Rybelsus, INN-Semaglutide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
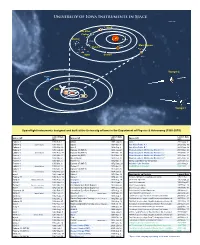
University of Iowa Instruments in Space
University of Iowa Instruments in Space A-D13-089-5 Wind Van Allen Probes Cluster Mercury Earth Venus Mars Express HaloSat MMS Geotail Mars Voyager 2 Neptune Uranus Juno Pluto Jupiter Saturn Voyager 1 Spaceflight instruments designed and built at the University of Iowa in the Department of Physics & Astronomy (1958-2019) Explorer 1 1958 Feb. 1 OGO 4 1967 July 28 Juno * 2011 Aug. 5 Launch Date Launch Date Launch Date Spacecraft Spacecraft Spacecraft Explorer 3 (U1T9)58 Mar. 26 Injun 5 1(U9T68) Aug. 8 (UT) ExpEloxrpelro r1e r 4 1915985 8F eJbu.l y1 26 OEGxOpl o4rer 41 (IMP-5) 19697 Juunlye 2 281 Juno * 2011 Aug. 5 Explorer 2 (launch failure) 1958 Mar. 5 OGO 5 1968 Mar. 4 Van Allen Probe A * 2012 Aug. 30 ExpPloiorenre 3er 1 1915985 8M Oarc. t2. 611 InEjuxnp lo5rer 45 (SSS) 197618 NAouvg.. 186 Van Allen Probe B * 2012 Aug. 30 ExpPloiorenre 4er 2 1915985 8Ju Nlyo 2v.6 8 EUxpKlo 4r e(rA 4ri1el -(4IM) P-5) 197619 DJuenc.e 1 211 Magnetospheric Multiscale Mission / 1 * 2015 Mar. 12 ExpPloiorenre 5e r 3 (launch failure) 1915985 8A uDge.c 2. 46 EPxpiolonreeerr 4130 (IMP- 6) 19721 Maarr.. 313 HMEaRgCnIe CtousbpeShaetr i(cF oMxu-1ltDis scaatelell itMe)i ssion / 2 * 2021081 J5a nM. a1r2. 12 PionPeioenr e1er 4 1915985 9O cMt.a 1r.1 3 EExpxlpolorerer r4 457 ( S(IMSSP)-7) 19721 SNeopvt.. 1263 HMaalogSnaett oCsupbhee Sriact eMlluitlet i*scale Mission / 3 * 2021081 M5a My a2r1. 12 Pioneer 2 1958 Nov. 8 UK 4 (Ariel-4) 1971 Dec. 11 Magnetospheric Multiscale Mission / 4 * 2015 Mar. -
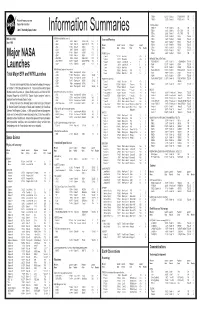
Information Summaries
TIROS 8 12/21/63 Delta-22 TIROS-H (A-53) 17B S National Aeronautics and TIROS 9 1/22/65 Delta-28 TIROS-I (A-54) 17A S Space Administration TIROS Operational 2TIROS 10 7/1/65 Delta-32 OT-1 17B S John F. Kennedy Space Center 2ESSA 1 2/3/66 Delta-36 OT-3 (TOS) 17A S Information Summaries 2 2 ESSA 2 2/28/66 Delta-37 OT-2 (TOS) 17B S 2ESSA 3 10/2/66 2Delta-41 TOS-A 1SLC-2E S PMS 031 (KSC) OSO (Orbiting Solar Observatories) Lunar and Planetary 2ESSA 4 1/26/67 2Delta-45 TOS-B 1SLC-2E S June 1999 OSO 1 3/7/62 Delta-8 OSO-A (S-16) 17A S 2ESSA 5 4/20/67 2Delta-48 TOS-C 1SLC-2E S OSO 2 2/3/65 Delta-29 OSO-B2 (S-17) 17B S Mission Launch Launch Payload Launch 2ESSA 6 11/10/67 2Delta-54 TOS-D 1SLC-2E S OSO 8/25/65 Delta-33 OSO-C 17B U Name Date Vehicle Code Pad Results 2ESSA 7 8/16/68 2Delta-58 TOS-E 1SLC-2E S OSO 3 3/8/67 Delta-46 OSO-E1 17A S 2ESSA 8 12/15/68 2Delta-62 TOS-F 1SLC-2E S OSO 4 10/18/67 Delta-53 OSO-D 17B S PIONEER (Lunar) 2ESSA 9 2/26/69 2Delta-67 TOS-G 17B S OSO 5 1/22/69 Delta-64 OSO-F 17B S Pioneer 1 10/11/58 Thor-Able-1 –– 17A U Major NASA 2 1 OSO 6/PAC 8/9/69 Delta-72 OSO-G/PAC 17A S Pioneer 2 11/8/58 Thor-Able-2 –– 17A U IMPROVED TIROS OPERATIONAL 2 1 OSO 7/TETR 3 9/29/71 Delta-85 OSO-H/TETR-D 17A S Pioneer 3 12/6/58 Juno II AM-11 –– 5 U 3ITOS 1/OSCAR 5 1/23/70 2Delta-76 1TIROS-M/OSCAR 1SLC-2W S 2 OSO 8 6/21/75 Delta-112 OSO-1 17B S Pioneer 4 3/3/59 Juno II AM-14 –– 5 S 3NOAA 1 12/11/70 2Delta-81 ITOS-A 1SLC-2W S Launches Pioneer 11/26/59 Atlas-Able-1 –– 14 U 3ITOS 10/21/71 2Delta-86 ITOS-B 1SLC-2E U OGO (Orbiting Geophysical -

Radial Variation of the Interplanetary Magnetic Field Between 0.3 AU and 1.0 AU
