alliance Memory California Proposition 65 list of chemicals. The following is a list of chemicals published as a requirement of Safe Drinking Water and Toxic Enforcement Act of 1986, commonly known as California Proposition 65, that are ‘known to the state to cause -

Health Effects Support Document for 1,1-Dichloro-2,2- Bis(P-Chlorophenyl)Ethylene (DDE)
Health Effects Support Document for 1,1-Dichloro-2,2- bis(p-chlorophenyl)ethylene (DDE) Health Effects Support Document for 1,1-Dichloro-2,2-bis(p-chlorophenyl)ethylene (DDE) U.S. Environmental Protection Agency Office of Water (4304T) Health and Ecological Criteria Division Washington, DC 20460 www.epa.gov/safewater/ccl/pdf/DDE.pdf EPA Document Number EPA-822-R-08-003 January, 2008 Printed on Recycled Paper DDE — January, 2008 iv FOREWORD The Safe Drinking Water Act (SDWA), as amended in 1996, requires the Administrator of the Environmental Protection Agency (EPA) to establish a list of contaminants to aid the Agency in regulatory priority setting for the drinking water program. In addition, the SDWA requires EPA to make regulatory determinations for no fewer than five contaminants by August 2001 and every five years thereafter. The criteria used to determine whether or not to regulate a chemical on the Contaminant Candidate List (CCL) are the following: • The contaminant may have an adverse effect on the health of persons. • The contaminant is known to occur or there is a substantial likelihood that the contaminant will occur in public water systems with a frequency and at levels of public health concern. • In the sole judgment of the Administrator, regulation of such contaminant presents a meaningful opportunity for health risk reduction for persons served by public water systems. The Agency’s findings for all three criteria are used in making a determination to regulate a contaminant. The Agency may determine that there is no need for regulation when a contaminant fails to meet one of the criteria. -

Report on Pesticide Rapid Assessments
REPORT ON PESTICIDE RAPID ASSESSMENTS Minnesota Department of Health This report was prepared by the Minnesota Department of Health (MDH), Drinking Water Contaminants of Emerging Concern Program; Dan Balluff, Alexandra Barber, Jim Jacobus, Sarah Johnson, and Pam Shubat. The Pesticide Rapid Assessment Project was made possible by funds from the Clean Water Fund, from the Clean Water, Land and Legacy Amendment. For more information: Drinking Water Contaminants of Emerging Concern Program Phone: 651-201-4899 Website: www.health.state.mn.us/cec Email: [email protected] December 2014 Table of Contents Executive Summary 4 Background 5 Methods for Conducting Rapid Assessments 6 Results 10 Discussion 13 Table 1: Pesticides listed by MDA for which current assessments were available or are pending 16 Table 2: Pesticide degradates for which MDH recommends the non-cancer rapid assessment of a surrogate chemical 17 References 18 Appendix A: Rapid Assessments Table 20 Executive Summary The Minnesota Department of Health (MDH) Health Risk Assessment Unit developed a new, rapid way to assess health risks of chemicals in drinking water. Rapid assessments were completed for 159 pesticides selected by the Minnesota Department of Agriculture or Minnesota Department of Health. The chemicals were selected because no MDH drinking water guidance was available or the guidance was outdated. The result of a rapid assessment is an amount of chemical in water that is unlikely to harm people who drink the water. MDH used information on toxic (harmful) effects of pesticides and risk assessment methods used by MDH for other types of drinking water guidance. The values that result from the rapid assessments are likely to be low compared to the result MDH would produce from an in-depth and lengthy review of the same chemical. -

