Parotid Gland It Is the Largest Salivary Gland (Serous)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Parotid and Mandibular Salivary Glands Segmentation of the One Humped Dromedary Camel (Camelus Dromedarius)
Int. J. Adv. Res. Biol. Sci. (2017). 4(11): 32-41 International Journal of Advanced Research in Biological Sciences ISSN: 2348-8069 www.ijarbs.com DOI: 10.22192/ijarbs Coden: IJARQG(USA) Volume 4, Issue 11 - 2017 Research Article DOI: http://dx.doi.org/10.22192/ijarbs.2017.04.11.005 Parotid and Mandibular Salivary Glands Segmentation Of The One Humped Dromedary Camel (Camelus dromedarius) Hamdy M. Rezk and Nora A. Shaker* Department of Anatomy and Embryology, Faculty of Veterinary Medicine, Cairo University, Egypt *Corresponding author: [email protected] Abstract The present study provides detailed anatomical description of the parotid and mandibular salivary glands of the one humped camel with their segmentation based on arterial blood supply and salivary ducts; to facilitate partial removal of the pathologic gland. The shape, position, relations and blood supply of both salivary glands with their ducts were studied on six cadaveric heads. The mandibular and parotid ducts were injected with Urographin® as contrast medium; through inserting the catheter into their openings in the oral cavity; then applying lateral radiography immediately after the injection. The common carotid arteries were injected with red Latex Neoprene and dissected. The parotid gland was irregular rectangular and had five processes while the mandibular gland was irregular triangular with rounded proximal and pointed distal extremity. The parotid duct enters the oral cavity on the cheek opposite the upper 4th molar tooth. The mandibular duct opens in the oral cavity at the sublingual caruncles on the sublingual floor, just about 2cm cranial to frenulum linguae. Both The parotid and the mandibular salivary glands could be divided into four segments. -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Basic Histology (23 Questions): Oral Histology (16 Questions
Board Question Breakdown (Anatomic Sciences section) The Anatomic Sciences portion of part I of the Dental Board exams consists of 100 test items. They are broken up into the following distribution: Gross Anatomy (50 questions): Head - 28 questions broken down in this fashion: - Oral cavity - 6 questions - Extraoral structures - 12 questions - Osteology - 6 questions - TMJ and muscles of mastication - 4 questions Neck - 5 questions Upper Limb - 3 questions Thoracic cavity - 5 questions Abdominopelvic cavity - 2 questions Neuroanatomy (CNS, ANS +) - 7 questions Basic Histology (23 questions): Ultrastructure (cell organelles) - 4 questions Basic tissues - 4 questions Bone, cartilage & joints - 3 questions Lymphatic & circulatory systems - 3 questions Endocrine system - 2 questions Respiratory system - 1 question Gastrointestinal system - 3 questions Genitouirinary systems - (reproductive & urinary) 2 questions Integument - 1 question Oral Histology (16 questions): Tooth & supporting structures - 9 questions Soft oral tissues (including dentin) - 5 questions Temporomandibular joint - 2 questions Developmental Biology (11 questions): Osteogenesis (bone formation) - 2 questions Tooth development, eruption & movement - 4 questions General embryology - 2 questions 2 National Board Part 1: Review questions for histology/oral histology (Answers follow at the end) 1. Normally most of the circulating white blood cells are a. basophilic leukocytes b. monocytes c. lymphocytes d. eosinophilic leukocytes e. neutrophilic leukocytes 2. Blood platelets are products of a. osteoclasts b. basophils c. red blood cells d. plasma cells e. megakaryocytes 3. Bacteria are frequently ingested by a. neutrophilic leukocytes b. basophilic leukocytes c. mast cells d. small lymphocytes e. fibrocytes 4. It is believed that worn out red cells are normally destroyed in the spleen by a. neutrophils b. -

