Primary Angiomyolipoma of the Pelvic Region
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primary Mixed Myosarcoma of the Uterine Tube: a Case Report and Review of the Literature ALEXANDER S
Med. J. 258 CASE REPORT: MYOSAIRCOMAMYOSARCOMA OFUTERINEOF UTERINE TUBE Canad.Feb. 3, 1968, Ass.vol. 98 dans 1'cesophage superieur. Le plus petit malade REFERENCES chez qui une biopsie fut prelevee pesait 13 livres 1. CROSBY, W. H.: Amer. or. Dig. Dis., 8: 2, 1963. 2. CAREY, J. B., JR.: Gastroenterology, 46: 550, 1964. et 6tait age de 9 mois. 3. BECK, L T. et al.: Bull. Gastroint. EBndosc., 11: 15, 1965. We wish to thank 0. H. Kimbell, Ph.D., H. Robidoux- 4. MCDONALD, W. G.: Gastroenterology, 51: 390, 1966. 5. PARTIN, J. C. AND SCHUBERT, W. K: New Eng. J. Poirier, R.N., R.-M. Leblanc, R.N., D. Michaud, R.N., Med., 274: 94, 1966. and Marc Gigu6re, R.B.P., for their co-operation and 6. KUITUNEN, P. AND VISAKORPI, J. K.: Lancet, 1: 1276, active assistance. 1965. Primary Mixed Myosarcoma of the Uterine Tube: A Case Report and Review of the Literature ALEXANDER S. ULLMANN, M.D. and MAERIT B. KALLET, M.D., Detroit, Mich., U.S.A. SINCE primary malignant neoplasms of the uterine tube are so rare that no one indi- vidual or clinic has been able to study a large series of patients, the importance of reporting every case has often been emphasized.2-4 Although over 800 cases of primary carcinoma of the tube have been described in the liter- ature,4 up to 1956 only 30 authentic cases of primary sarcoma had been reported and to this number Abrams added another one.1' 8 Recently we had the opportunity to study a patient with primary sarcoma of the fallopian tube. -

Angiomyolipoma of the Cervix – Report of a Rare Entity
Internet Journal of Medical Update. 2017 July;12(2):13-15. doi: 10.4314/ijmu.v12i2.4 Internet Journal of Medical Update Journal home page: http://www.akspublication.com/ijmu Case Report Angiomyolipoma of the cervix – report of a rare entity N. Hariharanadha Sarmaᴪ1, Rama Srivastava2, Smriti Agnihotri3 1Consultant Pathologist, Department of Pathology, RDT Hospital, Bathalapalli, Andhra Pradesh, India 2Professor, Department of Pathology, SSR Medical College, Belle Rive, Mauritius 3Professor, Department of Pathology, American University of Antigua College of Medicine, Antigua & Barbuda, WI (Received 22 September 2017 and accepted 04 October 2017) ABSTRACT: Angiomyolipoma (AML) is a mesenchymal neoplasm seen usually in the kidney. Few cases of extra renal AML have been documented in various organs including the female genital tract, where the uterus is the most common site. To the best of our knowledge, only 4 cases of AML in the cervix have been reported in the literature. Association of AML with tuberous sclerosis is well known. Presently AML is included in the spectrum of disease entities called PEComa. We report a case of AML without tuberous sclerosis arising from the uterine cervix, which has to be differentiated from lipoleiomyoma. KEY WORDS: Angiomyolipoma; Uterine cervix; PEComas; Uterine tumor INTRODUCTIONV localization8, and mostly in females over 409. The occurrence of AML in the cervix without Angiomyolipoma (AML) occurs most frequently in concurrent incidence in the kidney is extremely the kidney, where it is closely related to tuberous rare, and only four cases have been reported in the sclerosis complex (TSC)1,2, occasionally in other scientific literature10. We are reporting a case of organs, most commonly the liver, but occurrence at uterine cervix AML without tuberous sclerosis other sites is extremely rare3. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

Uterine Carcinosarcoma Associated with Pelvic Radiotherapy for Sacral Chordoma: a Case Report