Pesticides in Streams in New Jersey and Long Island, New
PESTICIDES IN STREAMS IN NEW JERSEY National Water-Quality AND LONG ISLAND, NEW YORK, AND Assessment Program Long Island - New Jersey RELATION TO LAND USE Study Unit Abstract Pesticide compounds were detected in all 50 water samples collected from streams in New Jersey and Long Island, New York, during June 9-18, 1997. Samples were analyzed for 47 compounds, of which 25 were detected. The number of pesticides detected at each site ranged from 1 to 14. The seven most frequently detected pesticides were atrazine (in 93 percent of samples), metolachlor (86 percent), prometon (84 percent), desethyl-atrazine (78 percent), simazine (78 percent), carbaryl (44 percent), and diazinon (44 percent). All pesticide concentrations were within both U.S. Environmental Protection Agency (USEPA) and State maximum contami- nant levels (MCL’s) for drinking water and USEPA lifetime health advisory levels (HAL’s). Concentrations of dieldrin and methyl- azinphos at one or more sites, however, equaled or exceeded a Federal or State water-quality criterion for aquatic life. The pesticides detected in a stream were related to the land-use composition of the basin. Detection frequencies of 14 of the 25 pesticides detected were highest at agricultural sites; acetochlor, azinphos-methyl, carbofuran, and pebulate were detected only at agricultural sites. Seven compounds were detected most frequently at urban sites; trifluralin, dieldrin, napropamide, and benfluralin were detected only at urban sites. Four compounds were detected most frequently at sites draining areas of mixed land use. No pesticides were detected most frequently at sites draining forested areas. The median concentration and the detection frequency of a given pesticide always were highest in samples from sites in the same land-use category.The median concentrations of seven pesticides at the agricultural sites were at least twice as high as the median concentrations at sites in other land-use categories. -

L Earl Gray Jr
Effects of mixtures of phthalates and other toxicants on sexual differentiation in rats: A risk assessment framework based upon disruption of common developing systems USEPAUSEPA scientistscientist grapplesgrapples withwith difficultdifficult environmentalenvironmental issuesissues L Earl Gray Jr. This presentation does not necessarily reflect USEPA policy, but rather represents the author’s current view on the state of the science Reproductive Toxicology Branch, NHEERL, ORD, USEPA EstrogensEstrogens Developmental MethoxychlorMethoxychlor Reproductive Toxicants EthinylEthinyl EstradiolEstradiol BisphenolBisphenol AA InhibitorsInhibitors ofof fetalfetal FetalFetal GermGerm CellCell ToxicantsToxicants ARAR AntagonistsAntagonists androgenandrogen synthesissynthesis BusulfanBusulfan DiazoDiazo dyesdyes CompeteCompete withwith naturalnatural PreventPrevent thethe synthesissynthesis ofof hormoneshormones TT andand DHTDHT forfor AR,AR, naturalnatural hormoneshormones TT andand SteroidogenesisSteroidogenesis inhibitorsinhibitors prevent AR-DNA binding in prevent AR-DNA binding in DHTDHT andand cancan induceinduce ProchlorazProchloraz vitro,vitro, inhibitinhibit AR-dependentAR-dependent malformations in male malformations in male Linuron genegene expressionexpression inin vivo,vivo, andand reproductivereproductive tracttract andand Linuron maymay induceinduce malformationsmalformations inin delaydelay pubertypuberty inin malemale ratrat KetoconazoleKetoconazole malemale reproductivereproductive tracttract andand FenarimolFenarimol delaydelay pubertypuberty -
Changes in Soil Microbial Community and Activity Caused by Application
www.nature.com/scientificreports OPEN Changes in soil microbial community and activity caused by application of dimethachlor and linuron Juraj Medo1*, Jana Maková1, Janka Medová2, Nikola Lipková1, Renata Cinkocki1, Radoslav Omelka3 & Soňa Javoreková1 Soil microorganisms and their activities are essential for maintaining soil health and fertility. Microorganisms can be negatively afected by application of herbicides. Although efects of herbicides on microorganisms are widely studied, there is a lack of information for chloroacetamide herbicide dimethachlor. Thus, dimethachlor and well known linuron were applied to silty-loam luvisol and their efects on microorganisms were evaluated during112 days long laboratory assay. Dimethachlor and linuron were applied in doses 1.0 kg ha−1 and 0.8 kg ha−1 corresponding to 3.33 mg kg−1 and 2.66 mg kg−1 respectively. Also 100-fold doses were used for magnifcation of impacts. Linuron in 100-fold dose caused minor increase of respiration, temporal increase of soil microbial biomass, decrease of soil dehydrogenase activity, and altered microbial community. Dimethachlor in 100-fold dose signifcantly increased respiration; microbial biomass and decreased soil enzymatic activities. Microbial composition changed signifcantly, Proteobacteria abundance, particularly Pseudomonas and Achromobacter genera increased from 7 to 28th day. In-silico prediction of microbial gene expression by PICRUSt2 software revealed increased expression of genes related to xenobiotic degradation pathways. Evaluated characteristics of microbial community and activity were not afected by herbicides in recommended doses and the responsible use of both herbicides will not harm soil microbial community. Modern agriculture depends heavily on pesticide use. Majority of the used pesticides are herbicides applied to almost all crops in conventional agriculture systems 1. -

