Axillary Brachial Plexus Block: Landmark Techniques
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Neurology of the Upper Limb
Neurology of the Upper limb Donald Sammut Hand Surgeon Kings Upper Limb Anatomy plus lecture notes The$Neck$ The$Nerve$roots$which$supply$the$Upper$Limb$are$C5$to$T1$ Pre<fixed$(C4$to$C8)$and$Post<fixed$(C6$to$T2)$plexus$not$uncommon.$ Also$common$contributions$from$C4$and$from$T2$in$a$normally$rooted$plexus.$ $ The$anterior$nerve$roots$emerge$between$the$vertebrae$and$immediately$pass$ $through$the$first$area$of$possible$compression:$ The$root$nerve$canal$is$bounded$$ Anteriorly$by$the$posterior$margin$of$the$intervertebral$disc$and$$ Posteriorly,$by$the$facet$joint$between$vertebrae.$ $ Pathology$of$the$disc,$or$joint,$or$both,$can$narrow$this$channel$and$compress$ $the$nerve$root$ The$roots$emerge$from$the$cervical$spine$into$the$plane$between$$ Scalenius$Anterior$and$Scalenius$Medius.$$ $ Scalenius*Anterior:** Origin:$Anterior$tubercles$of$Cervical$vertebae$C3$to$6$(C6$tubercle$is$the$Carotid$tubercle)$ Insertion:$The$scalene$tubercle$on$inner$border/upper$surface$1st$rib$ $ Scalenius*Medius:* Origin:$Posterior$tubercles$of$all$cervical$vertebrae$ Insertion:$Quadrangular$area$between$the$neck$and$subclavian$groove$1st$rib$ $ Exiting$from$the$Scalenes,$the$trunks$lie$in$the$posterior$triangle$of$the$neck.$ The$posterior$triangle$is$bounded$anteriorly$by$SternoCleidoMastoid$and$$ posteriorly$by$the$Trapezius.$ The$inferior$border$is$the$clavicle$.$ The$apex$of$the$triangle$superiorly$is$at$the$back$of$the$skull$on$the$superior$nuchal$line$ $ $ The$Posterior$Triangle$ SternoCleidoMastoid$ Trapezius$ Scalenius$Medius$ Scalenius$Anterior$ -
Brachial Plexus and Branches Axillary A
Regional Anatomy of the Upper Limb 1 Wu Genghua Medical College Yangzhou University Anterior surface of the •Incisions: Upper Limb Make the skin incisions indicated in figure and reflect the skin flaps. Be careful not to cut too deep. As you remove the skin, look for the cephalic v., basilic v. and median cubital v. Superficial veins and nerves Mamma Structures Contains skin, mammary glands and adipose tissue Consists of 15 to 20 Lobes of mammary gland that radiate outward from the nipple lactiferous duct lactiferous sinuse Suspensory ligaments of breast (cooper’s ligaments): connective tissue septa that extend from the skin to the deep fascia Pectoral Region Superficial structures Superficial n. Supraclavicular n. Anterior cutaneous branches of intercostal n. lateral cutaneous branches of intercostal n. Muscles connecting the upper limb to the thoracic wall Pectoralis major 胸大肌 Subclevius 锁骨下肌 Pectoralis minor 胸小肌 Serratus anterior 前锯肌 Pectoral Region Deep structures clavipectoral fascia The deep fascia which extends between subclavius, coracoid process and pectoralis minor muscles The structures pass through the clavipectoral fascia . Cephalic v. Thoracoacromial a. Lateral pectoral n. Axillary region 腋区 Boundaries of the axillary fossa Apex is bounded by Middle 1/3 of clavicle Lateral border of first rib Upper border of the scapula Base is formed by the skin stretching between the anterior and posterior walls Anterior wall Formed by pectoralis major, pectoralis minor and subclavius muscles Boundaries of the axillary fossa The posterior wall latissimus dorsi teres major subscapularis and scapula Trilateral and quadrilateral space The posterior humeral circumflex a. and axillary n. pass through the quadrilateral foramen. -
Pectoral Region and Axilla Doctors Notes Notes/Extra Explanation Editing File Objectives