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Available online at www.sciencedirect.com Taiwanese Journal of Obstetrics & Gynecology 51 (2012) 89e92 www.tjog-online.com Case Report Uterine carcinosarcoma associated with pelvic radiotherapy for sacral chordoma: A case report Korhan Kahraman a,*, Fırat Ortac a, Duygu Kankaya b, Gulsah Aynaoglu a a Department of Obstetrics and Gynecology, Ankara University School of Medicine, Ankara, Turkey b Department of Pathology, Ankara University School of Medicine, Ankara, Turkey Accepted 28 December 2010 Abstract Objective: Postirradiation sarcoma of the female genital tract is rare, but a recognized event. Most reported cases have been associated with history of radiotherapy for various gynecologic conditions, particularly cancer of the uterine cervix and abnormal uterine bleeding. The occurrence of uterine sarcoma secondary to radiotherapy for a non-gynecologic tumor and, furthermore, this condition being simultaneous with the recurrence of primary tumor is unique. Case Report: A 67-year-old woman presented with a uterine mass which was diagnosed as a sarcoma by endometrial curettage and history of pelvic radiotherapy 23 years previously for sacral chordoma. Surgical staging procedure for uterine malignancy was performed. The final pathologic diagnosis was carcinosarcoma of the uterus. Conclusion: In uterine masses seen in patients with history of irradiation to the pelvic field, the probability of uterine sarcomas should always be kept in mind. These tumors may occur simultaneously with recurrence of primary tumor previously treated by adjuvant radiation therapy. Copyright Ó 2012, Taiwan Association of Obstetrics & Gynecology. Published by Elsevier Taiwan LLC. -

Diagnostic Immunohistochemistry for Canine Cutaneous Round Cell Tumours — Retrospective Analysis of 60 Cases
FOLIA HISTOCHEMICA ORIGINAL PAPER ET CYTOBIOLOGICA Vol. 57, No. 3, 2019 pp. 146–154 Diagnostic immunohistochemistry for canine cutaneous round cell tumours — retrospective analysis of 60 cases Katarzyna Pazdzior-Czapula, Mateusz Mikiewicz, Michal Gesek, Cezary Zwolinski, Iwona Otrocka-Domagala Department of Pathological Anatomy, Faculty of Veterinary Medicine, University of Warmia and Mazury in Olsztyn, Olsztyn, Poland Abstract Introduction. Canine cutaneous round cell tumours (CCRCTs) include various benign and malignant neoplastic processes. Due to their similar morphology, the diagnosis of CCRCTs based on histopathological examination alone can be challenging, often necessitating ancillary immunohistochemical (IHC) analysis. This study presents a retrospective analysis of CCRCTs. Materials and methods. This study includes 60 cases of CCRCTs, including 55 solitary and 5 multiple tumours, evaluated immunohistochemically using a basic antibody panel (MHCII, CD18, Iba1, CD3, CD79a, CD20 and mast cell tryptase) and, when appropriate, extended antibody panel (vimentin, desmin, a-SMA, S-100, melan-A and pan-keratin). Additionally, histochemical stainings (May-Grünwald-Giemsa and methyl green pyronine) were performed. Results. IHC analysis using a basic antibody panel revealed 27 cases of histiocytoma, one case of histiocytic sarcoma, 18 cases of cutaneous lymphoma of either T-cell (CD3+) or B-cell (CD79a+) origin, 5 cases of plas- macytoma, and 4 cases of mast cell tumours. The extended antibody panel revealed 2 cases of alveolar rhabdo- myosarcoma, 2 cases of amelanotic melanoma, and one case of glomus tumour. Conclusions. Both canine cutaneous histiocytoma and cutaneous lymphoma should be considered at the beginning of differential diagnosis for CCRCTs. While most poorly differentiated CCRCTs can be diagnosed immunohis- tochemically using 1–4 basic antibodies, some require a broad antibody panel, including mesenchymal, epithelial, myogenic, and melanocytic markers. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

Non-Wilms Renal Cell Tumors in Children
PEDIATRIC UROLOGIC ONCOLOGY 0094-0143/00 $15.00 + .OO NON-WILMS’ RENAL TUMORS IN CHILDREN Bruce Broecker, MD Renal tumors other than Wilms’ tumor are tastases occur in 40% to 60% of patients with infrequent in childhood. Wilms’ tumors ac- clear cell sarcoma of the kidney, whereas they count for 6% to 7% of childhood cancer, are found in less than 2% of patients with whereas the remaining renal tumors account Wilms’ tumor.