Washington, Dc September 21-24, 2011
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
What Are Soy Isoflavones? Figure 2: Soy Isoflavones Reduced Plasma Isoprostanes Soy Isoflavones Are a Class of Natural Bioactive Compounds in Soybeans
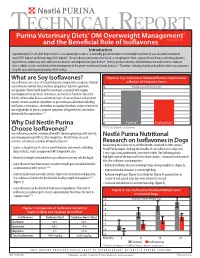
TECHNICAL REPORT Purina Veterinary Diets® OM Overweight Management® brand canine dry formula and the Beneficial Role of Isoflavones Introduction Approximately 35% of adult dogs in the U.S. are overweight or obese1. A markedly greater incidence of overweight and obesity was observed in neutered male (59% higher) and female dogs (40% higher)1. Chronic obesity can increase the risk of, or complications from, several chronic diseases including diabetes, hypertension, pulmonary and cardiovascular disease, and degenerative joint disease2. Obesity produces chronic, mild inflammation and increases oxidative stress, which, in turn, contributes to the development of the above-mentioned chronic diseases.3,4 Therefore, reducing obesity and oxidative stress can promote a long life span and improved quality of life in dogs. What are Soy Isoflavones? Figure 2: Soy Isoflavones Reduced Plasma Isoprostanes Soy isoflavones are a class of natural bioactive compounds in soybeans. Natural a Marker of Oxidative Stress soy isoflavones include three chemical compounds: daidzein, genistein, 5 Plasma Isoprostanes (ng/ml) and glycitein. Many health benefits have been associated with regular consumption of soy products. In humans, soy has been found to reduce the 4 risk of cardiovascular disease and certain types of cancer (breast and prostate cancer); relieve a number of problems in post menopausal women including 3 hot flashes, osteoporosis, and decline in cognitive function; reduce cholesterol and triglycerides in plasma; improve symptoms of hypertension; and reduce 2 abdominal fat accumulation.5,6,7 1 Why Did Nestlé Purina 0 Control Isoflavones* Choose Isoflavones? *P<0.01 for Control vs. Isoflavones Soy isoflavones provide a number of benefits for managing dogs with obesity, and reducing rebound effects after weight loss. -

Applications of in Silico Methods to Analyze the Toxicity and Estrogen T Receptor-Mediated Properties of Plant-Derived Phytochemicals ∗ K
Food and Chemical Toxicology 125 (2019) 361–369 Contents lists available at ScienceDirect Food and Chemical Toxicology journal homepage: www.elsevier.com/locate/foodchemtox Applications of in silico methods to analyze the toxicity and estrogen T receptor-mediated properties of plant-derived phytochemicals ∗ K. Kranthi Kumara, P. Yugandharb, B. Uma Devia, T. Siva Kumara, N. Savithrammab, P. Neerajaa, a Department of Zoology, Sri Venkateswara University, Tirupati, 517502, India b Department of Botany, Sri Venkateswara University, Tirupati, 517502, India ARTICLE INFO ABSTRACT Keywords: A myriad of phytochemicals may have potential to lead toxicity and endocrine disruption effects by interfering Phytochemicals with nuclear hormone receptors. In this examination, the toxicity and estrogen receptor−binding abilities of a QSAR modeling set of 2826 phytochemicals were evaluated. The endpoints mutagenicity, carcinogenicity (both CAESAR and ISS Toxicity models), developmental toxicity, skin sensitization and estrogen receptor relative binding affinity (ER_RBA) Nuclear hormone receptor binding were studied using the VEGA QSAR modeling package. Alongside the predictions, models were providing pos- Self−Organizing maps sible information for applicability domains and most similar compounds as similarity sets from their training Clustering and classification schemes sets. This information was subjected to perform the clustering and classification of chemicals using Self−Organizing Maps. The identified clusters and their respective indicators were considered as potential hotspot structures for the specified data set analysis. Molecular screening interpretations of models wereex- hibited accurate predictions. Moreover, the indication sets were defined significant clusters and cluster in- dicators with probable prediction labels (precision). Accordingly, developed QSAR models showed good pre- dictive abilities and robustness, which observed from applicability domains, representation spaces, clustering and classification schemes. -