Color Code Important Pectoral Region and Axilla Doctors Notes Notes/Extra explanation Editing File Objectives By the end of the lecture the students should be able to : Identify and describe the muscles of the pectoral region. I. Pectoralis major. II. Pectoralis minor. III. Subclavius. IV. Serratus anterior. Describe and demonstrate the boundaries and contents of the axilla. Describe the formation of the brachial plexus and its branches. The movements of the upper limb Note: differentiate between the different regions Flexion & extension of Flexion & extension of Flexion & extension of wrist = hand elbow = forearm shoulder = arm = humerus I. Pectoralis Major Origin 2 heads Clavicular head: From Medial ½ of the front of the clavicle. Sternocostal head: From; Sternum. Upper 6 costal cartilages. Aponeurosis of the external oblique muscle. Insertion Lateral lip of bicipital groove (humerus)* Costal cartilage (hyaline Nerve Supply Medial & lateral pectoral nerves. cartilage that connects the ribs to the sternum) Action Adduction and medial rotation of the arm. Recall what we took in foundation: Only the clavicular head helps in flexion of arm Muscles are attached to bones / (shoulder). ligaments / cartilage by 1) tendons * 3 muscles are attached at the bicipital groove: 2) aponeurosis Latissimus dorsi, pectoral major, teres major 3) raphe Extra Extra picture for understanding II. Pectoralis Minor Origin From 3rd ,4th, & 5th ribs close to their costal cartilages. Insertion Coracoid process (scapula)* 3 Nerve Supply Medial pectoral nerve. 4 Action 1. Depression of the shoulder. 5 2. Draw the ribs upward and outwards during deep inspiration. *Don’t confuse the coracoid process on the scapula with the coronoid process on the ulna Extra III. -

Section 1 Upper Limb Anatomy 1) with Regard to the Pectoral Girdle
Section 1 Upper Limb Anatomy 1) With regard to the pectoral girdle: a) contains three joints, the sternoclavicular, the acromioclavicular and the glenohumeral b) serratus anterior, the rhomboids and subclavius attach the scapula to the axial skeleton c) pectoralis major and deltoid are the only muscular attachments between the clavicle and the upper limb d) teres major provides attachment between the axial skeleton and the girdle 2) Choose the odd muscle out as regards insertion/origin: a) supraspinatus b) subscapularis c) biceps d) teres minor e) deltoid 3) Which muscle does not insert in or next to the intertubecular groove of the upper humerus? a) pectoralis major b) pectoralis minor c) latissimus dorsi d) teres major 4) Identify the incorrect pairing for testing muscles: a) latissimus dorsi – abduct to 60° and adduct against resistance b) trapezius – shrug shoulders against resistance c) rhomboids – place hands on hips and draw elbows back and scapulae together d) serratus anterior – push with arms outstretched against a wall 5) Identify the incorrect innervation: a) subclavius – own nerve from the brachial plexus b) serratus anterior – long thoracic nerve c) clavicular head of pectoralis major – medial pectoral nerve d) latissimus dorsi – dorsal scapular nerve e) trapezius – accessory nerve 6) Which muscle does not extend from the posterior surface of the scapula to the greater tubercle of the humerus? a) teres major b) infraspinatus c) supraspinatus d) teres minor 7) With regard to action, which muscle is the odd one out? a) teres -

Hand and Foot Musculature of Anura: Structure, Homology, Terminology, and Synapomorphies for Major Clades
HAND AND FOOT MUSCULATURE OF ANURA: STRUCTURE, HOMOLOGY, TERMINOLOGY, AND SYNAPOMORPHIES FOR MAJOR CLADES BORIS L. BLOTTO, MARTÍN O. PEREYRA, TARAN GRANT, AND JULIÁN FAIVOVICH BULLETIN OF THE AMERICAN MUSEUM OF NATURAL HISTORY HAND AND FOOT MUSCULATURE OF ANURA: STRUCTURE, HOMOLOGY, TERMINOLOGY, AND SYNAPOMORPHIES FOR MAJOR CLADES BORIS L. BLOTTO Departamento de Zoologia, Instituto de Biociências, Universidade de São Paulo, São Paulo, Brazil; División Herpetología, Museo Argentino de Ciencias Naturales “Bernardino Rivadavia”–CONICET, Buenos Aires, Argentina MARTÍN O. PEREYRA División Herpetología, Museo Argentino de Ciencias Naturales “Bernardino Rivadavia”–CONICET, Buenos Aires, Argentina; Laboratorio de Genética Evolutiva “Claudio J. Bidau,” Instituto de Biología Subtropical–CONICET, Facultad de Ciencias Exactas Químicas y Naturales, Universidad Nacional de Misiones, Posadas, Misiones, Argentina TARAN GRANT Departamento de Zoologia, Instituto de Biociências, Universidade de São Paulo, São Paulo, Brazil; Coleção de Anfíbios, Museu de Zoologia, Universidade de São Paulo, São Paulo, Brazil; Research Associate, Herpetology, Division of Vertebrate Zoology, American Museum of Natural History JULIÁN FAIVOVICH División Herpetología, Museo Argentino de Ciencias Naturales “Bernardino Rivadavia”–CONICET, Buenos Aires, Argentina; Departamento de Biodiversidad y Biología Experimental, Facultad de Ciencias Exactas y Naturales, Universidad de Buenos Aires, Buenos Aires, Argentina; Research Associate, Herpetology, Division of Vertebrate Zoology, American -

