BUCCAL FAT PAD FLAP Johan Fagan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Parotid and Mandibular Salivary Glands Segmentation of the One Humped Dromedary Camel (Camelus Dromedarius)
Int. J. Adv. Res. Biol. Sci. (2017). 4(11): 32-41 International Journal of Advanced Research in Biological Sciences ISSN: 2348-8069 www.ijarbs.com DOI: 10.22192/ijarbs Coden: IJARQG(USA) Volume 4, Issue 11 - 2017 Research Article DOI: http://dx.doi.org/10.22192/ijarbs.2017.04.11.005 Parotid and Mandibular Salivary Glands Segmentation Of The One Humped Dromedary Camel (Camelus dromedarius) Hamdy M. Rezk and Nora A. Shaker* Department of Anatomy and Embryology, Faculty of Veterinary Medicine, Cairo University, Egypt *Corresponding author: [email protected] Abstract The present study provides detailed anatomical description of the parotid and mandibular salivary glands of the one humped camel with their segmentation based on arterial blood supply and salivary ducts; to facilitate partial removal of the pathologic gland. The shape, position, relations and blood supply of both salivary glands with their ducts were studied on six cadaveric heads. The mandibular and parotid ducts were injected with Urographin® as contrast medium; through inserting the catheter into their openings in the oral cavity; then applying lateral radiography immediately after the injection. The common carotid arteries were injected with red Latex Neoprene and dissected. The parotid gland was irregular rectangular and had five processes while the mandibular gland was irregular triangular with rounded proximal and pointed distal extremity. The parotid duct enters the oral cavity on the cheek opposite the upper 4th molar tooth. The mandibular duct opens in the oral cavity at the sublingual caruncles on the sublingual floor, just about 2cm cranial to frenulum linguae. Both The parotid and the mandibular salivary glands could be divided into four segments. -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone Tissue Engineering
Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone tissue Engineering Elisabet Farré Guasch Dipòsit Legal: B-25086-2011 ISBN: 978-90-5335-394-3 http://hdl.handle.net/10803/31987 ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tesisenxarxa.net) ha estat autoritzada pels titulars dels drets de propietat intel·lectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tesisenred.net) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR. No se autoriza la presentación de su contenido en una ventana o marco ajeno a TDR (framing). -

Salivary Glands
GASTROINTESTINAL SYSTEM [Anatomy and functions of salivary gland] 1 INTRODUCTION Digestive system is made up of gastrointestinal tract (GI tract) or alimentary canal and accessory organs, which help in the process of digestion and absorption. GI tract is a tubular structure extending from the mouth up to anus, with a length of about 30 feet. GI tract is formed by two types of organs: • Primary digestive organs. • Accessory digestive organs 2 Primary Digestive Organs: Primary digestive organs are the organs where actual digestion takes place. Primary digestive organs are: Mouth Pharynx Esophagus Stomach 3 Anatomy and functions of mouth: FUNCTIONAL ANATOMY OF MOUTH: Mouth is otherwise known as oral cavity or buccal cavity. It is formed by cheeks, lips and palate. It encloses the teeth, tongue and salivary glands. Mouth opens anteriorly to the exterior through lips and posteriorly through fauces into the pharynx. Digestive juice present in the mouth is saliva, which is secreted by the salivary glands. 4 ANATOMY OF MOUTH 5 FUNCTIONS OF MOUTH: Primary function of mouth is eating and it has few other important functions also. Functions of mouth include: Ingestion of food materials. Chewing the food and mixing it with saliva. Appreciation of taste of the food. Transfer of food (bolus) to the esophagus by swallowing . Role in speech . Social functions such as smiling and other expressions. 6 SALIVARY GLANDS: The saliva is secreted by three pairs of major (larger) salivary glands and some minor (small) salivary glands. Major glands are: 1. Parotid glands 2. Submaxillary or submandibular glands 3. Sublingual glands. 7 Parotid Glands: Parotid glands are the largest of all salivary glands, situated at the side of the face just below and in front of the ear. -

The Buccal Fat Pad: Importance and Function