|00000575|| J. Geophys. 42, 591 - 598, 1977 Journal of Geophysics Radial Variation of the Interplanetary Magnetic Field between 0.3 AU and 1.0 AU Observations by the Helios-I Spacecraft G. Musmann, F.M. Neubauer and E. Lammers Institut for Geophysik and Meteorologie, Technische Universitiit Braunschweig, Mendelssohnstr. lA, D-3300 Braunschweig, Federal Republic of Germany Abstract. We have investigated the radial dependence of the radial and azimuthal components and the magnitude of the interplanetary magnetic field obtained by the Technical University of Braunschweig magnetometer experiment on-board of Helios-1 from December 10, 1974 to first perihelion on March 15, 1975. Absolute values of daily averages of each quantity have been employed. The regression analysis based on power laws leads to 2.55 y x r- 2 · 0 , 2.26 y x r- i.o and F = 5.53 y x r- i. 6 with standard deviations of 2.5 y, 2.0 y and 3.2 y for the radial and azimuthal components and magnitude, respectively. Here r is the radial distance from the sun in astronomical units. The results are compared with results obtained for Mariners 4, 5 and 10 and Pioneers 6 and 10. The differences are probably due to different epochs in the solar cycle and the different statistical techniques used. Key words: Interplanetary magnetic field - Helios-1 results. Introduction The study of the vanat10n of the components and magnitude of the in terplanetary magnetic field with heliocentric distance is very intersting at the present time. The mission of Mariner 10 to the inner solar system to a heliocentric distance of 0.46 AU and the missions of Pioneer 10 and Pioneer 11 to the outer solar system to heliocentric distances beyond 5 AU have provided new data over a wide range of heliocentric distance. -

Space and Astrophysical Plasmas: Pervasive Problems
PRAMANA c Indian Academy of Sciences Vol. 55, Nos 5 & 6 — journal of Nov. & Dec. 2000 physics pp. 645–654 Space and astrophysical plasmas: Pervasive problems CHANCHAL UBEROI Department of Mathematics, Indian Institute of Science, Bangalore 560 012, India Abstract. The observations and measurements given by Earth orbiting satellites, deep space probes, sub-orbital systems and orbiting astronomical observatories point out that there are impor- tant physical processes which are responsible for a wide variety of phenomena in solar-terrestrial, solar-system and astrophysical plasmas. In this review these topics are exemplified both from an observational and a theoretical point of view. Keywords. Heliosphere; solar corona; Alfven resonances; magnetic reconnection. PACS Nos 95.30 Q; 96.50 R 1. Introduction Space science is generally defined as investigations that are conducted by scientists using earth orbiting satellites, deep space probes like Pioneer series and sub-orbital systems. Space plasma sciences are now a very highly developed multidisciplinary area of research and can be divided into three areas: solar-terrestrial or Sun–Earth relations, solar-systems exploration and astrophysics. Though space science grew out of the rocket research which followed the end of World War II, the early investigations which began in 1946 concentrated on studies of the Earth’s atmosphere, solar radiation and cosmic rays from space. It was in 1958 that launch of Ex- plorer I and subsequent discovery of Van Allen belts which brought the scientific research in space sciences on to the list of other branches of physical and astrophysical sciences. These earlier flights of Pioneer I and subsequent series which laid the foundation of area of space plasma physics which as we now know has become a highly developed multidis- ciplinary area of research to understand the Sun–Earth or solar-terrestrial relations. -
