Diagnostic Immunohistochemistry for Canine Cutaneous Round Cell Tumours — Retrospective Analysis of 60 Cases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primary Mixed Myosarcoma of the Uterine Tube: a Case Report and Review of the Literature ALEXANDER S
Med. J. 258 CASE REPORT: MYOSAIRCOMAMYOSARCOMA OFUTERINEOF UTERINE TUBE Canad.Feb. 3, 1968, Ass.vol. 98 dans 1'cesophage superieur. Le plus petit malade REFERENCES chez qui une biopsie fut prelevee pesait 13 livres 1. CROSBY, W. H.: Amer. or. Dig. Dis., 8: 2, 1963. 2. CAREY, J. B., JR.: Gastroenterology, 46: 550, 1964. et 6tait age de 9 mois. 3. BECK, L T. et al.: Bull. Gastroint. EBndosc., 11: 15, 1965. We wish to thank 0. H. Kimbell, Ph.D., H. Robidoux- 4. MCDONALD, W. G.: Gastroenterology, 51: 390, 1966. 5. PARTIN, J. C. AND SCHUBERT, W. K: New Eng. J. Poirier, R.N., R.-M. Leblanc, R.N., D. Michaud, R.N., Med., 274: 94, 1966. and Marc Gigu6re, R.B.P., for their co-operation and 6. KUITUNEN, P. AND VISAKORPI, J. K.: Lancet, 1: 1276, active assistance. 1965. Primary Mixed Myosarcoma of the Uterine Tube: A Case Report and Review of the Literature ALEXANDER S. ULLMANN, M.D. and MAERIT B. KALLET, M.D., Detroit, Mich., U.S.A. SINCE primary malignant neoplasms of the uterine tube are so rare that no one indi- vidual or clinic has been able to study a large series of patients, the importance of reporting every case has often been emphasized.2-4 Although over 800 cases of primary carcinoma of the tube have been described in the liter- ature,4 up to 1956 only 30 authentic cases of primary sarcoma had been reported and to this number Abrams added another one.1' 8 Recently we had the opportunity to study a patient with primary sarcoma of the fallopian tube. -

Uterine Carcinosarcoma Associated with Pelvic Radiotherapy for Sacral Chordoma: a Case Report
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Available online at www.sciencedirect.com Taiwanese Journal of Obstetrics & Gynecology 51 (2012) 89e92 www.tjog-online.com Case Report Uterine carcinosarcoma associated with pelvic radiotherapy for sacral chordoma: A case report Korhan Kahraman a,*, Fırat Ortac a, Duygu Kankaya b, Gulsah Aynaoglu a a Department of Obstetrics and Gynecology, Ankara University School of Medicine, Ankara, Turkey b Department of Pathology, Ankara University School of Medicine, Ankara, Turkey Accepted 28 December 2010 Abstract Objective: Postirradiation sarcoma of the female genital tract is rare, but a recognized event. Most reported cases have been associated with history of radiotherapy for various gynecologic conditions, particularly cancer of the uterine cervix and abnormal uterine bleeding. The occurrence of uterine sarcoma secondary to radiotherapy for a non-gynecologic tumor and, furthermore, this condition being simultaneous with the recurrence of primary tumor is unique. Case Report: A 67-year-old woman presented with a uterine mass which was diagnosed as a sarcoma by endometrial curettage and history of pelvic radiotherapy 23 years previously for sacral chordoma. Surgical staging procedure for uterine malignancy was performed. The final pathologic diagnosis was carcinosarcoma of the uterus. Conclusion: In uterine masses seen in patients with history of irradiation to the pelvic field, the probability of uterine sarcomas should always be kept in mind. These tumors may occur simultaneously with recurrence of primary tumor previously treated by adjuvant radiation therapy. Copyright Ó 2012, Taiwan Association of Obstetrics & Gynecology. Published by Elsevier Taiwan LLC. -

