Maxillofacial Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Natural History of Odontogenic Infection
Natural History of Odontogenic Infection The usual cause of odontogenic infections is necrosis of the pulp of the tooth, which is followed by bacterial invasion through the pulp chamber and into the deeper tissues. Necrosis of the pulp is the result of deep caries in the tooth, to which the pulp responds with a typical inflammatory reaction. Vasodilation and edema cause pressure in the tooth and severe pain as the rigid walls of the tooth prevent swelling. If left untreated the pressure leads to strangulation of the blood supply to the tooth through the apex and consequent necrosis. The necrotic pulp then provides a perfect setting for bacterial invasion into the bone tissue. Once the bacteria have invaded the bone, the infection spreads equally in all directions until a cortical plate is encountered. During the time of intrabony spread, the patient usually experiences sufficient pain to seek treatment. Extraction of the tooth (or removal of the necrotic pulp by an endodontic procedure) results in resolution of the infection. Direction of Spread of Infection The direction of the infection's spread from the tooth apex depends on the thickness of the overlying bone and the relationship of the bone's perforation site to the muscle attachments of the jaws. If no treatment is provided for it, the infection erodes through the thinnest, nearest cortical plate of bone and into the overlying soft tissue. If the root apex is centrally located, the infection erodes through the thinnest bone first. In the maxilla the thinner bone is the labial-buccal side; the palatal cortex is thicker. -

Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone Tissue Engineering
Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone tissue Engineering Elisabet Farré Guasch Dipòsit Legal: B-25086-2011 ISBN: 978-90-5335-394-3 http://hdl.handle.net/10803/31987 ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tesisenxarxa.net) ha estat autoritzada pels titulars dels drets de propietat intel·lectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tesisenred.net) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR. No se autoriza la presentación de su contenido en una ventana o marco ajeno a TDR (framing). -

The Buccal Fat Pad: Importance and Function
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 6 Ver. XIII (June. 2016), PP 79-81 www.iosrjournals.org The Buccal Fat Pad: Importance And Function Ulduz Zamani Ahari1, Hosein Eslami2, Parisa Falsafi*2, Aila Bahramian2, Saleh Maleki1 1. Post Graduate Student Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. 2.Department Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. ●Corresponding Author Email:[email protected] Abstract: The buccal fat is an important anatomic structure intimately related to the masticatory muscles, facial nerve , and parotid duct.while anatomically complex , an understanding of its boundaries will allow the surgeon to safely manipulate this structure in reconstructive and aesthetic procedures . Technically, the buccal fat pad is easily accessed and moblized . It is does not cause any noticeable defect in the cheek or mouth, and it can be performed in a very short time and without causing complication for the patient. The pedicled BFP graft is more resistant to infection than other kinds of free graft and will result in very success. The buccal fat pad has a satisfactory vascular supply , This property of graft and other properties will allow for the closure of defects that cannot be repaired by conventional procedures. The buccal fat pad exposed through an intraoral and buccal incision , has several clinical application including aesthetic improvement , close of oroantral and Oroantral defects reconstruction of surgical defects and palatal cleft defects and palatal cleft defects , reconstruction of maxilla and palatal defects. -
Nbde Part 2 Decks and Remembed-Arroz Con Mango
ARROZ CON MANGO Dear friends, these are remembered/repeated questions (RQs) and answers I COPIED and PASTED from different discussions on Facebook. I feel sorry because I couldn’t organize the file the way I wanted but I hope it helps. Probably you’ll find some wrong answers in this file, but PLEASE … DO NOT CRITICIZE! Find out the right answer, learn it, share it, PASS your test and BE HAPPY J I wish you all the best GOD BLESS YOU! PAITO 1. All of the following are adverse effects of opioids except? diarrhea and somnolence 2. Advantage of osteogenesis distraction is? less relapse, large movements 3. An investigation that is not accurate but consistent is: reliability 4. Remineralized enamel is rough and cavitation? Dark hard and opaque 5. Characteristics of a child with autism - repetitive action, sensitive to light and noise 6. S,z,che sounds : Teeth barely touching – True 7. Something about bio-transformation, more polar and less lipid soluble? - True 8. How much of he population has herpes? 80% - (65-90% worldwide; 80-85% USA) More than 3.7 billion people under the age of 50 – or 67% of the population – are infected with herpes simplex virus type 1 (HSV-1), according to WHO's first global estimates of HSV-1 infection published today in the journal PLOS ONE. 9. Steps of plaque formation: pellicle, biofilm, materia alba, plaque 10. Dose of hydrocortisone taken per year that will indicate have adrenal insufficiency and need supplement dose for surgery - 20 mg 2 weeks for 2 years 11. Rpd clasp breakage due to what? Work hardening 12. -

