Student to Student Guides
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Natural History of Odontogenic Infection
Natural History of Odontogenic Infection The usual cause of odontogenic infections is necrosis of the pulp of the tooth, which is followed by bacterial invasion through the pulp chamber and into the deeper tissues. Necrosis of the pulp is the result of deep caries in the tooth, to which the pulp responds with a typical inflammatory reaction. Vasodilation and edema cause pressure in the tooth and severe pain as the rigid walls of the tooth prevent swelling. If left untreated the pressure leads to strangulation of the blood supply to the tooth through the apex and consequent necrosis. The necrotic pulp then provides a perfect setting for bacterial invasion into the bone tissue. Once the bacteria have invaded the bone, the infection spreads equally in all directions until a cortical plate is encountered. During the time of intrabony spread, the patient usually experiences sufficient pain to seek treatment. Extraction of the tooth (or removal of the necrotic pulp by an endodontic procedure) results in resolution of the infection. Direction of Spread of Infection The direction of the infection's spread from the tooth apex depends on the thickness of the overlying bone and the relationship of the bone's perforation site to the muscle attachments of the jaws. If no treatment is provided for it, the infection erodes through the thinnest, nearest cortical plate of bone and into the overlying soft tissue. If the root apex is centrally located, the infection erodes through the thinnest bone first. In the maxilla the thinner bone is the labial-buccal side; the palatal cortex is thicker. -

6 Development of the Teeth: Root and Supporting Structures Nagat M
AVERY Chap.06 27-11-2002 10:09 Pagina 108 108 II Development of the Teeth and Supporting Structures 6 Development of the Teeth: Root and Supporting Structures Nagat M. ElNesr and James K. Avery Chapter Outline Introduction Introduction... 108 Objectives... 108 Root development is initiated through the contributions Root Sheath Development... 109 of the cells originating from the enamel organ, dental Single-Root Formation... 110 papilla, and dental follicle. The cells of the outer enamel Multiple-Root Formation... 111 epithelium contact the inner enamel epithelium at the Root Formation Anomalies... 112 base of the enamel organ, the cervical loop (Figs. 6.1 and Fate of the Epithelial Root Sheath (Hertwig's Sheath)... 113 6.2A). Later, with crown completion, the cells of the cer- Dental Follicle... 114 vical loop continue to grow away from the crown and Development of (Intermediate) Cementum... 116 become root sheath cells (Figs. 6.2B and 6.3). The inner Cellular and Acellular Cementum... 116 root sheath cells cause root formation by inducing the Development of the Periodontal Ligament... 117 adjacent cells of the dental papilla to become odonto- Development of the Alveolar Process... 119 blasts, which in turn will form root dentin. The root Summary... 121 sheath will further dictate whether the tooth will have Self-Evaluation Review... 122 single or multiple roots. The remainder of the cells of the dental papilla will then become the cells of the root pulp.The third compo- nent in root formation, the dental follicle, is the tissue that surrounds the enamel organ, the dental papilla, and the root. -