Misdiagnosed Infantile Rhabdomyofibrosarcoma: a Case Report
2766 ONCOLOGY LETTERS 12: 2766-2768, 2016 Misdiagnosed infantile rhabdomyofibrosarcoma: A case report TAO PAN1*, KEN CHEN1*, RUN-SONG JIANG2 and ZHENG‑YAN ZHAO2 Departments of 1General Surgery and 2Reconstructive Plastic Surgery, The Children's Hospital of Zhejiang University School of Medicine, Hangzhou, Zhejiang 310003, P.R. China Received January 19, 2015; Accepted February 16, 2016 DOI: 10.3892/ol.2016.5032 Abstract. Infantile rhabdomyofibrosarcoma is a rare form of infantile fibrosarcoma has uniform, solidly‑packed spindle cells soft‑tissue tumor often associated with difficulties in diagnosis. arranged in a fascicular or herringbone pattern similar to the The disease is positioned intermediately between rhabdo- vascular pattern observed with hemangiopericytoma (4). Infan- myosarcoma and infantile fibrosarcoma in terms of clinical tile rhabdomyofibrosarcoma may be identified as childhood presentation, immunohistochemistry, behavior, morphology spindle‑cell sarcoma with a low degree of rhabdoid differentiation and ultrastructural features. Reports of rhabdomyofibrosarcoma and aggressive clinical behavior (5). Overlooking the diagnosis cases are limited in the literature. The present case describes a of infantile rhabdomyofibrosarcoma may increase the chances 26‑month‑old female who presented with a slowly progressive, of local recurrence or metastatic disease; therefore, aggressive soft‑tissue mass in the right chest wall. The mass was success- multimodality treatment is required for these patients (6). Reports fully treated with surgery. Using histopathology, the tumor was of rhabdomyofibrosarcoma cases are limited in the literature. diagnosed and classified as infantile rhabdomyofibrosarcoma. The present case report describes a 26‑month‑old patient who The patient has been followed‑up for 2 years and is currently presented with a slowly progressive, soft‑tissue mass in the right in good condition. -

Dermatofibrosarcoma Protuberans and Dermatofibroma: Dermal Dendrocytomas? a Ultrastructural Study
Dermatofibrosarcoma Protuberans and Dermatofibroma: Dermal Dendrocytomas? A Ultrastructural Study Hugo Dominguez-Malagon, M.D., Ana Maria Cano-Valdez, M.D. Department of Pathology, Instituto Nacional de Cancerología, Mexico. ABSTRACT population of plump spindled cells devoid of cell processes, these cells contained intracytoplasmic lipid droplets and rare Dermatofibroma (DF) and Dermatofibrosarcoma subplasmalemmal densities but lacked MVB. Protuberans (DFSP) are dermal tumors whose histogenesis has not been well defined to date. The differential diagnosis in most With the ultrastructural characteristics and the constant cases is established in routine H/E sections and may be confirmed expression of CD34 in DFSP, a probable origin in dermal by immunohistochemistry; however there are atypical variants dendrocytes is postulated. The histogenesis of DF remains of DF with less clear histological differences and non-conclusive obscure. immunohistochemical results. In such cases electron microscopy studies may be useful to establish the diagnosis. INTRODUCTION In the present paper the ultrastructural characteristics of 38 The histogenesis or differentiation of cases of DFSP and 10 cases of DF are described in detail, the Dermatofibrosarcoma Protuberans (DFSP) and objective was to identify some features potentially useful for Dermatofibroma (DF) is controversial in the literature. For differential diagnosis, and to identify the possible histogenesis of DFSP diverse origins such as fibroblastic,1 fibro-histiocytic2 both neoplasms. Schwannian,3 myofibroblastic,4 perineurial,5,6 and endoneurial (7) have been postulated. DFSP in all cases was formed by stellate or spindled cells with long, slender, ramified cell processes joined by primitive junctions, Regarding DF, most authors are in agreement of a subplasmalemmal densities were frequently seen in the processes. -
Soft Tissue Sarcoma Classifications
Soft Tissue Sarcoma Classifications Contents: 1. Introduction 2. Summary of SSCRG’s decisions 3. Issue by issue summary of discussions A: List of codes to be included as Soft Tissue Sarcomas B: Full list of codes discussed with decisions C: Sarcomas of neither bone nor soft tissue D: Classifications by other organisations 1. Introduction We live in an age when it is increasingly important to have ‘key facts’ and ‘headline messages’. The national registry for bone and soft tissue sarcoma want to be able to produce high level factsheets for the general public with statements such as ‘There are 2000 soft tissue sarcomas annually in England’ or ‘Survival for soft tissue sarcomas is (eg) 75%’ It is not possible to write factsheets and data briefings like this, without a shared understanding from the SSCRG about which sarcomas we wish to include in our headline statistics. The registry accepts that soft tissue sarcomas are a very complex and heterogeneous group of cancers which do not easily reduce to headline figures. We will still strive to collect all data from cancer registries about anything that is ‘like a sarcoma’. We will also produce focussed data briefings on sites such as dermatofibrosarcomas and Kaposi’s sarcomas – the aim is not to forget any sites we exclude! The majority of soft tissue sarcomas have proved fairly uncontroversial in discussions with individual members of the SSCRG, but there were 7 particular issues it was necessary to make a group decision on. This paper records the decisions made and the rationale behind these decisions. 2. Summary of SSCRG’s decisions: Include all tumours with morphology codes as listed in Appendix A for any cancer site except C40 and C41 (bone). -