Geological Survey Research 1961 Synopsis of Geologic and Hydrologic Results
Geological Survey Research 1961 Synopsis of Geologic and Hydrologic Results GEOLOGICAL SURVEY PROFESSIONAL PAPER 424-A Geological Survey Research 1961 THOMAS B. NOLAN, Director GEOLOGICAL SURVEY PROFESSIONAL PAPER 424 A synopsis ofgeologic and hydrologic results, accompanied by short papers in the geologic and hydrologic sciences. Published separately as chapters A, B, C, and D UNITED STATES GOVERNMENT PRINTING OFFICE, WASHINGTON : 1961 FOEEWOED The Geological Survey is engaged in many different kinds of investigations in the fields of geology and hydrology. These investigations may be grouped into several broad, inter related categories as follows: (a) Economic geology, including engineering geology (b) Eegional geologic mapping, including detailed mapping and stratigraphic studies (c) Eesource and topical studies (d) Ground-water studies (e) Surface-water studies (f) Quality-of-water studies (g) Field and laboratory research on geologic and hydrologic processes and principles. The Geological Survey also carries on investigations in its fields of competence for other Fed eral agencies that do not have the required specialized staffs or scientific facilities. Nearly all the Geological Survey's activities yield new data and principles of value in the development or application of the geologic and hydrologic sciences. The purpose of this report, which consists of 4 chapters, is to present as promptly as possible findings that have come to the fore during the fiscal year 1961 the 12 months ending June 30, 1961. The present volume, chapter A, is a synopsis of the highlights of recent findings of scientific and economic interest. Some of these findings have been published or placed on open file during the year; some are presented in chapters B, C, and D ; still others have not been pub lished previously. -
Deep Space Chronicle Deep Space Chronicle: a Chronology of Deep Space and Planetary Probes, 1958–2000 | Asifa
dsc_cover (Converted)-1 8/6/02 10:33 AM Page 1 Deep Space Chronicle Deep Space Chronicle: A Chronology ofDeep Space and Planetary Probes, 1958–2000 |Asif A.Siddiqi National Aeronautics and Space Administration NASA SP-2002-4524 A Chronology of Deep Space and Planetary Probes 1958–2000 Asif A. Siddiqi NASA SP-2002-4524 Monographs in Aerospace History Number 24 dsc_cover (Converted)-1 8/6/02 10:33 AM Page 2 Cover photo: A montage of planetary images taken by Mariner 10, the Mars Global Surveyor Orbiter, Voyager 1, and Voyager 2, all managed by the Jet Propulsion Laboratory in Pasadena, California. Included (from top to bottom) are images of Mercury, Venus, Earth (and Moon), Mars, Jupiter, Saturn, Uranus, and Neptune. The inner planets (Mercury, Venus, Earth and its Moon, and Mars) and the outer planets (Jupiter, Saturn, Uranus, and Neptune) are roughly to scale to each other. NASA SP-2002-4524 Deep Space Chronicle A Chronology of Deep Space and Planetary Probes 1958–2000 ASIF A. SIDDIQI Monographs in Aerospace History Number 24 June 2002 National Aeronautics and Space Administration Office of External Relations NASA History Office Washington, DC 20546-0001 Library of Congress Cataloging-in-Publication Data Siddiqi, Asif A., 1966 Deep space chronicle: a chronology of deep space and planetary probes, 1958-2000 / by Asif A. Siddiqi. p.cm. – (Monographs in aerospace history; no. 24) (NASA SP; 2002-4524) Includes bibliographical references and index. 1. Space flight—History—20th century. I. Title. II. Series. III. NASA SP; 4524 TL 790.S53 2002 629.4’1’0904—dc21 2001044012 Table of Contents Foreword by Roger D. -