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 6 Ver. XIII (June. 2016), PP 79-81 www.iosrjournals.org The Buccal Fat Pad: Importance And Function Ulduz Zamani Ahari1, Hosein Eslami2, Parisa Falsafi*2, Aila Bahramian2, Saleh Maleki1 1. Post Graduate Student Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. 2.Department Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. ●Corresponding Author Email:[email protected] Abstract: The buccal fat is an important anatomic structure intimately related to the masticatory muscles, facial nerve , and parotid duct.while anatomically complex , an understanding of its boundaries will allow the surgeon to safely manipulate this structure in reconstructive and aesthetic procedures . Technically, the buccal fat pad is easily accessed and moblized . It is does not cause any noticeable defect in the cheek or mouth, and it can be performed in a very short time and without causing complication for the patient. The pedicled BFP graft is more resistant to infection than other kinds of free graft and will result in very success. The buccal fat pad has a satisfactory vascular supply , This property of graft and other properties will allow for the closure of defects that cannot be repaired by conventional procedures. The buccal fat pad exposed through an intraoral and buccal incision , has several clinical application including aesthetic improvement , close of oroantral and Oroantral defects reconstruction of surgical defects and palatal cleft defects and palatal cleft defects , reconstruction of maxilla and palatal defects. -
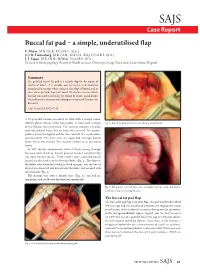
Buccal Fat Pad – a Simple, Underutilised Flap E
SAJS Case Report Buccal fat pad – a simple, underutilised flap E. Meyer, M.B. Ch.B., F.C.O.R.L. (S.A.) S. J. R. Liebenberg, M.B. Ch.B., M.R.C.S. (Ed.), F.C.O.R.L. (S.A.) J. J. Fagan, M.B. Ch.B., M.Med., F.C.O.R.L. (S.A.) Division of Otolaryngology, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital Summary The pedicled buccal fat pad is a reliable flap for the repair of small oral defects. It is durable, easy to harvest, and should be considered in settings where access to free flaps is limited and in cases where previous flaps have failed. We discuss a case in which this flap was used successfully for closure of an oro-antral fistula. The indications, anatomy and techniques of successful harvest are discussed. S Afr J Surg 2012;50(2):47-49. A 57-year-old woman presented in 1998 with a benign minor salivary gland tumour of the hard palate. A wide local excision Fig. 2. Buccal fat pad sutured to cover the oro-antral fistula. of the tumour was performed. The excision margins extended onto the palatal bone, but no bone was excised. The greater palatine artery was ligated and the bone was left to re-epithelialise spontaneously. Two years later, she again had a benign palatal lesion which was excised. The surgery resulted in an oro-antral fistula. In 2007 she was symptomatic, with all fluids coming through her nose when drinking. A local gingival mucosal rotational flap was done without success. -

Distribution and Roles of Substance P in Human Parotid Duct
IJAE Vol. 121, n. 3: 219-225, 2016 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Research article - Histology and cell biology Distribution and roles of substance P in human parotid duct Kaori Amano1,*, Osamu Amano2, George Matsumura3, Kazuyuki Shimada4 1,3Department of Anatomy, Kyorin University School of Medicine; 2Department of Anatomy, Meikai University School of Dentistry; 4Kagoshima University Abstract Sialadenitis occurs with greatest frequency in the parotid glands because infection and inflam- mation arise easily from the oral cavity. Since patients often experience severe swelling and pain during inflammation, the distribution of sensory nerves in these ducts may have clini- cal significance. We used antibodies to the known neuropeptide substance P and to tyrosine hydroxylase - a marker of adrenergic fibres - to observe their distribution and gain insight on their functional role in adult human parotid duct. After excising the parotid duct along with the gland, specimens were divided into three regions: the tract adjacent to the parotid gland, the route along the anterior surface of the masseter, and the area where the duct penetrates the buc- cinator muscle and opens into the oral cavity. Specimens were prepared and examined under a fluorescence microscope following immunostaining. Substance P positivity was observed in all three regions of the duct, whereas tyrosine hydroxylase was distributed mainly in the vas- cular walls and surrounding areas. The distribution of substance P candidates this molecule to assist in tissue defense in conjunction with the blood and lymph vessels of this area. Tyrosine hydroxylase in the blood vessel wall likely contributes to regulation of blood flow in concert with substance P positive nerves surrounding the blood vessels. -