Salivary Glands
GASTROINTESTINAL SYSTEM [Anatomy and functions of salivary gland] 1 INTRODUCTION Digestive system is made up of gastrointestinal tract (GI tract) or alimentary canal and accessory organs, which help in the process of digestion and absorption. GI tract is a tubular structure extending from the mouth up to anus, with a length of about 30 feet. GI tract is formed by two types of organs: • Primary digestive organs. • Accessory digestive organs 2 Primary Digestive Organs: Primary digestive organs are the organs where actual digestion takes place. Primary digestive organs are: Mouth Pharynx Esophagus Stomach 3 Anatomy and functions of mouth: FUNCTIONAL ANATOMY OF MOUTH: Mouth is otherwise known as oral cavity or buccal cavity. It is formed by cheeks, lips and palate. It encloses the teeth, tongue and salivary glands. Mouth opens anteriorly to the exterior through lips and posteriorly through fauces into the pharynx. Digestive juice present in the mouth is saliva, which is secreted by the salivary glands. 4 ANATOMY OF MOUTH 5 FUNCTIONS OF MOUTH: Primary function of mouth is eating and it has few other important functions also. Functions of mouth include: Ingestion of food materials. Chewing the food and mixing it with saliva. Appreciation of taste of the food. Transfer of food (bolus) to the esophagus by swallowing . Role in speech . Social functions such as smiling and other expressions. 6 SALIVARY GLANDS: The saliva is secreted by three pairs of major (larger) salivary glands and some minor (small) salivary glands. Major glands are: 1. Parotid glands 2. Submaxillary or submandibular glands 3. Sublingual glands. 7 Parotid Glands: Parotid glands are the largest of all salivary glands, situated at the side of the face just below and in front of the ear. -

Salivary Glands; the Parotid Submandibular and Sublingual Functions of Saliva
Lecture series Gastrointestinal tract Professor Shraddha Singh, Department of Physiology, KGMU, Lucknow Various secretions from GIT First secretion from GIT that encounter the food is SALIVARY SECRETIONS What is saliva • Saliva is the mixed glandular secretion which constantly bathes the teeth and the oral mucosa • First secretion encounter the food • It is vital for oral health • It is constituted by the secretions of the three paired major salivary glands; The Parotid Submandibular and Sublingual Functions of saliva 1. Defense: a. Antibacterial b. Antifungal c.Immunological 2. Digestive function: a. Digestive enzymes – ptyalin, lipase b. Formation of bolus c. Taste 3. Protective function: a. Protective coating for hard tissues-teeth b. Protective coating for soft tissues 4. Lubricative function: a.Keeps the oral cavity moist b.Facilitates speech c.Helps in mastication and swallowing 5. Buffering function Salivary glands Structure of Salivary Gland Parotid gland • Parotid is large accounts for 50% secretion of saliva • Situated in front of ear behind the ramus of mandible • Gland drain in to oral cavity opposite to second molar tooth • Secretions are basically serous Submandibular and Sub lingual gland • The submandibular gland is about half the size of the parotid gland • It lies above the mylohyoid in the floor of the mouth. It opens into the floor of the mouth underneath the anterior part of the tongue • The sublingual is the smallest of the paired major salivary glands, being about one fifth the size of the submandibular. • It -
Buccal Fat Pad – a Simple, Underutilised Flap E
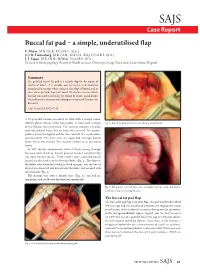
SAJS Case Report Buccal fat pad – a simple, underutilised flap E. Meyer, M.B. Ch.B., F.C.O.R.L. (S.A.) S. J. R. Liebenberg, M.B. Ch.B., M.R.C.S. (Ed.), F.C.O.R.L. (S.A.) J. J. Fagan, M.B. Ch.B., M.Med., F.C.O.R.L. (S.A.) Division of Otolaryngology, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital Summary The pedicled buccal fat pad is a reliable flap for the repair of small oral defects. It is durable, easy to harvest, and should be considered in settings where access to free flaps is limited and in cases where previous flaps have failed. We discuss a case in which this flap was used successfully for closure of an oro-antral fistula. The indications, anatomy and techniques of successful harvest are discussed. S Afr J Surg 2012;50(2):47-49. A 57-year-old woman presented in 1998 with a benign minor salivary gland tumour of the hard palate. A wide local excision Fig. 2. Buccal fat pad sutured to cover the oro-antral fistula. of the tumour was performed. The excision margins extended onto the palatal bone, but no bone was excised. The greater palatine artery was ligated and the bone was left to re-epithelialise spontaneously. Two years later, she again had a benign palatal lesion which was excised. The surgery resulted in an oro-antral fistula. In 2007 she was symptomatic, with all fluids coming through her nose when drinking. A local gingival mucosal rotational flap was done without success. -