Dermatofibrosarcoma Protuberans of the Parotid Gland -A Case Report
The Korean Journal of Pathology 2004; 38: 276-9 Dermatofibrosarcoma Protuberans of the Parotid Gland -A Case Report - Ok-Jun Lee∙David Y. Pi∙ Dermatofibrosarcoma protuberans (DFSP) typically presents during the early or mid-adult life, Daniel H. Jo∙Kyung-Ja Cho and the most common site of origin is the skin on the trunk and proximal extremities. DFSP of Sang Yoon Kim1∙Jae Y. Ro the parotid gland is extremely rare and only one case has been reported in the literature. We present here a case of a 30-year-old woman with DFSP occurring in the parotid gland, and we Departments of Pathology and discuss the differential diagnosis. The patient is alive and doing well one year after her operation. 1Otolaryngology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea Received : January 27, 2004 Accepted : July 5, 2004 Corresponding Author Jae Y. Ro, M.D. Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, 388-1 Pungnap-dong, Songpa-gu, Seoul 138-736, Korea Tel: 02-3010-4550 Fax: 02-472-7898 E-mail: [email protected] Key Words : Dermatofibrosarcoma Protuberans-Parotid Gland Epithelial tumors make up the majority of salivary gland neo- CASE REPORT plasms, while mesenchymal tumors of this organ are uncommon. Dermatofibrosarcoma protuberans (DFSP) of the salivary gland A 30-year-old woman came to the Otolaryngology Clinic at is exremely rare and only one case has been reported in the parotid the Asan Medical Center with a 2-year history of a slowly enlarg- gland.1 ing mass inferior to the left angle of the mandible. -

Epithelioid Fibrous Histiocytoma
Modern Pathology (2018) 31, 753–762 © 2018 USCAP, Inc All rights reserved 0893-3952/18 $32.00 753 Epithelioid fibrous histiocytoma: molecular characterization of ALK fusion partners in 23 cases Brendan C Dickson1,2,3, David Swanson1,3, George S Charames1,2,3, Christopher DM Fletcher4,5 and Jason L Hornick4,5 1Department of Pathology and Laboratory Medicine, Mount Sinai Hospital, Toronto, ON, Canada; 2Department of Pathobiology and Laboratory Medicine, University of Toronto, Toronto, ON, Canada; 3Lunenfeld-Tanenbaum Research Institute, Mount Sinai Hospital, Toronto, ON, Canada; 4Department of Pathology, Brigham and Women’s Hospital, Boston, MA, USA and 5Harvard Medical School, Boston, MA, USA Epithelioid fibrous histiocytoma is a rare and distinctive cutaneous neoplasm. Most cases harbor ALK rearrangement and show ALK overexpression, which distinguish this neoplasm from conventional cutaneous fibrous histiocytoma and variants. SQSTM1 and VCL have previously been shown to partner with ALK in one case each of epithelioid fibrous histiocytoma. The purpose of this study was to examine a large cohort of epithelioid fibrous histiocytomas by next-generation sequencing to characterize the nature and prevalence of ALK fusion partners. A retrospective archival review was performed to identify cases of epithelioid fibrous histiocytoma (2012–2016). Immunohistochemistry was performed to confirm ALK expression. Targeted next- generation sequencing was applied on RNA extracted from formalin-fixed paraffin-embedded tissue to identify the fusion partners. Twenty-three cases fulfilled inclusion criteria. The mean patient age was 39 years (range, 8– 74), there was no sex predilection, and 475% of cases involved the lower extremities. The most common gene fusions were SQSTM1-ALK (N = 12; 52%) and VCL-ALK (N = 7; 30%); the other four cases harbored novel fusion partners (DCTN1, ETV6, PPFIBP1, and SPECC1L). -