GALEN on Anatomical Procedures
GALEN On Anatomical Procedures TRANSLATION WITH INTRODUCTION AND NOTES BY CHARLES SINGER Until recent years the works of Galen, the greatest and most prolific medical writer of antiquity, were closed books to the modern reader. Professor Singer has now added another to the very few works of Galen which have been translated from the Greek into English. Galen's work entitled De anatomicis administrationihus is the text of lectures on anatomy delivered in Rome about a.d. 177. The Greek text was translated into Latin in 153 1, and in this form the work had a profound influence on Vesalius and other great Renaissance anatomists. Although Galen had some knowledge ofhuman anatomy, especially of the bones, most of his dis^ section was done on the Rhesus monkey and the Barbary ape, in which many parts show marked differences from their human counterparts. Professor Singer has not only provided a scholarly translation of Galen's text, but he has also identic fied wherever possible the structures men^ tioned, and has attached to them their modern anatomical names. The book provides a basis for the study ofthe sources available for the foundation of modern anatomy. The dissection scene on the front of this jacket illustrates Galen demonstrating on a pig. Itjirst appeared on the title page of the Giunta edition of Galen s Works, Venice 1541-2. ^js. 6d. net Digitized by tlie Internet Arcliive in 2014 Iittps://arcliive.org/details/b20457194 PUBLICATIONS OF THE WELLCOME HISTORICAL MEDICAL MUSEUM NEW SERIES, NO. 7 GALEN ON ANATOMICAL PROCEDURES PUBLICATIONS OF THE WELLCOME HISTORICAL MEDICAL MUSEUM NEW SERIES {General Editor: Dr. -
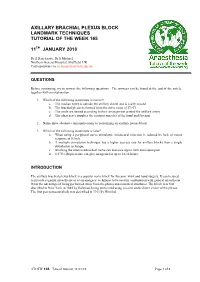
165 Axillary Brachial Plexus Block. Landmark Techniques
AXILLARY BRACHIAL PLEXUS BLOCK LANDMARK TECHNIQUES TUTORIAL OF THE WEEK 165 11TH JANUARY 2010 Dr Z Harclerode, Dr S Michael Northern General Hospital, Sheffield, UK Correspondence to [email protected] QUESTIONS Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation. 1. Which of the following statements is correct? a. The median nerve is outside the axillary sheath and is easily missed b. The brachial plexus is formed from the nerve roots of C3-T1 c. The cords are named according to their arrangement around the axillary artery d. The ulnar nerve supplies the extensor muscles of the hand and forearm 2. Name three absolute contraindications to performing an axillary plexus block 3. Which of the following statements is false? a. When using a peripheral nerve stimulator, intraneural injection is reduced by lack of motor response at 0.3mA b. A multiple stimulation technique has a higher success rate for axillary blocks than a single stimulation technique c. Blocking the intercostobrachial nerve can decrease upper limb tourniquet pain d. 0.375% Bupivacaine can give analgesia for up to 14-16 hours. INTRODUCTION The axillary brachial plexus block is a popular nerve block for forearm, wrist and hand surgery. It can be used to provide regional anaesthesia or as an analgesic technique to be used in combination with general anaesthesia. It has the advantage of being performed away from the pleura and neuraxial structures. The block was first described in New York in 1884 by Halstead, being performed using cocaine under direct vision of the plexus. -

The Axilla Summary