Distribution and Roles of Substance P in Human Parotid Duct
IJAE Vol. 121, n. 3: 219-225, 2016 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Research article - Histology and cell biology Distribution and roles of substance P in human parotid duct Kaori Amano1,*, Osamu Amano2, George Matsumura3, Kazuyuki Shimada4 1,3Department of Anatomy, Kyorin University School of Medicine; 2Department of Anatomy, Meikai University School of Dentistry; 4Kagoshima University Abstract Sialadenitis occurs with greatest frequency in the parotid glands because infection and inflam- mation arise easily from the oral cavity. Since patients often experience severe swelling and pain during inflammation, the distribution of sensory nerves in these ducts may have clini- cal significance. We used antibodies to the known neuropeptide substance P and to tyrosine hydroxylase - a marker of adrenergic fibres - to observe their distribution and gain insight on their functional role in adult human parotid duct. After excising the parotid duct along with the gland, specimens were divided into three regions: the tract adjacent to the parotid gland, the route along the anterior surface of the masseter, and the area where the duct penetrates the buc- cinator muscle and opens into the oral cavity. Specimens were prepared and examined under a fluorescence microscope following immunostaining. Substance P positivity was observed in all three regions of the duct, whereas tyrosine hydroxylase was distributed mainly in the vas- cular walls and surrounding areas. The distribution of substance P candidates this molecule to assist in tissue defense in conjunction with the blood and lymph vessels of this area. Tyrosine hydroxylase in the blood vessel wall likely contributes to regulation of blood flow in concert with substance P positive nerves surrounding the blood vessels. -

Oral & Maxillofacial Surgery Removal of Parotid Salivary Gland
Oxford University Hospitals NHS Trust Oral & Maxillofacial Surgery Removal of parotid salivary gland Information for patients This leaflet will help you understand your treatment and should answer many of the questions patients commonly ask before surgery for the removal of a parotid gland. A member of staff will be available if you would like further explanation and to answer any other questions that the leaflet does not cover. What is the parotid gland? The parotid gland lies in front of and below the earlobe. It produces saliva. Saliva drains from the parotid gland through a tube that opens on the inside of the cheek, opposite the upper back teeth. Why do I need my gland removed? The most common reason for removing a parotid gland (or part of the gland) is because a lump has been found inside it. There are also other reasons which your surgeon will discuss with you. What happens before the operation? Pre-assessment clinic – You will be asked to attend an appointment at this clinic. Nursing and/or medical staff will go through some important checks and make certain all relevant investigations have been completed well in advance of the operation date. Admission – You will normally be asked to come to Theatre Direct Admissions or Litchfield Day Surgery Unit on the morning of your operation. The anaesthetist will see you to explain the anaesthetic and answer any questions you may have. They will also be able to advise you about pain relief available after the operation. The surgeon will explain the details of the operation and discuss the possible risks, before asking you to sign a consent form (this may be done at the pre-assessment appointment). -

Wayne County Community College District
Wayne County Community College District COURSE SYLLABUS DHY 111 Histology and Oral Embryology CREDIT HOURS: 3.00 CONTACT HOURS: 45.00 COURSE DESCRIPTION: Basic principles of histology and embryology are reviewed with emphasis on tissues of the oral cavity and contiguous structures. Histology and embryology encompasses the development of the oral facial complex including the formation of the enamel, dentin and pulp, root formation, the attachment apparatus and the eruption and shedding of teeth. PREREQUISITES: DHY 101, DHY 110, DHY 120 EXPECTED COMPETENCIES: Upon completion of this course, the student will be familiar with: • Name the four basic tissues in the body and give an example of where each type is found. • List and give the relative size of various subdivisions of the meter down to the angstrom and give the range of human cell sizes. • Give the function of the following cell parts and organelles. • Relate the structures of the oral cavity with their description or label: • Describe normal gingival including its component parts. • Name the structure that lies under the sublingual fold. • Discuss why dentin formation can continue throughout life but enamel cannot. • List and discuss the types of dentin and cementum. • Describe the functions of cementum. • State the functions of the pulp. • Label the parts of the pulp cavity. • Describe an odontoblast, cementocyte and cemento last. • Name, identify and locate in the body the various types of epithelia both simple and stratified, and pseudostralified. • Name, define and give examples of the various epithelial glands. • Name, describe, compare and locate in the body the various connective tissues. • Name, describe, compare and locate in the body the various types of cartilage. -