Universidade Estadual De Campinas Faculdade De Engenharia De Alimentos Naice Eleidiane Santana Monteiro Evaluation of Probiotics
UNIVERSIDADE ESTADUAL DE CAMPINAS FACULDADE DE ENGENHARIA DE ALIMENTOS NAICE ELEIDIANE SANTANA MONTEIRO EVALUATION OF PROBIOTICS ON INFLUENCE IN THE ABSORPTION AND PRODUCTION OF SOY ISOFLAVONES METABOLITES IN MENOPAUSAL WOMEN WITH CLIMATERIC SYMPTOMATOLOGY AVALIAÇÃO DA INFLUÊNCIA DE PROBIÓTICOS NA ABSORÇÃO E PRODUÇÃO DE METABÓLITOS DE ISOFLAVONAS DA SOJA EM MULHERES MENOPAUSADAS COM SINTOMATOLOGIA CLIMATÉRICA CAMPINAS 2018 NAICE ELEIDIANE SANTANA MONTEIRO EVALUATION OF PROBIOTICS ON INFLUENCE IN THE ABSORPTION AND PRODUCTION OF SOY ISOFLAVONES METABOLITES IN MENOPAUSAL WOMEN WITH CLIMATERIC SYMPTOMATOLOGY AVALIAÇÃO DA INFLUÊNCIA DE PROBIÓTICOS NA ABSORÇÃO E PRODUÇÃO DE METABÓLITOS DE ISOFLAVONAS DA SOJA EM MULHERES MENOPAUSADAS COM SINTOMATOLOGIA CLIMATÉRICA Thesis presented to School of Food Engineering of University of Campinas as part of the requirements for PhD in Food and Nutrition in Experimental Nutrition and Applied to Food Technology area. Tese apresentada à Faculdade de Engenharia de Alimentos da Universidade Estadual de Campinas como parte dos requisitos exigidos para a obtenção do título de Doutora em Alimentos e Nutrição na Área de Nutrição Experimental e aplicada à Tecnologia de Alimentos. ORIENTADOR: GABRIELA ALVES MACEDO COORIENTADOR: ADRIANA ORCESI PEDRO CAMPANA ESTE EXEMPLAR CORRESPONDE A VERSÃO FINAL DA TESE DEFENDIDA PELA ALUNA NAICE ELEIDIANE SANTANA MONTEIRO, E ORIENTADA PELA PROFª. DRª. GABRIELA ALVES MACEDO. CAMPINAS 2018 BANCA EXAMINADORA DA DEFESA DE DOUTORADO NAICE ELEIDIANE SANTANA MONTEIRO MEMBROS: 1. PROF. DR. GABRIELA ALVES MACEDO - PRESIDENTE - (UNIVERSIDADE ESTADUAL DE CAMPINAS) 2. PROF. DR. ANA LUCIA TASCA GOIS RUIZ (UNIVERSIDADE ESTADUAL DE CAMPINAS) 3. PROF. DR. JOELISE DE ALENCAR FIGUEIRA ANGELOTTI (UNIVERSIDADE FEDERAL DE ALFENAS) 4. PROF. DR. LOUISE EMY KUROZAWA (UNIVERSIDADE ESTADUAL DE CAMPINAS) 5. -

Interaction Between the Effects of the Selective Estrogen Modulator Femarelle and a Vitamin D Analog in Human Umbilical Artery V
Journal of Steroid Biochemistry and Molecular Biology xxx (xxxx) xxx–xxx Contents lists available at ScienceDirect Journal of Steroid Biochemistry and Molecular Biology journal homepage: www.elsevier.com/locate/jsbmb Interaction between the effects of the selective estrogen modulator femarelle and a vitamin D analog in human umbilical artery vascular smooth muscle cells ⁎ Dalia Somjen , Esther Knoll, Orli Sharon, Ariel Many, Naftali Stern Institute of Endocrinology, Metabolism and Hypertension, Tel-Aviv Sourasky Medical Center and Sackler Faculty of Medicine, Tel Aviv University, Tel-Aviv, 64239, Israel ARTICLE INFO ABSTRACT Keywords: To further investigate the interaction between vitamin D system and estrogen-mimetic compounds in the human Vascular smooth muscle cells vasculature we studied the effect of the “less- calcemic” analog of 1,25(OH)2D3 (1,25D); JK 1624F2-2 (JKF) in Femarelle the presence of selective estrogen modulator femarelle (F), the phytoestrogen daidzein (D) and estradiol-17b (E2) 1,25D on 3[H] thymidine incorporation (DNA synthesis) and creatine kinase specific activity (CK) in human umbilical JKF