THE AMERICAN JOURNAL of CANCER a Continuation of the Journal of Cancer Research
THE AMERICAN JOURNAL OF CANCER A Continuation of The Journal of Cancer Research ~ VOLUMEXXXIV DECEMBER,1938 NUMBER4 SYNOVIAL SARCOMAS IN SEROUS BURSAE AND TENDON SHEATHS PROF. LOUIS BERGER, M.D. (From the Pathological Department, HBpital de I'Enfant-Jdsus, and the Anti-Cancer Center of Lava1 University, Quebec) Progress in the knowledge of malignant tumors arising from synovial tissue has been slow. In spite of some recent and valuable contributions, this chapter is far from complete. The reasons for this are threefold: first, the want of knowledge concerning the normal features and nature of synovial tissue, which was long studied in articulations only, although it is common, also, to serous bursae and tendon sheaths; second, the relative-perhaps only apparent-rarity of cases; finally, the lack of precision and even vagueness of the reports in the literature., Most of the older authors, and even some contemporary ones, interested primarily in the clinical or surgical aspects of the question, have been satisfied with a purely topographical diagnosis and have either neglected the histologic aspects of their tumors or described them only briefly and superficially. We have had the opportunity of studying five cases of synovial sarcoma, differing more or less from one another but all originating outside of articu- lations, that is in serous bursae or tendon sheaths, where these tumors are less known, but perhaps easier to study than in the more intricate tissues of the joints. THENORMAL SYNOVIAL TISSUE The prototype of synovial tissue is encountered in the synovial membranes of the joints, but all histologists admit that the lining tissue of the serous bursae and tendon sheaths is homologous with articular synovialis. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -
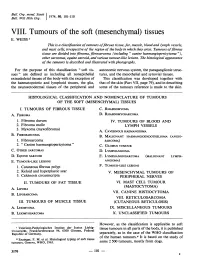
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -
Pathology and Genetics of Tumours of Soft Tissue and Bone
bb5_1.qxd 13.9.2006 14:05 Page 3 World Health Organization Classification of Tumours WHO OMS International Agency for Research on Cancer (IARC) Pathology and Genetics of Tumours of Soft Tissue and Bone Edited by Christopher D.M. Fletcher K. Krishnan Unni Fredrik Mertens IARCPress Lyon, 2002 bb5_1.qxd 13.9.2006 14:05 Page 4 World Health Organization Classification of Tumours Series Editors Paul Kleihues, M.D. Leslie H. Sobin, M.D. Pathology and Genetics of Tumours of Soft Tissue and Bone Editors Christopher D.M. Fletcher, M.D. K. Krishnan Unni, M.D. Fredrik Mertens, M.D. Coordinating Editor Wojciech Biernat, M.D. Layout Lauren A. Hunter Illustrations Lauren A. Hunter Georges Mollon Printed by LIPS 69009 Lyon, France Publisher IARCPress International Agency for Research on Cancer (IARC) 69008 Lyon, France bb5_1.qxd 13.9.2006 14:05 Page 5 This volume was produced in collaboration with the International Academy of Pathology (IAP) The WHO Classification of Tumours of Soft Tissue and Bone presented in this book reflects the views of a Working Group that convened for an Editorial and Consensus Conference in Lyon, France, April 24-28, 2002. Members of the Working Group are indicated in the List of Contributors on page 369. bb5_1.qxd 22.9.2006 9:03 Page 6 Published by IARC Press, International Agency for Research on Cancer, 150 cours Albert Thomas, F-69008 Lyon, France © International Agency for Research on Cancer, 2002, reprinted 2006 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. -

Histiocytic Sarcoma in a 3-Year-Old Male: a Case Report
Histiocytic Sarcoma in a 3-Year-Old Male: A Case Report Samuel Buonocore, MD*; Alfredo L. Valente, MD‡; Daniel Nightingale, MD‡; Jeffrey Bogart, MD§; and Abdul-Kader Souid, MD, PhD* ABSTRACT. We describe a pediatric patient with his- CASE REPORT tiocytic sarcoma involving the T6 and L4 vertebral bodies This previously healthy 3-year-old boy experienced intermit- and the lungs. His tumor progressed during chemother- tent low back pain radiating to the right inguinal region for ϳ2 apy designed for Langerhans’ cell histiocytosis and sar- months. His symptoms initially responded to ibuprofen. The pain coma. High-dose radiation, on the other hand, was intensity increased over a 2-week period, and he refused to walk. effective. Pediatrics 2005;116:e322–e325. URL: www. Review of systems was significant for pain with urination. With the exception of being unable to stand, his physical examination pediatrics.org/cgi/doi/10.1542/peds.2005-0026; sarcoma, was unremarkable. The laboratory tests showed normal blood histiocytes, Langerhans’ cell histiocytosis, histiocytic sar- counts and normal liver and renal function. An MRI showed coma. collapse of the T6 and L4 vertebral bodies and a soft tissue mass in the anterior epidural space at the level of L4 (Fig 1 A and B). The chest and abdominal computed tomography (CT) scans were nor- ABBREVIATIONS. LCH, Langerhans’ cell histiocytosis; CT, com- mal. Bone marrow aspiration revealed no malignant infiltration. A puted tomography; 2CdA, 2-chlorodeoxyadenosine. technetium bone scan showed increased uptake limited to the T6 and L4 regions. CT-scan–guided needle biopsy of the L4 mass revealed infiltrative proliferation of the bone and soft tissue by istiocytic and dendritic neoplasms are rare, sheets and clusters of large ovoid cells with abundant eosinophilic cytoplasm (Fig 2A).