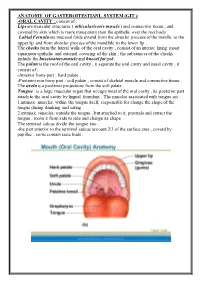
ANATOMY of GASTEROITESTIANL SYSTEM (GIT ): Consist of : ORAL CAVITY
ANATOMY OF GASTEROITESTIANL SYSTEM (GIT ): -ORAL CAVITY : consist of : Lips are muscular structures ( orbicularis oris muscle ) and connective tissue , and covered by skin which is more transparent than the epithelia over the rest body . Labial Fernula are mucosal folds extend from the alveolar process of the maxilla to the upper lip and from alveolar process of the mandible to the lower lip . The cheeks form the lateral walls of the oral cavity , consist of an interior lining moist squamous epithelia and external covering of the skin , the substances of the cheeks include the buccinators muscle and buccal fat pad. The palate is the roof of the oral cavity , it separate the oral cavity and nasal cavity , it consist of : -Anterior bony part : hard palate . -Posterior non bony part : soft palate , consist of skeletal muscle and connective tissue . The uvela is a posterior projections from the soft palate . Tongue : is a large muscular organ that occupy most of the oral cavity , its posterior part attach to the oral cavity by lingual frenulum . The muscles associated with tongue are : 1.intrinsic muscles: within the tongue itself, responsible for change the shape of the tongue during drinking and eating . 2.extrinsic muscles: outside the tongue , but attached to it, protrude and retract the tongue , move it from side to side and change its shape . The terminal sulcus divide the tongue into : -the part anterior to the terminal sulcus account 2/3 of the surface area , coverd by papillae , some contain taste buds . -the posterior one third is devoid of papillae , has few scattered taste buds , it has few small glands and lymphatic tissue (lingual tissue ) Teeth : adults have 32 teeth distributed in two dental arches, the maxillary arch , and the mandibular arch . -

A Guide to Salivary Gland Disorders the Salivary Glands May Be Affected by a Wide Range of Neoplastic and Inflammatory
MedicineToday PEER REVIEWED ARTICLE CPD 1 POINT A guide to salivary gland disorders The salivary glands may be affected by a wide range of neoplastic and inflammatory disorders. This article reviews the common salivary gland disorders encountered in general practice. RON BOVA The salivary glands include the parotid glands, examination are often adequate to recognise and MB BS, MS, FRACS submandibular glands and sublingual glands differentiate many of these conditions. A wide (Figure 1). There are also hundreds of minor sali- array of benign and malignant neoplasms may also Dr Bova is an ENT, Head and vary glands located in the mucosa of the hard and affect the salivary glands and a neoplasia should Neck Surgeon, St Vincent’s soft palate, oral cavity, lips, tongue and oro - always be considered when assessing a salivary Hospital, Sydney, NSW. pharynx. The parotid gland lies in the preauricular gland mass. region and extends inferiorly over the angle of the mandible. The parotid duct courses anteriorly Inflammatory disorders from the parotid gland and enters the mouth Acute sialadenitis through the buccal mucosa adjacent to the second Acute inflammation of the salivary glands is usu- upper molar tooth. The submandibular gland lies ally of viral or bacterial origin. Mumps is the most in the submandibular triangle and its duct passes common causative viral illness, typically affecting anteriorly along the floor of the mouth to enter the parotid glands bilaterally. Children are most adjacent to the frenulum of the tongue. The sub- often affected, with peak incidence occurring at lingual glands are small glands that lie just beneath approximately 4 to 6 years of age. -
Bichectomy: Achieving Aesthetic, Funcional and Psychological Results with a Simple Intraoral Surgical Procedure