artery vascular smooth muscle cells (VSMC). F, D and E , stimulated DNA synthesis at low concentrations, and 1OHase 2 inhibited it at high concentrations. All estrogen-related compounds increased CK dose- dependently. Daily treatment with JKF (1 nM for 3 days) resulted in decreased DNA synthesis, increased CK and up- regulation of the stimulation of DNA synthesis by low estrogen-related hormones whereas D- and E2- mediated inhibition of cell proliferation was abolished by JKF. In contrast, inhibition of cell proliferation by F could not be blocked by JKF. JKF also up-regulated the stimulatory effects on CK by F, E2 and D. -

Daidzein and Genistein Content of Cereals
European Journal of Clinical Nutrition (2002) 56, 961–966 ß 2002 Nature Publishing Group All rights reserved 0954–3007/02 $25.00 www.nature.com/ejcn ORIGINAL COMMUNICATION Daidzein and genistein content of cereals J Liggins1, A Mulligan1,2, S Runswick1 and SA Bingham1,2* 1Medical Research Council Dunn Human Nutrition Unit, Hills Road, Cambridge, UK; and 2European Prospective Investigation of Cancer, University of Cambridge, Cambridge, UK Objective: To analyse 75 cereals and three soy flours commonly eaten in Europe for the phytoestrogens daidzein and genistein. Design: The phytoestrogens daidzein and genistein were extracted from dried foods, and the two isoflavones quantified after hydrolytic removal of any conjugated carbohydrate. Completeness of extraction and any procedural losses of the isoflavones 0 0 were accounted for using synthetic daidzin (7-O-glucosyl-4 -hydroxyisoflavone) and genistin (7-O-glucosyl-4 5-dihydroxyiso- flavone) as internal standards. Setting: Foods from the Cambridge UK area were purchased, prepared for eating, which included cooking if necessary, and freeze dried. Three stock soy flours were also analysed. Results: Eighteen of the foods assayed contained trace or no detectable daidzein or genistein. The soy flours were rich sources, containing 1639 – 2117 mg=kg. The concentration of the two isoflavones in the remaining foods ranged from 33 to 11 873 mg=kg. Conclusion: These analyses will supply useful information to investigators determining the intake of phytoestrogens in cereal products in order to relate intakes to potential biological activities. Sponsorship: This work was supported by the United Kingdom Medical Research Council, Ministry of Agriculture Fisheries and Food (contract FS2034) and the United States of America Army (contract DAMD 17-97-1-7028). -

Mindy Goldman, MD Clinical Professor Dept
Managing Menopause Medically and Naturally Mindy Goldman, MD Clinical Professor Dept. of Ob/Gyn and Reproductive Sciences Director, Women’s Cancer Care Program, UCSF Breast Care Center and Women’s Health University of California, San Francisco I have nothing to disclose –Mindy Goldman, MD CASE STUDY 50 yr. old G2P2 peri-menopausal woman presents with complaints of significant night sweats interfering with her ability to sleep. She has mild hot flashes during the day. She has never had a bone mineral density test but her mother had a hip fracture at age 62 due to osteoporosis. Her 46 yr. old sister was diagnosed with breast cancer at age 43, treated with lumpectomy and radiation and currently is doing well. There is no other family history of cancer. Questions 1. Would you offer her MHT? 2. If yes, how long would you continue it? 3. If no, what would you offer for alternative treatments? 4. Would your treatment differ if you knew she had underlying heart disease? Is it safe? How long can I take it? What about Mymy Bones?bones? Will it protect my heart? MHT - 2015 What about my brain? Will I get breast cancer? What about my hot flashes? Menopausal Symptoms Hot flashes Night sweats Sleep disturbances Vaginal dryness/Sexual dysfunction Mood disturbances How to Treat Menopausal Symptoms Hormone therapy Alternatives to hormones Complementary and Integrative Techniques Prior to Women’s Health Initiative Hormone therapy primary treatment of menopausal hot flashes Few women would continue hormones past one year By 1990’s well known -