Specialized Stem Cell Niche Enables Repetitive Renewal of Alligator Teeth
Specialized stem cell niche enables repetitive renewal PNAS PLUS of alligator teeth Ping Wua, Xiaoshan Wua,b, Ting-Xin Jianga, Ruth M. Elseyc, Bradley L. Templed, Stephen J. Diverse, Travis C. Glennd, Kuo Yuanf, Min-Huey Cheng,h, Randall B. Widelitza, and Cheng-Ming Chuonga,h,i,1 aDepartment of Pathology, University of Southern California, Los Angeles, CA 90033; bDepartment of Oral and Maxillofacial Surgery, Xiangya Hospital, Central South University, Hunan 410008, China; cLouisiana Department of Wildlife and Fisheries, Rockefeller Wildlife Refuge, Grand Chenier, LA 70643; dEnvironmental Health Science and eDepartment of Small Animal Medicine and Surgery, University of Georgia, Athens, GA 30602; fDepartment of Dentistry and iResearch Center for Wound Repair and Regeneration, National Cheng Kung University, Tainan City 70101, Taiwan; and gSchool of Dentistry and hResearch Center for Developmental Biology and Regenerative Medicine, National Taiwan University, Taipei 10617, Taiwan Edited by Edward M. De Robertis, Howard Hughes Medical Institute/University of California, Los Angeles, CA, and accepted by the Editorial Board March 28, 2013 (received for review July 31, 2012) Reptiles and fish have robust regenerative powers for tooth renewal. replaced from the dental lamina connected to the lingual side of However, extant mammals can either renew their teeth one time the deciduous tooth (15). Human teeth are only replaced one time; (diphyodont dentition) or not at all (monophyodont dentition). however, a remnant of the dental lamina still exists (16) and may Humans replace their milk teeth with permanent teeth and then become activated later in life to form odontogenic tumors (17). lose their ability for tooth renewal. -
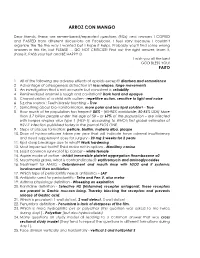
Nbde Part 2 Decks and Remembed-Arroz Con Mango
ARROZ CON MANGO Dear friends, these are remembered/repeated questions (RQs) and answers I COPIED and PASTED from different discussions on Facebook. I feel sorry because I couldn’t organize the file the way I wanted but I hope it helps. Probably you’ll find some wrong answers in this file, but PLEASE … DO NOT CRITICIZE! Find out the right answer, learn it, share it, PASS your test and BE HAPPY J I wish you all the best GOD BLESS YOU! PAITO 1. All of the following are adverse effects of opioids except? diarrhea and somnolence 2. Advantage of osteogenesis distraction is? less relapse, large movements 3. An investigation that is not accurate but consistent is: reliability 4. Remineralized enamel is rough and cavitation? Dark hard and opaque 5. Characteristics of a child with autism - repetitive action, sensitive to light and noise 6. S,z,che sounds : Teeth barely touching – True 7. Something about bio-transformation, more polar and less lipid soluble? - True 8. How much of he population has herpes? 80% - (65-90% worldwide; 80-85% USA) More than 3.7 billion people under the age of 50 – or 67% of the population – are infected with herpes simplex virus type 1 (HSV-1), according to WHO's first global estimates of HSV-1 infection published today in the journal PLOS ONE. 9. Steps of plaque formation: pellicle, biofilm, materia alba, plaque 10. Dose of hydrocortisone taken per year that will indicate have adrenal insufficiency and need supplement dose for surgery - 20 mg 2 weeks for 2 years 11. Rpd clasp breakage due to what? Work hardening 12. -

Fate Map of the Dental Mesenchyme Dynamic Development Of
Developmental Biology 366 (2012) 244–254 Contents lists available at SciVerse ScienceDirect Developmental Biology journal homepage: www.elsevier.com/locate/developmentalbiology Fate map of the dental mesenchyme: Dynamic development of the dental papilla and follicle Michaela Rothova´ a,b,c, Renata Peterkova´ b, Abigail S. Tucker a,n a Department of Craniofacial Development, King’s College London, Floor 27 Guy’s Tower, Guy’s Hospital, London Bridge, SE1 9RT, London, UK b Department of Teratology, Institute of Experimental Medicine, Academy of Sciences of the Czech Republic, Vı´denskaˇ ´ 1083, 14220 Prague, Czech Republic c Department of Cell Biology, Faculty of Science, Charles University, Vinicˇna´ 7, 128 44 Prague, Czech Republic article info abstract Article history: At the bud stage of tooth development the neural crest derived mesenchyme condenses around the Received 31 October 2011 dental epithelium. As the tooth germ develops and proceeds to the cap stage, the epithelial cervical Received in revised form loops grow and appear to wrap around the condensed mesenchyme, enclosing the cells of the forming 1 March 2012 dental papilla. We have fate mapped the dental mesenchyme, using in vitro tissue culture combined Accepted 30 March 2012 with vital cell labelling and tissue grafting, and show that the dental mesenchyme is a much more Available online 20 April 2012 dynamic population then previously suggested. At the bud stage the mesenchymal cells adjacent to the Keywords: tip of the bud form both the dental papilla and dental follicle. At the early cap stage a small population Tooth of highly proliferative mesenchymal cells in close proximity to the inner dental epithelium and primary Mouse enamel knot provide the major contribution to the dental papilla. -