The Axilla It is a pyramid shaped space between the upper part of the arm and the side of the chest It forms an important passage for nerves, blood, and lymph vessels as they travel from the root of the neck to the upper limb Apex (cervico-axillary canal): The upper end of the axilla Boundaries: Front clavicle Behind upper border of the scapula Medially the outer border of the first rib Base of the Axilla Boundaries: Front pectoralis major muscle (anterior axillary fold) by the tendon of latissimus dorsi and the teres Behind major muscle (the posterior axillary fold) Medially chest wall Walls of the Axilla By the pectoralis major, subclavius, and Anterior wall pectoralis minor muscles By the coracobrachialis and biceps muscles in Lateral wall the bicipital groove of the humerus By the upper four or five ribs and the Medial wall intercostal spaces covered by the serratus anterior muscle By the subscapularis, latissimus dorsi, and teres Posterior wall major muscles from above down Contents of the Axilla 1-Axillary artery and its branches 2-Axillary vein 3-Lymph vessels and lymph nodes 4- Brachial plexus Axillary artery Course Begins: at the lateral border of the 1st rib as a Ends: at the lower border of the teres major muscle, continuation of the subclavian artery where it continues as the brachial artery Throughout its course, the artery is closely related to the cords of the brachial plexus and their branches and is enclosed with them in a connective tissue sheath called THE AXILLARY SHEATH The Pectoralis minor muscle crosses -

Brachial Plexus, Which Innervates the Upper Limb
The Upper Limbs Basic Anatomy The upper limb is a multijointed lever that is freely movable on the trunk at the shoulder joint. At the distal end of the upper limb is the important organ, the hand. Much of the importance of the hand depends on the pincer-like action of the thumb, which enables one to grasp objects between the thumb and index finger. The upper limb is divided into the shoulder (junction of the trunk with the arm), arm, elbow, forearm, wrist, and hand. Bones of the Shoulder Girdle and Arm The shoulder girdle consists of the clavicle and the scapula, which articulate with one another at the acromioclavicular joint. Muscle attachments to the bones of the thorax, clavicle, scapula, and humerus. Clavicle The clavicle is a long, slender bone that lies horizontally across the root of the neck just beneath the skin. It articulates with the sternum and 1st costal cartilage medially and with the acromion process of the scapula laterally. The clavicle acts as a strut that holds the arm away from the trunk. It also transmits forces from the upper limb to the axial skeleton and provides attachment for muscles. The medial two thirds of the clavicle is convex forward and its lateral third is concave forward. Important muscular and ligamentous attachments to the right clavicle. Scapula The scapula is a flat triangular bone that lies on the posterior chest wall between the 2nd and 7th ribs. On its posterior surface, the spine of the scapula projects backward. The lateral end of the spine is free and forms the acromion, which articulates with the clavicle. -

Peripheral Nerves and Plexus. Questions. Questions 1 – 12
EANS/UEMS European examination in neurosurgery Part I (written) Variants of questions with answers (compilation - Vyacheslav S. Botev, Department of Neurosurgery, M.Gorky Donetsk National Medical University) Peripheral Nerves and Plexus. Questions. Questions 1 – 12 Directions: The questions below consist of lettered headings from figure followed by a set of numbered items. For each numbered item select one heading with which it is most closely associated. Each lettered heading may be used once, more than once, or not at all. 1. Nerve supplies muscles that are antagonists to the serratus anterior. 2. Injury to this nerve may result in winged scapula. 3. Innervates teres minor muscle. 4. Injury to this nerve will result in flexion weakness, especially when the forearm is supine. 5. Innervates supinator muscle. 6. Nerve most commonly affected by entrapment neuropathy. 7. A pure lesion of a branch of this nerve can result in weakness of the long flexors of the thumb and index finger (producing a pinch sign) and pronator quadratus. 