Simultaneous Determination of Daidzein, Genistein and Formononetin in Coffee by Capillary Zone Electrophoresis
separations Article Simultaneous Determination of Daidzein, Genistein and Formononetin in Coffee by Capillary Zone Electrophoresis Feng Luan *, Li Li Tang, Xuan Xuan Chen and Hui Tao Liu College of Chemistry and Chemical Engineering, Yantai University, Yantai 264005, China; [email protected] (L.L.T.); [email protected] (X.X.C.); [email protected] (H.T.L.) * Correspondence: fl[email protected]; Tel.: +86-535-6902063 Academic Editor: Doo Soo Chung Received: 29 October 2016; Accepted: 20 December 2016; Published: 1 January 2017 Abstract: Coffee is a favorite and beverage in Western countries that is consumed daily. In the present study, capillary zone electrophoresis (CE) was applied for the separation and quantification of three isoflavones including daidzein, genistein and formononetin in coffee. Extraction of isoflavones from the coffee sample was carried out by extraction and purification process using ether after the acid hydrolysis with the antioxidant butylated hydroxy-toluene (BHT). The experimental conditions of the CE separation method were: 20 mmol/L Na2HPO4 buffer solution, 25 kV applied voltage, 3 s hydrodynamic injection at 30 mbar, and UV detection at 254 nm. The results show that the three compounds can be tested within 10 min with a linearity of 0.5–50 µg/mL for all three compounds. The limits of detection were 0.0642, 0.134, and 0.0825 µg/mL for daidzein, formononetin and genistein, respectively. The corresponding average recovery was 99.39% (Relative Standard Detection (RSD) = 1.76%), 98.71% (RSD = 2.11%) and 97.37% (RSD = 3.74%). Keywords: capillary zone electrophoresis (CE); daidzein; genistein; formononetin; acid hydrolysis 1. -

Contemporary Approaches for Managing Menopause Symptoms
Menopause 2017 Guidelines: Looking at Special Populations and Building on Existing Practice Patricia Geraghty, MSN, FNP-BC, WHNP Disclosures • Speaker Bureau • AbbVie • Therapeutics MD • Advisory Board • AbbVie (endometriosis) • Sharecare Inc. • Procedure Proctor • Bayer (Contraception) • Off label discussion will be included and identified in this discussion. Objectives • Identify the benefits and risks of estrogen, progesterone, and non-hormonal pharmacological management of menopause symptoms based on dosage, route of administration, pharmacokinetics, treatment population and duration of use. • Develop treatment strategies for special populations including premature ovarian insufficiency, prolonged symptoms, and women who are not candidates for estrogen. • Incorporate the NAMS 2017 Position Statement into patient counseling on the timeline of menopause symptoms and the termination of hormone therapy. Lifespan Lifespan Median 34 322 BC Aristotle describes transition Ages the Through Menopause yr JAMA. JAMA. Investigators. Initiative Health the Women's for Group Writing 2002;288(3):321 - 333. doi:10.1001/jama.288.3.321 Treated with plants s/a 1800’s cohosh, cannabis, opium 1821 French physician DeGardanne 53 lifespan lifespan calls it “Menopause” Adult - 1900’s Deficiency disease 55 1942 Premarin” copyright yr 1960’s “Forever Feminine” by Robert Wilson MD 1980’s-1990’s “Politics of Menopause” by Frances McCrea 2002 WHI- First large randomized control trial “My periods are different. Is This Menopause?” • Random cycling, sometimes early, sometimes late. • Flow variable with prodromal spotting, a long taper, or stopping and starting. • She has a day of very heavy flow. • 77% have duration 10+ days, heavy bleeding 3+ days, spotting 6+ days Paramsothy P, et al. BJOG. 2014 Nov;121(12):1564-73. -