NEWS 02 2020 ENG.Qxp Layout 1
Polymers and fluorescence Balance of power 360° drinking water analysis trilogy Fluorescence spectroscopy LCMS-8060NX: performance of industrial base polymers and robustness without Automatic, simultaneous and compromising sensitivity rapid analysis of pesticides and speed CONTENT APPLICATION »Plug und Play« disease screening solution? – The MALDI-8020 in screening for Sickle Cell Disease 4 Customized software solutions for any measurement – Macro programming for Shimadzu UV-Vis and FTIR 8 Ensuring steroid-free food supplements – Identification of steroids in pharmaceuticals and food supplements with LCMS-8045 11 MSn analysis of nonderivatized and Mtpp-derivatized peptides – Two recent studies applying LCMS-IT-TOF instruments 18 Polymers and fluorescence – Part 2: How much fluorescence does a polymer show during quality control? 26 PRODUCTS The balance of power – LCMS-8060NX balances enhanced performance and robustness 7 360° drinking water analysis: Episode 2 – Automatic, simul- taneous and rapid analysis of pesticides in drinking water by online SPE and UHPLC-MS/MS 14 Versatile testing tool for the automotive industry – Enrico Davoli with the PESI-MS system (research-use only [RUO] instrument) New HMV-G3 Series 17 No more headaches! A guide to choosing the perfect C18 column 22 Validated method for monoclonal antibody drugs – Assessment of the nSMOL methodology in Global solution through the validation of bevacizumab in human serum 24 global collaboration LATEST NEWS Global solution through global collaboration – Shimadzu Cancer diagnosis: -

OECD Test Guideline 441: Hershberger Bioassay in Rats
OECD/OCDE 441 Adopted: 7 September 2009 OECD GUIDELINE FOR THE TESTING OF CHEMICALS Hershberger Bioassay in Rats: A Short-term Screening Assay for (Anti)Androgenic Properties INTRODUCTION 1. The OECD initiated a high-priority activity in 1998 to revise existing guidelines and to develop new guidelines for the screening and testing of potential endocrine disrupters (1). One element of the activity was to develop a Test Guideline for the rat Hershberger Bioassay. After several decades of use by the pharmaceutical industry, this assay was first standardized by an official expert committee in 1962 as a screening tool for androgenic chemicals (2). In 2001-2007, the rat Hershberger Bioassay has undergone an extensive validation programme including the generation of a Background Review Document (23), compilation of a detailed methods paper (3), development of a dissection guide (21) and the conduct of extensive intra- and interlaboratory studies to show the reliability and reproducibility of the bioassay. These validation studies were conducted with a potent reference androgen (testosterone propionate (TP)), two potent synthetic androgens (trenbolone acetate and methyl testosterone), a potent antiandrogenic pharmaceutical (flutamide), a potent inhibitor of the synthesis (finasteride) of the natural androgen (dihydrotestosterone-DHT), several weakly antiandrogenic pesticides (linuron, vinclozolin, procymidone, p,p’ DDE), a potent 5α reductase inhibitor (finasteride) and two known negative chemicals (dinitrophenol and nonylphenol) (4) (5) (6) (7) (8). This Test Guideline is the outcome of the long historical experience with the bioassay and the experience gained during the validation test programme and the results obtained therein. 2. The Hershberger Bioassay is a short-term in vivo screening test using accessory tissues of the male reproductive tract.