Student to Student Guides
Harvard School of Dental Medicine Student-to-Student Guide to Clinic: How to Excel in Third Year 2010-2011 Edition Adam Donnell Mindy Gil Brandon Grunes Sharon Jin Aram Kim Michelle Mian Tracy Pogal-Sussman Kim Whippy 1999 – Blaine Langberg & Justine Tompkins 2000 – Blaine Langberg & Justine Tompkins 2001 – Blaine Langberg & Justine Tompkins 2002 – Mark Abel & David Halmos 2003 – Ketan Amin 2004 – Rishita Saraiya & Vanessa Yu 2005 – Prathima Prasanna & Amy Crystal 2006 – Seenu Susarla & Brooke Blicher 2007 – Deepak Gupta & Daniel Cassarella 2008 – Bryan Limmer & Josh Kristiansen 2009 – Byran Limmer & Josh Kristiansen 2010 – Adam Donnell, Tracy Pogal-Sussman, Kim Whippy, Mindy Gil, Sharon Jin, Brandon Grunes, Aram Kim, Michelle Mian 1 2 Foreword Dear Class of 2012, We present the 12th edition of this guide to you to assist your transition from the medical school to the HSDM clinic. You have accomplished an enormous amount thus far, but the transformation to come is beyond expectation. Third year is challenging, but fun; you‘ll look back a year from now with amazement at the material you‘ve learned, the skills you‘ve acquired, and the new language that gradually becomes second nature. To ease this process, we would like to share with you the material in this guide, starting with lessons from our own experience. Course material is the bedrock of third year. Without knowing and fully understanding prevention, disease control, and the basics of dentistry, even the most technically skilled dental student can not provide patients with successful treatment. Be on time to lectures, don‘t be afraid to ask questions, and take some time to review your notes in the evening. -
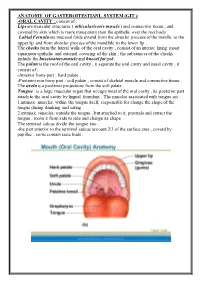
ANATOMY of GASTEROITESTIANL SYSTEM (GIT ): Consist of : ORAL CAVITY
ANATOMY OF GASTEROITESTIANL SYSTEM (GIT ): -ORAL CAVITY : consist of : Lips are muscular structures ( orbicularis oris muscle ) and connective tissue , and covered by skin which is more transparent than the epithelia over the rest body . Labial Fernula are mucosal folds extend from the alveolar process of the maxilla to the upper lip and from alveolar process of the mandible to the lower lip . The cheeks form the lateral walls of the oral cavity , consist of an interior lining moist squamous epithelia and external covering of the skin , the substances of the cheeks include the buccinators muscle and buccal fat pad. The palate is the roof of the oral cavity , it separate the oral cavity and nasal cavity , it consist of : -Anterior bony part : hard palate . -Posterior non bony part : soft palate , consist of skeletal muscle and connective tissue . The uvela is a posterior projections from the soft palate . Tongue : is a large muscular organ that occupy most of the oral cavity , its posterior part attach to the oral cavity by lingual frenulum . The muscles associated with tongue are : 1.intrinsic muscles: within the tongue itself, responsible for change the shape of the tongue during drinking and eating . 2.extrinsic muscles: outside the tongue , but attached to it, protrude and retract the tongue , move it from side to side and change its shape . The terminal sulcus divide the tongue into : -the part anterior to the terminal sulcus account 2/3 of the surface area , coverd by papillae , some contain taste buds . -the posterior one third is devoid of papillae , has few scattered taste buds , it has few small glands and lymphatic tissue (lingual tissue ) Teeth : adults have 32 teeth distributed in two dental arches, the maxillary arch , and the mandibular arch . -