Hormonal and Non-Hormonal Management of Vasomotor Symptoms: a Narrated Review
Central Journal of Endocrinology, Diabetes & Obesity Review Article Corresponding authors Orkun Tan, Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology Hormonal and Non-Hormonal and Infertility, University of Texas Southwestern Medical Center, 5323 Harry Hines Blvd. Dallas, TX 75390 and ReproMed Fertility Center, 3800 San Management of Vasomotor Jacinto Dallas, TX 75204, USA, Tel: 214-648-4747; Fax: 214-648-8066; E-mail: [email protected] Submitted: 07 September 2013 Symptoms: A Narrated Review Accepted: 05 October 2013 Orkun Tan1,2*, Anil Pinto2 and Bruce R. Carr1 Published: 07 October 2013 1Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology Copyright and Infertility, University of Texas Southwestern Medical Center, USA © 2013 Tan et al. 2Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology and Infertility, ReproMed Fertility Center, USA OPEN ACCESS Abstract Background: Vasomotor symptoms (VMS; hot flashes, hot flushes) are the most common complaints of peri- and postmenopausal women. Therapies include various estrogens and estrogen-progestogen combinations. However, both physicians and patients became concerned about hormone-related therapies following publication of data by the Women’s Health Initiative (WHI) study and have turned to non-hormonal approaches of varying effectiveness and risks. Objective: Comparison of the efficacy of non-hormonal VMS therapies with estrogen replacement therapy (ERT) or ERT combined with progestogen (Menopausal Hormone Treatment; MHT) and the development of literature-based guidelines for the use of hormonal and non-hormonal VMS therapies. Methods: Pubmed, Cochrane Controlled Clinical Trials Register Database and Scopus were searched for relevant clinical trials that provided data on the treatment of VMS up to June 2013. -

Inhibitory Effect of Genistein and Daidzein on Ovarian Cancer Cell Growth
ANTICANCER RESEARCH 24: 795-800 (2004) Inhibitory Effect of Genistein and Daidzein on Ovarian Cancer Cell Growth CICEK GERCEL-TAYLOR, ANNA K. FEITELSON and DOUGLAS D. TAYLOR Department of Obstetrics, Gynecology and Women’s Health, University of Louisville, School of Medicine, Louisville, KY 40202, U.S.A. Abstract. Background: Survival from ovarian cancer has not Genistein, a soy isoflavanoid, has been intensely studied changed significantly in the past twenty years requiring in relation to breast cancer. Interest first arose upon development of additional treatment protocols. We studied the discovery of the vast difference in breast cancer rates in effect of genistein and daidzein on ovarian cancer cell growth. Asia versus Western countries (1). Large dietary differences Materials and Methods: Five ovarian cancer cell lines from Stage exist, especially in genistein consumption, as the average IIIC disease were evaluated. Sulforhodamine B and colony Asian intake is 20-80 mg/day whereas the average US intake formation assays were used to analyze growth inhibitory effects of is only 1-3 mg (2,3) The dietary and disease discrepancy genistein and daidzein alone and with cisplatin, paclitaxel or prompted further study into the chemopreventive and topotecan. Apoptosis induction was studied by determining potentially therapeutic properties of genistein. caspase-3 activity. Results: Inhibition of growth (50-80%), colony Genistein has been found to inhibit cell proliferation, formation and colony size was seen at 144 Ìm of genistein, 0-23% oncogenesis and clonogenic ability in animal and human reduction was demonstrated at 9 Ìm. At 144 Ìm, the colony size cells (3-5). Several studies have been performed to evaluate was inhibited >75%; at 9 Ìm 4/5 cell lines had >50% reduction. -