Sinking Our Teeth in Getting Dental Stem Cells to Clinics for Bone Regeneration
International Journal of Molecular Sciences Review Sinking Our Teeth in Getting Dental Stem Cells to Clinics for Bone Regeneration Sarah Hani Shoushrah , Janis Lisa Transfeld , Christian Horst Tonk, Dominik Büchner , Steffen Witzleben , Martin A. Sieber, Margit Schulze and Edda Tobiasch * Department of Natural Sciences, Bonn-Rhein-Sieg University of Applied Sciences, von-Liebig- Strasse. 20, 53359 Rheinbach, Germany; [email protected] (S.H.S.); [email protected] (J.L.T.); [email protected] (C.H.T.); [email protected] (D.B.); [email protected] (S.W.); [email protected] (M.A.S.); [email protected] (M.S.) * Correspondence: [email protected] Abstract: Dental stem cells have been isolated from the medical waste of various dental tissues. They have been characterized by numerous markers, which are evaluated herein and differentiated into multiple cell types. They can also be used to generate cell lines and iPSCs for long-term in vitro research. Methods for utilizing these stem cells including cellular systems such as organoids or cell sheets, cell-free systems such as exosomes, and scaffold-based approaches with and without drug release concepts are reported in this review and presented with new pictures for clarification. These in vitro applications can be deployed in disease modeling and subsequent pharmaceutical research and also pave the way for tissue regeneration. The main focus herein is on the potential of dental stem cells for hard tissue regeneration, especially bone, by evaluating their potential for osteogenesis Citation: Shoushrah, S.H.; Transfeld, and angiogenesis, and the regulation of these two processes by growth factors and environmental J.L.; Tonk, C.H.; Büchner, D.; stimulators. -

Cell Proliferation Study in Human Tooth Germs
Cell proliferation study in human tooth germs Vanesa Pereira-Prado1, Gabriela Vigil-Bastitta2, Estefania Sicco3, Ronell Bologna-Molina4, Gabriel Tapia-Repetto5 DOI: 10.22592/ode2018n32a10 Abstract The aim of this study was to determine the expression of MCM4-5-6 in human tooth germs in the bell stage. Materials and methods: Histological samples were collected from four fetal maxillae placed in paraffin at the block archive of the Histology Department of the School of Dentistry, UdelaR. Sections were made for HE routine technique and for immunohistochemistry technique for MCM4-5-6. Results: Different regions of the enamel organ showed 100% positivity in the intermediate layer, a variation from 100% to 0% in the inner epithelium from the cervical loop to the incisal area, and 0% in the stellar reticulum as well as the outer epithelium. Conclusions: The results show and confirm the proliferative action of the different areas of the enamel organ. Keywords: MCM4, MCM5, MCM6, tooth germ, cell proliferation. 1 Molecular Pathology in Stomatology, School of Dentistry, Universidad de la República, Montevideo, Uruguay. ORCID: 0000-0001- 7747-671 2 Molecular Pathology in Stomatology, School of Dentistry, Universidad de la República, Montevideo, Uruguay. ORCID: 0000-0002- 0617-1279 3 Molecular Pathology in Stomatology, School of Dentistry, Universidad de la República, Montevideo, Uruguay. ORCID: 0000-0003- 1137-6866 4 Molecular Pathology in Stomatology, School of Dentistry, Universidad de la República, Montevideo, Uruguay. ORCID: 0000-0001- 9755-4779 5 Histology Department, School of Dentistry, Universidad de la República, Montevideo, Uruguay. ORCID: 0000-0003-4563-9142 78 Odontoestomatología. Vol. XX - Nº 32 - Diciembre 2018 Introduction that all the DNA is replicated (12), and prevents DNA from replicating more than once in the Tooth organogenesis is a process involving a same cell cycle (13). -