**,26 This distinct clinical behav- for less than l%.27The most common non- ior is one of the features that has led to its Wilms‘ tumors are clear cell sarcoma of the designation as a separate tumor. Other clini- kidney, rhabdoid tumor of the kidney (both cal features include a lack of association with formerly considered unfavorable Wilms’ tu- sporadic aniridia or hemihypertrophy. mor variants but now considered separate tu- Clear cell sarcoma of the kidney has not mors), renal cell carcinoma, mesoblastic been reported to occur bilaterally and is not nephroma, and multilocular cystic nephroma. associated with nephroblastomatosis. It has Collectively, these tumors account for less been reported in infancy and adulthood, but than 10% of the primary renal neoplasms in the peak incidence is between 3 and 5 years childhood. of age. It has an aggressive behavior that responds poorly to treatment with vincristine and actinomycin alone, leading to its original CLEAR CELL SARCOMA designation by Beckwith as an unfavorable histology pattern. The addition of doxorubi- Clear cell sarcoma of the kidney is cur- cin in aggressive chemotherapy regimens has rently considered a separate tumor distinct improved outcome. -
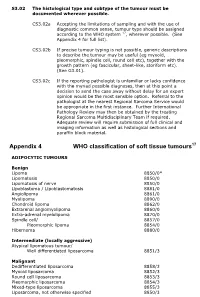
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Misdiagnosed Infantile Rhabdomyofibrosarcoma: a Case Report
2766 ONCOLOGY LETTERS 12: 2766-2768, 2016 Misdiagnosed infantile rhabdomyofibrosarcoma: A case report TAO PAN1*, KEN CHEN1*, RUN-SONG JIANG2 and ZHENG‑YAN ZHAO2 Departments of 1General Surgery and 2Reconstructive Plastic Surgery, The Children's Hospital of Zhejiang University School of Medicine, Hangzhou, Zhejiang 310003, P.R. China Received January 19, 2015; Accepted February 16, 2016 DOI: 10.3892/ol.2016.5032 Abstract. Infantile rhabdomyofibrosarcoma is a rare form of infantile fibrosarcoma has uniform, solidly‑packed spindle cells soft‑tissue tumor often associated with difficulties in diagnosis. arranged in a fascicular or herringbone pattern similar to the The disease is positioned intermediately between rhabdo- vascular pattern observed with hemangiopericytoma (4). Infan- myosarcoma and infantile fibrosarcoma in terms of clinical tile rhabdomyofibrosarcoma may be identified as childhood presentation, immunohistochemistry, behavior, morphology spindle‑cell sarcoma with a low degree of rhabdoid differentiation and ultrastructural features. Reports of rhabdomyofibrosarcoma and aggressive clinical behavior (5). Overlooking the diagnosis cases are limited in the literature. The present case describes a of infantile rhabdomyofibrosarcoma may increase the chances 26‑month‑old female who presented with a slowly progressive, of local recurrence or metastatic disease; therefore, aggressive soft‑tissue mass in the right chest wall. The mass was success- multimodality treatment is required for these patients (6). Reports fully treated with surgery. Using histopathology, the tumor was of rhabdomyofibrosarcoma cases are limited in the literature. diagnosed and classified as infantile rhabdomyofibrosarcoma. The present case report describes a 26‑month‑old patient who The patient has been followed‑up for 2 years and is currently presented with a slowly progressive, soft‑tissue mass in the right in good condition. -

The Identification of a Girl with Tuberous Sclerosis and an Unexpected Large Sized Renal Angiomyolipoma: a Case Report and Literature Review Study
Case Report Annals of Clinical Case Reports Published: 24 Aug, 2020 The Identification of a Girl with Tuberous Sclerosis and an Unexpected Large Sized Renal Angiomyolipoma: A Case Report and Literature Review Study Mitra Naseri1, Farah Ashrafzadeh2, Fatemeh Ghalibafan3* and Paria Dehghanian4 1Department of Pediatric Nephrology, Mashhad University of Medical Sciences, Iran 2Department of Pediatric Neurology, Mashhad University of Medical Sciences, Iran 3Department of Medicine, Mashhad University of Medical Sciences, Iran 4Department of Pathology, Mashhad University of Medical Sciences, Iran Abstract Background: The TSC1 mutated gene, hamartin, and the TSC2 gene, tuberin, cause tuberous sclerosis, the autosomal dominant tumor syndrome. The angiomyolipoma of the kidney is a benign tumor that often happens along with tuberous sclerosis. Large renal angiomyolipoma’s associated with tuberous sclerosis are in danger of fatal hemorrhage. This study reported a case with an unexpected large size of renal angiomyolipoma’s associated with tuberous sclerosis. Case Presentation: We report a girl aged 5 years and 9 months old with tuberous sclerosis who referred to nephrology clinic due to abdominal pain. Physical examination revealed a large mass in the right flank. Kidney ultrasound reported a large mass with approximate size of 90 mm × 60 mm in the right kidney, and abdominal CT scan also showed a non-hemogenic solid mass in the right kidney with size of 91 mm × 68 mm × 67 mm, was highly suspected for Wilms' tumor. Since OPEN ACCESS the large size -