Volume 1- Issue 2: 2017 DOI: 10.26717/BJSTR.2017.01.000205 Simone De Luccas. Biomed J Sci & Tech Res ISSN: 2574-1241 Opinion Open Access Bichectomy: Achieving Aesthetic, Funcional and Psychological Results with A Simple Intraoral Surgical Procedure Simone De Luccas* Dentist Surgeon, Brazil Received: July 13, 2017; Published: July 19, 2017 *Corresponding author: Simone De Luccas, Dentist Surgeon Rua Antonio Meneghetti, 226 - Sala 4 - Parque Terra Nova II, São Bernardo do Campo - SP, 09820-700, Brazil, Tel: ; Email: Opinion or female, with a round face. The best example is Nefertiti, the Bichectomy, or Bichat fat pad removal, is a surgical procedure Egyptian queen, that is still considered a beauty symbol with her indicated when there is excess volume on the middle third of the face (bellow the cheekbones / zygoma) giving it a chubby or round look. The ideal candidates are men and women who wish to achieve definedAlso and in prominentmy opinion, jaw the line. removal of Bichat fat pads do not a slimmer face appearance in this area, and it is also recommended contribute to ageing or future skin slack around the area. These are for patients with chronic cheek biting. Extra-oral photographs are the result of the normal ageing process, due to the loss of collagen part of the preoperative clinical assessment and will be compared and elastin and the shifting of fat tissues under the skin that are with photographs taken postoperative (immediately after the inevitable with age. This procedure changes the contour of the face with a decrease in bulk, resulting in less weight for the tissues to months), when the facial contour and volume reduction will be support, and, therefore, less sagging. -

Marsupialisation of Bilateral Ranula in a Buffalo Calf
MOJ Anatomy & Physiology Research Article Open Access Marsupialisation of bilateral ranula in a buffalo calf Abstract Volume 8 Issue 1 - 2021 Diabetes in elderly patients has frequent occurrence of geriatric syndrome. It includes a Kalaiselvan E, Swapan Kumar Maiti, Azam Ranula refers to accumulation of extra-glandular saliva in the floor of the mouth interfering the normal feeding. A male buffalo calf, age of 6 months had bilateral sublingual sialocele Khan, Naveen Kumar Verma, Mohar Singh, (ranula) showing difficulty to masticate and drink water. Bilateral ranula was excised Sharun Khan, Naveen Kumar elliptically to facilitate dynamic fluid/saliva drainage and marsupialisation performed under Division of Surgery, ICAR-Indian Veterinary Research Institute, Izatnagar, Bareilly, Uttar Pradesh, India anesthesia. Animal showed uneventful recovery without any postoperative complications. Correspondence: Swapan Kumar Maiti, Division of Surgery, ICAR-Indian Veterinary Research Institute, Izatnagar, Bareilly, Uttar Pradesh, India, Email Received: January 15, 2021 | Published: Febrauary 15, 2021 Introduction saliva into the mouth (Figure 1–4). The owner was advised to clean the oral cavity with povidone iodine for 7 days. Postoperatively, Ranula or sublingual sialocele refers to a collection of extra- antibiotic, analgesic and fluid therapy was administered for 5 days. glandular and extra-ductal saliva in the floor of the mouth originating On 10thpost-operative day animal showed normal feeding habit and from the sublingual salivary gland. It -

Head and Neck Contouring
Practical Medical Physics: Head and Neck Contouring AAPM 2011 Vancouver, British Columbia Jonn Wu, BMSc MD FRCPC Radiation Oncologist, Vancouver Cancer Centre, BCCA Clinical Assistant Professor, UBC August 2nd, 2011 Objectives Review Selection of Normal Organs • Brachial Plexus • Pharyngeal Constrictors • Salivary Glands • Parotid • Submandibular Target Audience: • Physicists • Dosimetrists • Radiation Therapists Outline Why do we have to Contour? Which Organs are Important? How *I* contour? 3 Important Organ Systems • Xerostomia: Salivary Glands • Parotid • Submandibular • Dysphagia: Pharyngeal Constrictors • Brachial Plexus Outline (cont) For Each Organ System • Anatomy • Literature • Examples Why do we have to contour? • Target delineation • Organ avoidance 2D → 3D → IMRT (your fault) 2D Planning 2D Planning 2.5D… 3DCRT IMRT IMRT & Contours • Inverse Planning • Objective Cost Function • Computers are Binary Why take a contouring course? • IMRT and 3D = standard practice • Both techniques require (accurate) contours • Clinical trials require dose constraints • Consistency (precision) • Who: • Intra- vs inter-contourer • Intra- vs inter-institutional • Why: • Good practice • Dose constraints • Dosimetric repositories Why take a contouring course? • No formal training • Few reproducible guidelines • Everyone assumes consistent contouring • NCIC HN6, RTOG 0920, 0615, 0225 • Spinal Cord: • Intra-observer: avg 0.1 cm, max 0.7 cm • Inter-observer: avg 0.2 cm, max 0.9 cm Geets RO 2005 Which organs are important Brain (temporal lobe) Globe,