8. Injury of this nerve may occur in Guayan’s canal. 9. Compression of this nerve may occur by a ligament that bridges the supracondylar process to the medial epicondyle. 10. Innervates the interossei muscles. 11. Supplies sensation to the anteromedial and posteromedial forearm down to the wrist. 12. Entrapment in quadrilateral space. Questions 13 – 17 Directions: The questions below consist of lettered headings from figure followed by a set of numbered items. For each numbered item select one heading with which it is most closely associated. Each lettered heading may be used once, more than once, or not at all. -

United States National Museum Bulletin 273
SMITHSONIAN INSTITUTION MUSEUM O F NATURAL HISTORY UNITED STATES NATIONAL MUSEUM BULLETIN 273 The Muscular System of the Red Howling Monkey MIGUEL A. SCHON The Johns Hopkins University School of Medicine SMITHSONIAN INSTITUTION PRESS WASHINGTON, D.C. 1968 Publications of the United States National Museum The scientific publications of the United States National Museum include two series, Proceedings of the United States National Museum and United States National Museum Bulletin. In these series are published original articles and monographs dealing with the collections and work of the Museum and setting forth newly acquired facts in the fields of anthropology, biology, geology, history, and technology. Copies of each publication are distributed to libraries and scientific organizations and to specialists and others interested in the various subjects. The Proceedings, begun in 1878, are intended for the publication, in separate form, of shorter papers. These are gathered in volumes, octavo in size, with the publication date of each paper recorded in the table of contents of the volume. In the Bulletin series, the first of which was issued in 1875, appear longer, separate publications consisting of monographs (occasionally in several parts) and volumes in which are collected works on related subjects. Bulletins are either octavo or quarto in size, depending on the needs of the presentation. Since 1902, papers relating to the botanical collections of the Museum have been published in the Bulletin series under the heading Contributions from the United States National Herbarium. This work forms number 273 of the Bulletin series. Frank A. Taylor Director, United States National Museum U.S. -

Ultrasound Guided Axillary Brachial Plexus Block
R E G I O N A L A N A E S T H E S I A Tutorial 326 Ultrasound Guided Axillary Brachial Plexus Block Dr Robin Wingate Clinical Fellow, Royal Surrey County Hospital, UK Dr Gillian Foxall Anaesthetic Consultant, Royal Surrey County Hospital, UK Edited by: Dr Kim Russon th 4 MAR 2016 Correspondence to [email protected] QUESTIONS Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation. Please answer True or False: 1. Regarding ultrasound guided axillary brachial plexus block: a. A low frequency probe is used b. Arm abduction over 90o may be useful in identifying vascular structures c. The main landmark is the pulsatile, hyperechoic axillary artery which lies in close proximity to the nerves d. The ultrasound probe is placed transversely, approximately at the level at the junction of teres major and biceps brachii e. It can be performed by either an in-plane or out of plane technique 2. The following nerves provides cutaneous supply to the lateral forearm: a. Musculocutaneous nerve b. Ulnar nerve c. Radial nerve d. Median nerve e. Axillary nerve 3. The following statements are true: a. It is necessary to block the musculocutaneous nerve for elbow surgery b. A separate injection is usually required for the musculocutaneous nerve c. The radial nerve lies deep to the axillary artery d. The ulnar nerve lies lateral to the axillary artery e. It is possible to block the intercostobrachial nerve separately using ultrasound Key Points INTRODUCTION • Ultrasound guided axillary block is a safe, This article will focus on ultrasound guided approach to axillary reliable block of the brachial plexus.