Morphological and Immunohistochemical Characteristics of Surgically Removed Paediatric Renal Tumours in Latvia (1997–2010)
DOI: 10.2478/v10163-012-0008-6 ACTA CHIRURGICA LATVIENSIS • 2011 (11) ORIGINAL ARTICLE Morphological and Immunohistochemical Characteristics of Surgically Removed Paediatric Renal Tumours in Latvia (1997–2010) Ivanda Franckeviča*,**, Regīna Kleina*, Ivars Melderis** *Riga Stradins University, Riga, Latvia **Children’s Clinical University Hospital, Riga, Latvia Summary Introduction. Paediatric renal tumours represent 7% of all childhood malignancies. The variable appearances of the tumours and their rarity make them especially challenging group of lesions for the paediatric pathologist. In Latvia diagnostics and treatment of childhood malignancies is concentrated in Children’s Clinical University Hospital. Microscopic evaluation of them is realised in Pathology office of this hospital. Aim of the study is to analyze morphologic spectrum of children kidney tumours in Latvia and to characterise them from modern positions with wide range of immunohistochemical markers using morphological material of Pathology bureau of Children’s Clinical University Hospital. Materials and methods. We have analyzed surgically removed primary renal tumours in Children Clinical University Hospital from the year 1997 till 2010. Samples were fixed in 10% formalin fluid, imbedded in paraffin and haematoxylin-eosin stained slides were re-examined. Immunohistochemical re-investigation was made in 65.91% of cases. For differential diagnostic purposes were used antibodies for the detection of bcl-2, CD34, EMA, actin, desmin, vimentin, CKAE1/AE3, CK7, Ki67, LCA, WT1, CD99, NSE, chromogranin, synaptophyzin, S100, myoglobin, miogenin, MyoD1 (DakoCytomation) and INI1 protein (Santa Cruz Biotechnology). Results. During the revised period there were diagnosed 44 renal tumours. Accordingly of morphological examination data neoplasms were divided: 1) nephroblastoma – 75%, 2) clear cell sarcoma – 2.27%, 3) rhabdoid tumour – 4.55%, 4) angiomyolipoma – 4.55%, 5) embrional rhabdomyosarcoma – 2.27%, 6) mesoblastic nephroma – 4.55%, 7) multicystic nephroma – 4.55%, 8) angiosarcoma – 2.27%. -
Soft Tissue Sarcoma Classifications
Soft Tissue Sarcoma Classifications Contents: 1. Introduction 2. Summary of SSCRG’s decisions 3. Issue by issue summary of discussions A: List of codes to be included as Soft Tissue Sarcomas B: Full list of codes discussed with decisions C: Sarcomas of neither bone nor soft tissue D: Classifications by other organisations 1. Introduction We live in an age when it is increasingly important to have ‘key facts’ and ‘headline messages’. The national registry for bone and soft tissue sarcoma want to be able to produce high level factsheets for the general public with statements such as ‘There are 2000 soft tissue sarcomas annually in England’ or ‘Survival for soft tissue sarcomas is (eg) 75%’ It is not possible to write factsheets and data briefings like this, without a shared understanding from the SSCRG about which sarcomas we wish to include in our headline statistics. The registry accepts that soft tissue sarcomas are a very complex and heterogeneous group of cancers which do not easily reduce to headline figures. We will still strive to collect all data from cancer registries about anything that is ‘like a sarcoma’. We will also produce focussed data briefings on sites such as dermatofibrosarcomas and Kaposi’s sarcomas – the aim is not to forget any sites we exclude! The majority of soft tissue sarcomas have proved fairly uncontroversial in discussions with individual members of the SSCRG, but there were 7 particular issues it was necessary to make a group decision on. This paper records the decisions made and the rationale behind these decisions. 2. Summary of SSCRG’s decisions: Include all tumours with morphology codes as listed in Appendix A for any cancer site except C40 and C41 (bone).