NASA and Planetary Exploration
**EU5 Chap 2(263-300) 2/20/03 1:16 PM Page 263 Chapter Two NASA and Planetary Exploration by Amy Paige Snyder Prelude to NASA’s Planetary Exploration Program Four and a half billion years ago, a rotating cloud of gaseous and dusty material on the fringes of the Milky Way galaxy flattened into a disk, forming a star from the inner- most matter. Collisions among dust particles orbiting the newly-formed star, which humans call the Sun, formed kilometer-sized bodies called planetesimals which in turn aggregated to form the present-day planets.1 On the third planet from the Sun, several billions of years of evolution gave rise to a species of living beings equipped with the intel- lectual capacity to speculate about the nature of the heavens above them. Long before the era of interplanetary travel using robotic spacecraft, Greeks observing the night skies with their eyes alone noticed that five objects above failed to move with the other pinpoints of light, and thus named them planets, for “wan- derers.”2 For the next six thousand years, humans living in regions of the Mediterranean and Europe strove to make sense of the physical characteristics of the enigmatic planets.3 Building on the work of the Babylonians, Chaldeans, and Hellenistic Greeks who had developed mathematical methods to predict planetary motion, Claudius Ptolemy of Alexandria put forth a theory in the second century A.D. that the planets moved in small circles, or epicycles, around a larger circle centered on Earth.4 Only partially explaining the planets’ motions, this theory dominated until Nicolaus Copernicus of present-day Poland became dissatisfied with the inadequacies of epicycle theory in the mid-sixteenth century; a more logical explanation of the observed motions, he found, was to consider the Sun the pivot of planetary orbits.5 1. -

Mission Overview the Pioneer Mission Set the Stage for U.S. Space
Mission Overview The Pioneer mission set the stage for U.S. space exploration. Pioneer 1 was the first manmade object to escape the Earth's gravitational field. Later Pioneer 4 was the first spacecraft to fly to the moon, Pioneer 10 was the first to Jupiter, Pioneer 11 was the first to Saturn and Pioneer 12 was the first U.S. spacecraft to orbit another planet, Venus. The following table summarizes the Pioneer spacecraft and scientific objectives of the Pioneer mission. Name Launch Mission Status (as of 1998) ----------------------------------------------------------------- Pioneer 1 1958-10-11 Moon Reached altitude of 72765 miles Pioneer 2 1958-11-08 Moon Reached altitude of 963 miles Pioneer 3 1958-12-02 Moon Reached altitude of 63580 miles Pioneer 4 1959-03-03 Moon Passed by moon into solar orbit Pioneer 5 1960-03-11 Solar Orbit Entered solar orbit Pioneer 6 1965-12-16 Solar Orbit Still operating Pioneer 7 1966-08-17 Solar Orbit Still operating Pioneer 8 1967-12-13 Solar Orbit Still operating Pioneer 9 1967-11-08 Solar Orbit Signal lost in 1983 Pioneer E 1969-08-07 Solar Orbit Launch failure Pioneer10 1972-03-02 Jupiter Communication terminated 1998 Pioneer11 1972-03-02 Jupiter/Saturn Communication terminated 1997 Pioneer12 1978-05-20 Venus Entered Venus atmos. 1992-10-08 The focus of this document is on Pioneer Venus (12), the last spacecraft in a mission of firsts in space exploration. Probe Separation: Pioneer Venus separated into two spacecraft on Aug 8, 1978: an Orbiter (PVO) and a Multiprobe. The latter was separated into five separate vehicles near Venus. -