ODONTOGENTIC INFECTIONS Infection Spread Determinants
ODONTOGENTIC INFECTIONS The Host The Organism The Environment In a state of homeostasis, there is Peter A. Vellis, D.D.S. a balance between the three. PROGRESSION OF ODONTOGENIC Infection Spread Determinants INFECTIONS • Location, location , location 1. Source 2. Bone density 3. Muscle attachment 4. Fascial planes “The Path of Least Resistance” Odontogentic Infections Progression of Odontogenic Infections • Common occurrences • Periapical due primarily to caries • Periodontal and periodontal • Soft tissue involvement disease. – Determined by perforation of the cortical bone in relation to the muscle attachments • Odontogentic infections • Cellulitis‐ acute, painful, diffuse borders can extend to potential • fascial spaces. Abscess‐ chronic, localized pain, fluctuant, well circumscribed. INFECTIONS Severity of the Infection Classic signs and symptoms: • Dolor- Pain Complete Tumor- Swelling History Calor- Warmth – Chief Complaint Rubor- Redness – Onset Loss of function – Duration Trismus – Symptoms Difficulty in breathing, swallowing, chewing Severity of the Infection Physical Examination • Vital Signs • How the patient – Temperature‐ feels‐ Malaise systemic involvement >101 F • Previous treatment – Blood Pressure‐ mild • Self treatment elevation • Past Medical – Pulse‐ >100 History – Increased Respiratory • Review of Systems Rate‐ normal 14‐16 – Lymphadenopathy Fascial Planes/Spaces Fascial Planes/Spaces • Potential spaces for • Primary spaces infectious spread – Canine between loose – Buccal connective tissue – Submandibular – Submental -
Bichectomy: Achieving Aesthetic, Funcional and Psychological Results with a Simple Intraoral Surgical Procedure
Volume 1- Issue 2: 2017 DOI: 10.26717/BJSTR.2017.01.000205 Simone De Luccas. Biomed J Sci & Tech Res ISSN: 2574-1241 Opinion Open Access Bichectomy: Achieving Aesthetic, Funcional and Psychological Results with A Simple Intraoral Surgical Procedure Simone De Luccas* Dentist Surgeon, Brazil Received: July 13, 2017; Published: July 19, 2017 *Corresponding author: Simone De Luccas, Dentist Surgeon Rua Antonio Meneghetti, 226 - Sala 4 - Parque Terra Nova II, São Bernardo do Campo - SP, 09820-700, Brazil, Tel: ; Email: Opinion or female, with a round face. The best example is Nefertiti, the Bichectomy, or Bichat fat pad removal, is a surgical procedure Egyptian queen, that is still considered a beauty symbol with her indicated when there is excess volume on the middle third of the face (bellow the cheekbones / zygoma) giving it a chubby or round look. The ideal candidates are men and women who wish to achieve definedAlso and in prominentmy opinion, jaw the line. removal of Bichat fat pads do not a slimmer face appearance in this area, and it is also recommended contribute to ageing or future skin slack around the area. These are for patients with chronic cheek biting. Extra-oral photographs are the result of the normal ageing process, due to the loss of collagen part of the preoperative clinical assessment and will be compared and elastin and the shifting of fat tissues under the skin that are with photographs taken postoperative (immediately after the inevitable with age. This procedure changes the contour of the face with a decrease in bulk, resulting in less weight for the tissues to months), when the facial contour and volume reduction will be support, and, therefore, less sagging. -

Utilization of Pedicled Buccal Fat Pads for Coverage of the Lateral Relaxing Wound: a Review of Literature and a Case Series of 15 Patients
J Clin Exp Dent. 2018;10(5):e502-6. Erosive capacity of beverages on primary enamel Journal section: Oral Surgery doi:10.4317/jced.54797 Publication Types: Case Report http://dx.doi.org/10.4317/jced.54797 Utilization of pedicled buccal fat pads for coverage of the lateral relaxing wound: A review of literature and a case series of 15 patients Muhammad Ruslin, Andi S. Hajrah-Yusuf, Andi Tajrin, Lun-Jou Lo, Tymour Forouzanfar 1 Department of Oral and Maxillofacial Surgery/Oral Pathology, VU University Medical Center, P.O. Box 7057, 1007 MB, Am- sterdam, The Netherlands Correspondence: Department of Oral and Maxillofacial Surgery/Oral Pathology VU University Medical Center P.O. Box 7057, 1007 MB, Amsterdam, The Netherlands De Boelelaan 1117 1081 HV Amsterdam Ruslin M, Hajrah-Yusuf AS, Tajrin A, Lo LJ, Forouzanfar T. Utilization [email protected] of pedicled buccal fat pads for coverage of the lateral relaxing wound: A review of literature and a case series of 15 patients. J Clin Exp Dent. Received: 07/03/2018 2018;10(5):e502-6. Accepted: 11/04/2018 http://www.medicinaoral.com/odo/volumenes/v10i5/jcedv10i5p502.pdf Article Number: 54797 http://www.medicinaoral.com/odo/indice.htm © Medicina Oral S. L. C.I.F. B 96689336 - eISSN: 1989-5488 eMail: [email protected] Indexed in: Pubmed Pubmed Central® (PMC) Scopus DOI® System Abstract Background: The buccal fat pad (BFP) is an encapsulated mass originated from a specific fat tissue in various volume throughout the life of each person and BFP has been used in various surgeries as a source of useful graft material due to its easy accessibility and rich vascularization. -