Applying SERMS to Advance the Management of Menopause
Applying SERMS to Advance the Management of Menopause Lila Nachtigall, MD NCMP Professor of Ob/Gyn NYU School of Medicine Disclosures I have nothing to disclose SERMs •Selective •Estrogen •Receptor •Modulators The Dynamics of Estrogen & Estrogen Receptors ▪ Estrogen regulates the growth, development, and physiology of the reproductive system ▪ The biological functions of estrogen are mediated by binding to Estrogen Receptors (ER) which our found in most of the female body’s tissues ▪ In each target tissue the ERs have specific characteristics, providing a certain response within the tissue Short & Long-Term Effect of Hormone Depletion Brain & nervous system Skin Heart Breast Reproductive Tract Urinary System • ERs are found in most Bone of the female body’s tissues • Tremendous impact on • Estrogen decline affects short & long term QoL of all tissues women Effect of estrogen depletion in the Brain & Nervous System • Estrogen affects the autonomic control, the emotional state, and higher brain functions; • Reduction in estrogen levels leads to: – Mood swings – Memory loss – Problems focusing – Irritability – Fatigue – Hot flashes & night sweats – Stress & Anxiety – Depression – Decreased libido KNDy Neurons Szeliga A,Gennazzani AD Gynecological Endocrinology, 34:11, 913-919, DOI: 10.1080/09513590.2018.1480711 Szeliga A,Gennazzani AD Gynecological Endocrinology, 34:11, 913-919, DOI: 10.1080/09513590.2018.1480711 The Need Symptoms/Time Line The decline in estrogen levels in women leads to a chronic hormonal imbalance which accompanies women -

Copyright Undertaking
Copyright Undertaking This thesis is protected by copyright, with all rights reserved. By reading and using the thesis, the reader understands and agrees to the following terms: 1. The reader will abide by the rules and legal ordinances governing copyright regarding the use of the thesis. 2. The reader will use the thesis for the purpose of research or private study only and not for distribution or further reproduction or any other purpose. 3. The reader agrees to indemnify and hold the University harmless from and against any loss, damage, cost, liability or expenses arising from copyright infringement or unauthorized usage. IMPORTANT If you have reasons to believe that any materials in this thesis are deemed not suitable to be distributed in this form, or a copyright owner having difficulty with the material being included in our database, please contact [email protected] providing details. The Library will look into your claim and consider taking remedial action upon receipt of the written requests. Pao Yue-kong Library, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong http://www.lib.polyu.edu.hk CHARACTERIZATION OF THE TISSUE-SELECTIVITY OF TRADITIONAL CHINESE MEDICINE (TCM)-DERIVED PHYTOESTROGEN AND THE POSSIBLE MECHANISMS INVOLVED ZHOU LIPING Ph.D The Hong Kong Polytechnic University 2017 The Hong Kong Polytechnic University Department of Applied Biology and Chemical Technology Characterization of the Tissue-selectivity of Traditional Chinese Medicine (TCM)-derived Phytoestrogen and the Possible Mechanisms Involved ZHOU Liping A thesis submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy September 2016 I Certificate Originality I hereby declare that this thesis is my own work and that, to the best of my knowledge and belief, it reproduces no material previously published or written, nor material that has been accepted for the award of any other degree or diploma, except where due acknowledgement has been made in the text.