A Guide to Salivary Gland Disorders the Salivary Glands May Be Affected by a Wide Range of Neoplastic and Inflammatory
MedicineToday PEER REVIEWED ARTICLE CPD 1 POINT A guide to salivary gland disorders The salivary glands may be affected by a wide range of neoplastic and inflammatory disorders. This article reviews the common salivary gland disorders encountered in general practice. RON BOVA The salivary glands include the parotid glands, examination are often adequate to recognise and MB BS, MS, FRACS submandibular glands and sublingual glands differentiate many of these conditions. A wide (Figure 1). There are also hundreds of minor sali- array of benign and malignant neoplasms may also Dr Bova is an ENT, Head and vary glands located in the mucosa of the hard and affect the salivary glands and a neoplasia should Neck Surgeon, St Vincent’s soft palate, oral cavity, lips, tongue and oro - always be considered when assessing a salivary Hospital, Sydney, NSW. pharynx. The parotid gland lies in the preauricular gland mass. region and extends inferiorly over the angle of the mandible. The parotid duct courses anteriorly Inflammatory disorders from the parotid gland and enters the mouth Acute sialadenitis through the buccal mucosa adjacent to the second Acute inflammation of the salivary glands is usu- upper molar tooth. The submandibular gland lies ally of viral or bacterial origin. Mumps is the most in the submandibular triangle and its duct passes common causative viral illness, typically affecting anteriorly along the floor of the mouth to enter the parotid glands bilaterally. Children are most adjacent to the frenulum of the tongue. The sub- often affected, with peak incidence occurring at lingual glands are small glands that lie just beneath approximately 4 to 6 years of age. -

Marsupialisation of Bilateral Ranula in a Buffalo Calf
MOJ Anatomy & Physiology Research Article Open Access Marsupialisation of bilateral ranula in a buffalo calf Abstract Volume 8 Issue 1 - 2021 Diabetes in elderly patients has frequent occurrence of geriatric syndrome. It includes a Kalaiselvan E, Swapan Kumar Maiti, Azam Ranula refers to accumulation of extra-glandular saliva in the floor of the mouth interfering the normal feeding. A male buffalo calf, age of 6 months had bilateral sublingual sialocele Khan, Naveen Kumar Verma, Mohar Singh, (ranula) showing difficulty to masticate and drink water. Bilateral ranula was excised Sharun Khan, Naveen Kumar elliptically to facilitate dynamic fluid/saliva drainage and marsupialisation performed under Division of Surgery, ICAR-Indian Veterinary Research Institute, Izatnagar, Bareilly, Uttar Pradesh, India anesthesia. Animal showed uneventful recovery without any postoperative complications. Correspondence: Swapan Kumar Maiti, Division of Surgery, ICAR-Indian Veterinary Research Institute, Izatnagar, Bareilly, Uttar Pradesh, India, Email Received: January 15, 2021 | Published: Febrauary 15, 2021 Introduction saliva into the mouth (Figure 1–4). The owner was advised to clean the oral cavity with povidone iodine for 7 days. Postoperatively, Ranula or sublingual sialocele refers to a collection of extra- antibiotic, analgesic and fluid therapy was administered for 5 days. glandular and extra-ductal saliva in the floor of the mouth originating On 10thpost-operative day animal showed normal feeding habit and from the sublingual salivary gland. It -

Head and Neck Contouring
Practical Medical Physics: Head and Neck Contouring AAPM 2011 Vancouver, British Columbia Jonn Wu, BMSc MD FRCPC Radiation Oncologist, Vancouver Cancer Centre, BCCA Clinical Assistant Professor, UBC August 2nd, 2011 Objectives Review Selection of Normal Organs • Brachial Plexus • Pharyngeal Constrictors • Salivary Glands • Parotid • Submandibular Target Audience: • Physicists • Dosimetrists • Radiation Therapists Outline Why do we have to Contour? Which Organs are Important? How *I* contour? 3 Important Organ Systems • Xerostomia: Salivary Glands • Parotid • Submandibular • Dysphagia: Pharyngeal Constrictors • Brachial Plexus Outline (cont) For Each Organ System • Anatomy • Literature • Examples Why do we have to contour? • Target delineation • Organ avoidance 2D → 3D → IMRT (your fault) 2D Planning 2D Planning 2.5D… 3DCRT IMRT IMRT & Contours • Inverse Planning • Objective Cost Function • Computers are Binary Why take a contouring course? • IMRT and 3D = standard practice • Both techniques require (accurate) contours • Clinical trials require dose constraints • Consistency (precision) • Who: • Intra- vs inter-contourer • Intra- vs inter-institutional • Why: • Good practice • Dose constraints • Dosimetric repositories Why take a contouring course? • No formal training • Few reproducible guidelines • Everyone assumes consistent contouring • NCIC HN6, RTOG 0920, 0615, 0225 • Spinal Cord: • Intra-observer: avg 0.1 cm, max 0.7 cm • Inter-observer: avg 0.2 cm, max 0.9 cm Geets RO 2005 Which organs are important Brain (temporal lobe) Globe,