Buccal Fat Pad As an Intra Oral Reconstruction Method in a Case of Oral Verrucous Carcinoma Dr
Case Report Buccal fat pad as an intra oral reconstruction method in a case of oral verrucous carcinoma Dr. Mohammad Asifur Rahman1* , Dr. Md. Harun - Ur – Rashid2, Dr. Ismat Ara Haider3 ABSTRACT AFFILIATION 1. Dr.Mohammad Asifur Rahman, BDS, MS(OMS), The buccal fat pad is a special type of fat tissue, which is Assistant professor, Department of Oral & Maxillofacial Surgery, Dhaka located anterior to the masseter muscle and deep to the Dental College Hospital, Dhaka. buccinator muscle. It provides gliding motion between 2. Dr. Md. Harun - Ur - Rashid, BDS, MS (OMS), muscles, protects the neurovascular bundles from injuries and Associate professor, Department of Oral & Maxillofacial Surgery, maintains facial convexity. The use of the buccal fat pad is Dhaka Dental College Hospital, Dhaka. promoted for the reconstruction of postsurgical intraoral 3. Dr. Ismat Ara Haider, BDS, DDS, MS (OMS), defects in verrucous carcinoma because of its easy to harvest Professor & Head, Department of Oral & Maxillofacial Surgery, and rich in vascular supply. Here we present a case of 65 years old male with verrucous Dhaka Dental College Hospital, Dhaka. carcinoma of left buccal mucosa and retro molar trigone came Article info. to the Department of Oral & Maxillofacial Surgery, Dhaka Dental College & Hospital, Dhaka, Bangladesh which was th Received: 20 August, 2018 successfully managed by surgical excision of lesion and Accepted: 23rd September, 2018 reconstruction with buccal fat pad. Volume: 8, Issue-2 October, 2018 DOI: https://doi.org/10.3329/updcj.v8i2.40383 KEY WORDS - Buccal fat pad, Verrucous carcinoma, Intra oral reconstruction INTRODUCTION © Authors retain copyright and grant the journal right of first Reconstruction of intraoral postsurgical defect is always publication with the work simultaneously licensed under Creative challenging because of its anatomical complexity and special Commons Attribution License CC - BY 4.0 that allows others to share type of intraoral tissues. -

Complex Odontogenic Infections
Complex Odontogenic Infections Larry ). Peterson CHAPTEROUTLINE FASCIAL SPACE INFECTIONS Maxillary Spaces MANDIBULAR SPACES Secondary Fascial Spaces Cervical Fascial Spaces Management of Fascial Space Infections dontogenic infections are usually mild and easily and causes infection in the adjacent tissue. Whether or treated by antibiotic administration and local sur- not this becomes a vestibular or fascial space abscess is 0 gical treatment. Abscess formation in the bucco- determined primarily by the relationship of the muscle lingual vestibule is managed by simple intraoral incision attachment to the point at which the infection perfo- and drainage (I&D) procedures, occasionally including rates. Most odontogenic infections penetrate the bone dental extraction. (The principles of management of rou- in such a way that they become vestibular abscesses. tine odontogenic infections are discussed in Chapter 15.) On occasion they erode into fascial spaces directly, Some odontogenic infections are very serious and require which causes a fascial space infection (Fig. 16-1). Fascial management by clinicians who have extensive training spaces are fascia-lined areas that can be eroded or dis- and experience. Even after the advent of antibiotics and tended by purulent exudate. These areas are potential improved dental health, serious odontogenic infections spaces that do not exist in healthy people but become still sometimes result in death. These deaths occur when filled during infections. Some contain named neurovas- the infection reaches areas distant from the alveolar cular structures and are known as coinpnrtments; others, process. The purpose of this chapter is to present which are filled with loose areolar connective tissue, are overviews of fascial space infections of the head and neck known as clefts. -

Electrosurgery Implant Risk Factors Xerostomia and Diet Fear Factor
CHAPTER 29 Endodontic Records and Legal Responsibilities e169 of the general liability policy for an “accident” rather than leakage after compaction until a permanent restoration is as a malpractice incident compensable under the profes- cemented.305 Besides an adequate coronal sealing, an adequate sional liability policy. Call the patient periodically to check apical sealer should be well adhered to the canal walls. on healing, recovery, and any follow-up plastic or other The endodontic goal is to prevent bacterial contamination surgeries. of the periradicular tissue by predictably providing ade- quately cleaned, shaped, and filled root canal systems. Any Fear Factor residual bacteria should be entombed in the root canal filling. U.S. Centers for Disease Control and Prevention’s National A bacteria-tight apical seal should be designed to last long Center for Health Statistics report that cost is the overriding term with sealed portals to prevent reentry of microorgan- factor preventing adults from seeking dental care. Fear is the isms, which cause reentry recontamination and lead to end- second reason for delayed dental care. Medicaid recipients odontic failure.84,298 Younger patients are more susceptible to were at five times greater risk for worse dental health than bacterial penetration inside dentin tubules and thus recur- those with private coverage. Adults on Medicaid were twice as ring infections.177 likely to have not visited a dentist in more than 5 years.319 Dental fear may result in patients delaying or avoiding Electrosurgery dental care.199 Frequent cancellations and missed appoint- Electrosurgery can cause problems if mishandled. Damage to ments are characteristically associated with fearful dental the oral cavity caused by improper use of electrosurgical patients.