ODONTOGENTIC INFECTIONS Infection Spread Determinants
ODONTOGENTIC INFECTIONS The Host The Organism The Environment In a state of homeostasis, there is Peter A. Vellis, D.D.S. a balance between the three. PROGRESSION OF ODONTOGENIC Infection Spread Determinants INFECTIONS • Location, location , location 1. Source 2. Bone density 3. Muscle attachment 4. Fascial planes “The Path of Least Resistance” Odontogentic Infections Progression of Odontogenic Infections • Common occurrences • Periapical due primarily to caries • Periodontal and periodontal • Soft tissue involvement disease. – Determined by perforation of the cortical bone in relation to the muscle attachments • Odontogentic infections • Cellulitis‐ acute, painful, diffuse borders can extend to potential • fascial spaces. Abscess‐ chronic, localized pain, fluctuant, well circumscribed. INFECTIONS Severity of the Infection Classic signs and symptoms: • Dolor- Pain Complete Tumor- Swelling History Calor- Warmth – Chief Complaint Rubor- Redness – Onset Loss of function – Duration Trismus – Symptoms Difficulty in breathing, swallowing, chewing Severity of the Infection Physical Examination • Vital Signs • How the patient – Temperature‐ feels‐ Malaise systemic involvement >101 F • Previous treatment – Blood Pressure‐ mild • Self treatment elevation • Past Medical – Pulse‐ >100 History – Increased Respiratory • Review of Systems Rate‐ normal 14‐16 – Lymphadenopathy Fascial Planes/Spaces Fascial Planes/Spaces • Potential spaces for • Primary spaces infectious spread – Canine between loose – Buccal connective tissue – Submandibular – Submental -

A Global Compendium of Oral Health
A Global Compendium of Oral Health A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan This book first published 2019 Cambridge Scholars Publishing Lady Stephenson Library, Newcastle upon Tyne, NE6 2PA, UK British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Copyright © 2019 by Morenike Oluwatoyin Folayan and contributors All rights for this book reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner. ISBN (10): 1-5275-3691-2 ISBN (13): 978-1-5275-3691-3 TABLE OF CONTENTS Foreword .................................................................................................. viii Introduction ................................................................................................. 1 Dental Development: Anthropological Perspectives ................................. 31 Temitope A. Esan and Lynne A. Schepartz Belarus ....................................................................................................... 48 Natallia Shakavets, Alexander Yatzuk, Klavdia Gorbacheva and Nadezhda Chernyavskaya Bangladesh ............................................................................................... -

Stem Cells in the Face: Tooth Regeneration and Beyond
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Cell Stem Cell Perspective Stem Cells in the Face: Tooth Regeneration and Beyond Jeremy J. Mao1,* and Darwin J. Prockop2 1Center for Craniofacial Regeneration, Columbia University Medical Center, 630 West 168 Street – PH7E, New York, NY 10032, USA 2Institute for Regenerative Medicine at Scott and White, Texas A&M University Health Science Center, Temple TX 76502, USA *Correspondence: [email protected] http://dx.doi.org/10.1016/j.stem.2012.08.010 The face distinguishes one person from another. Postnatal orofacial tissues harbor rare cells that exhibit stem cell properties. Despite unmet clinical needs for reconstruction of tissues lost in congenital anomalies, infec- tions, trauma, or tumor resection, how orofacial stem/progenitor cells contribute to tissue development, pathogenesis, and regeneration is largely obscure. This perspective article critically analyzes the current status of our understanding of orofacial stem/progenitor cells, identifies gaps in our knowledge, and high- lights pathways for the development of regenerative therapies. Introduction natally from orofacial tissues, have been shown to exhibit stem/ The face consists of vastly diverse tissues, which not only are progenitor cell properties such as self-renewal, clonogenicity, vital for esthetics, but also exert several indispensable func- multilineage differentiation, and the ability to induce tissue tions including breathing, chewing, speech, sight, and smell. formation in vivo. However, how orofacial stem/progenitor cells Orofacial tissues are lost in congenital anomalies, infections, contribute to patterning in prenatal development, pathogen- trauma, or tumor resection. There is a tremendous and unmet esis, or tissue regeneration remains largely a mystery at this clinical need for reconstruction of lost orofacial tissues and time. -