Pioneer Data-Processing Equipment
https://ntrs.nasa.gov/search.jsp?R=19730009155 2020-03-23T07:26:19+00:00Z 'THE INTERPLANETARY 'PIONEERS VOLUME II: SYSTEM DESIGN AND DEVELOPMENT (NASA-SP-279-Vol-2) THE INTERPLANETARY PIONEERS. VOLUME 2: SYSTEM DESIGN AND DEVELOPMENT (NASA) 312 p MF. $0.95; SOD HC$2.5 N73-1788 CSCL 22C. N"' 73' 111/3 Unclas 62187 m0 I- U~~ NASA SP-279 THE INTERPLANETARY PIONEERS VOLUME II: SYSTEM DESIGN AND DEVELOPMENT by William R. Corliss Scientific and Technical Information Office 1972 NATIONAL AERONAUTICS AND SPACE ADMINISTRATION Washington, D.C. For sale by the Superintendent of Documents, U.S. Government Printing Office, Washington, D.C. 20402 Price $2.50 Stock Number 3300-0452 Library of Congress Catalog Card Number 74-176234 Foreword SOME EXPLORATORY ENTERPRISES start with fanfare and end with a quiet burial; some start with hardly a notice, yet end up significantly ad- vancing mankind's knowledge. The Interplanetary Pioneers more closely fit the latter description. When the National Aeronautics and Space Administration started the program a decade ago it received little public attention. Yet the four spacecraft, designated Pioneers 6, 7, 8, and 9, have faithfully lived up to their name as defined by Webster, "to discover or explore in advance of others." These pioneering spacecraft were the first to systematically orbit the Sun at widely separated points in space, collecting information on conditions far from the Earth's disturbing influence. From them we have learned much about space, the solar wind, and the fluc- tuating bursts of cosmic radiation of both solar and galactic origin. -

Descriptions of Planetary and He1 Iocent R Ic Spacecraft and Investigations
NATIONAL SPACE SCIENCE DATA CENTER WORLD DATA CENTER A for ROCKETS6 AND SATELLITES 88-07 DATA CATALOG SERIES FOR SPACE SCIENCE AND APPLICATIOINS FLIGHT MISSIONS Volume 1A Descriptions of Planetary and He1iocent r ic Spacecraft and Investigations Second Edition March 1988 ~ CATEGORIES PACECRAFT USED FN THIS PLANETARY AND HELIOCENTRIC This category includes probes to the various planets of the solar system and probes designed to make measurements of the characteristics of interplanetary space. Also included are the probes that will pass out of the solar system into interstellar space. NSSDC/WDC-A-R&S 88-07 DATA CATALOG SE:RIES FOR SPACE SCIENCE AND APPLICATIONS FLIGHT MISSIONS Volume 1A DESCRIPTIONS OF P:LANETARY AND HELIOCENTRIC SPACECRAFT AND INVESTIGATIONS Edited By Winifred Sawtell Cameron Robert W. Vostreys Second Edition March 1988 National Space Science Data Center (NSSDC) / World Data Center A for Rc'ckets and Satellites (WDC-A-R&S National Aeronautics and Space Administration Goddard Space Flight Center Greenbelt, Maryland 20771 PREFACE TO THE SECOND EDITION The decision to reprint Volume 1A of the Data Catalog Series for Space Science and Applications Flight Missions was made primarily because it was no longer available when its companion, Volume lB, was completed in April 1987. Although Volume 1A was printed in September 1982, in this second edition no changes were made to the original text, since it described spacecraft and experiments as they actually were durin~qthe acquisition of the data in Volume 1B‘. The only significantarevisionmade in the second edition was the addition of Appendix E, which is an index showing the pages in Volume 1A where one can find descriptions of the spacecraft and experiments corresponding to the data sets described in Volume 1B. -