Initiation to Eruption
Head and Neck embryology Tooth Development Review head and neckblk embryology Initiation to eruption Skip Review Initiation Initiation stomodeum Epithelial cells (dental lamina) During 6th week, ectoderm in stomodeum forms horseshoe shaped mass of oral epithelium mesenchyme Basement membrane mesenchyme Initiation of anterior primary teeth Epithelial cells in horseshoe Dental lamina begins begins the sixth to seventh week form dental lamina growing into mesenchyme of development, initiation of additional At site where tooth will be teeth follows and continues for years Dental Lamina – Initiation Supernumerary tooth PREDICT what would happen if an extra tooth was initiated. Mesiodens 1 Bud Stage – eighth week Bud Stage Epithelium (dental Lamina) Dental lamina grows down into mesenchyme at site of tooth. Mesenchyme starts to change composition in response mesenchyme PREDICT what would happen if two tooth buds fused together or one tooth bud split in half. Fusion/Gemination Cap stage – week 9 By week 9, all germ layers of future tooth have formed ElEnamel organ (ename ll)l only) Dental papilla (dentin and pulp) Fusion Gemination Dental sac (cementum, PDL, Alveolar bone) PREDICT how you would know if it was mesenchyme fusion or gemination Cap Stage Successional Dental Lamina Each primary tooth germ has epithelium a successional lamina that becomes a permanent tooth Succedaneous teeth replace a deciduous tooth, nonsuccedaneous do not IDENTIFY nonsuccedaneous teeth mesenchyme PREDICT What occurs if no successional lamina forms? 2 Congenitally -

Observations on Continuously Growing Roots of the Sloth and the K14-Eda
EVOLUTION & DEVELOPMENT 10:2, 187–195 (2008) Observations on continuously growing roots of the sloth and the K14-Eda transgenic mice indicate that epithelial stem cells can give rise to both the ameloblast and root epithelium cell lineage creating distinct tooth patterns Mark Tummersà and Irma Thesleff1 Institute of Biotechnology, Viikki Biocenter, University of Helsinki, Finland ÃAuthor for correspondence (email: [email protected]) 1Current address and address at time of work for both authors: Institute of Biotechnology, P.O. Box 56, FIN-00014 University of Helsinki, Finland. SUMMARY Root development is traditionally associated that it acts as a functional stem cell niche. Similarly we show with the formation of Hertwig’s epithelial root sheath (HERS), that continuously growing roots represented by the sloth molar whose fragments give rise to the epithelial cell rests of and K14-Eda transgenic incisor maintain a cervical loop with a Malassez (ERM). The HERS is formed by depletion of the small core of stellate reticulum cells around the entire core of stellate reticulum cells, the putative stem cells, in the circumference of the tooth and do not form a HERS, and still cervical loop, leaving only a double layer of the basal give rise to ERM. We propose that HERS is not a necessary epithelium with limited growth capacity. The continuously structure to initiate root formation. Moreover, we conclude that growing incisor of the rodent is subdivided into a crown analog crown vs. root formation, i.e. the production of enamel vs. half on the labial side, with a cervical loop containing a large cementum, and the differentiation of the epithelial cells into core of stellate reticulum, and its progeny gives rise to enamel ameloblasts vs.