Aerospace Micro-Lesson
AIAA AEROSPACE M ICRO-LESSON Easily digestible Aerospace Principles revealed for K-12 Students and Educators. These lessons will be sent on a bi-weekly basis and allow grade-level focused learning. - AIAA STEM K-12 Committee. THE MARINER PROJECT Started less than five years after the first launch of rockets into orbit, the Project Mariner was the United States’ first attempt to send a spacecraft to another planet. Between 1962 and 1975, Project Mariner involved the launch of ten unmanned spacecraft, seven of them successfully, to the other inner planets of the Solar System. You can find an overview of the project at NASA’s Science web site. GRADES K-2 Astronomy has always been about looking at things from a distance. For centuries and longer, stars and planets were simply points of light in the sky, most of them stationary and a few of them moving. (In fact, the word “planet” is derived from the Greek word “planetes,” which means “wanderer.”) The invention of the telescope changed the view of planets from wandering points of light to bodies that move around the Sun, but even the best telescopes could not distinguish features smaller than a mile across on the moon and several tens of miles across on even the closest planets. The space program changed this. By sending spacecraft to visit the moon and the planets, scientists were able to view these bodies from comparatively close up and see them in much greater detail. This revolutionized solar system astronomy and gave birth to a new science, “planetary science.” Planetary science joins the fields of astronomy, geology, meteorology, and others together into a unified study of the planets. -

Mondmissionen Von 1958 Bis 2019
WELT DER WISSENSCHAFT: RAUMFAHRT ZUM MOND Mondmissionen von 1958 bis 2019 Im Zeitraum zwischen dem 23. September 1958 und dem 9. August 1976 starteten fast 100 unbemannte und bemannte Raumfahrzeuge zum Mond. Die erste große Phase der Monderkundung endete mit der erfolgreichen Mission der sowjetischen Raumsonde Luna 24, die am 22. August 1976 mit 170 Gramm Mondmaterial aus dem Mare Crisium in Sibirien landete. Danach vergingen mehr als 14 Jahre, bis mit der japanischen Raumsonde Hiten das nächste Raumfahrzeug zum Erdtrabanten entsandt wurde. Von Eugen Reichl und Harro Zimmer 1950er Jahre Pioneer 0: Start am 17. August 1958; sollte am Mond Luna 1: 2. Januar 1959; sollte hart auf dem Mond aufschlagen, vorbeifliegen, Rakete explodierte beim Start. verfehlte den Mond und trat in eine Sonnenumlaufbahn ein. Erste erfolgreiche Raumsonde der Sowjetunion. Luna 1958A: 22. September 1958; sollte hart auf dem Mond aufschlagen, Rakete explodierte beim Start. Pioneer 4: 3. März 1959; Sonde passierte Mond in 60 000 Kilo- meter Abstand und trat in eine Sonnenumlaufbahn ein, erste Pioneer 1: 11. Oktober 1958; sollte am Mond vorbeifliegen, funktionierende Raumsonde der USA. Fehlschlag da Trägerrakete zu schwach, erreichte nur einen Abstand von 114 000 Kilometern zur Erde. Luna 1959A: 16. Juni 1959; sollte hart auf dem Mond aufschlagen, Versagen der Rakete beim Start. Luna 1958B: 11. Oktober 1958; sollte hart auf dem Mond aufschlagen, Rakete explodierte beim Start. Luna 2: 12. September 1959; schlug als erstes Objekt aus Menschenhand hart auf der Mondoberfläche ein, übermittel- Pioneer 2: 8. November 1958; sollte am Mond vorbeifliegen, te dabei keine Messdaten. Versagen der Rakete beim Start.