Product Information Venclexta® (Venetoclax)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Prospective, Multicenter, Phase-II Trial of Ibrutinib Plus Venetoclax In
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 A prospective, multicenter, phase-II trial of ibrutinib plus venetoclax in patients with creatinine clearance ≥ 30 ml/min who have relapsed or refractory chronic lymphocytic leukemia (RR-CLL) with or without TP53 aberrations HOVON 141 CLL / VIsion Trial of the HOVON and Nordic CLL study groups PROTOCOL Principal Investigator : Arnon P Kater (HOVON) Carsten U Niemann (Nordic CLL study Group)) Sponsor : HOVON EudraCT number : 2016-002599-29 ; Page 1 of 107 Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 LOCAL INVESTIGATOR SIGNATURE PAGE Local site name: Signature of Local Investigator Date Printed Name of Local Investigator By my signature, I agree to personally supervise the conduct of this study in my affiliation and to ensure its conduct in compliance with the protocol, informed consent, IRB/EC procedures, the Declaration of Helsinki, ICH Good Clinical Practices guideline, the EU directive Good Clinical Practice (2001-20-EG), and local regulations governing the conduct of clinical studies. -

The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia
International Journal of Molecular Sciences Review The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia Marta Weronika Lato 1 , Anna Przysucha 1, Sylwia Grosman 1, Joanna Zawitkowska 2 and Monika Lejman 3,* 1 Student Scientific Society, Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] (M.W.L.); [email protected] (A.P.); [email protected] (S.G.) 2 Department of Pediatric Hematology, Oncology and Transplantology, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 3 Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland * Correspondence: [email protected] Abstract: Childhood acute lymphoblastic leukemia is a genetically heterogeneous cancer that ac- counts for 10–15% of T-cell acute lymphoblastic leukemia (T-ALL) cases. The T-ALL event-free survival rate (EFS) is 85%. The evaluation of structural and numerical chromosomal changes is important for a comprehensive biological characterization of T-ALL, but there are currently no ge- netic prognostic markers. Despite chemotherapy regimens, steroids, and allogeneic transplantation, relapse is the main problem in children with T-ALL. Due to the development of high-throughput molecular methods, the ability to define subgroups of T-ALL has significantly improved in the last few years. The profiling of the gene expression of T-ALL has led to the identification of T-ALL subgroups, and it is important in determining prognostic factors and choosing an appropriate treatment. Novel therapies targeting molecular aberrations offer promise in achieving better first remission with the Citation: Lato, M.W.; Przysucha, A.; hope of preventing relapse. -
Draft Matrix Post Referral PDF 189 KB
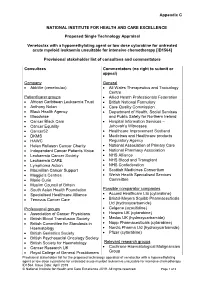
Appendix C NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Proposed Single Technology Appraisal Venetoclax with a hypomethylating agent or low dose cytarabine for untreated acute myeloid leukaemia unsuitable for intensive chemotherapy [ID1564] Provisional stakeholder list of consultees and commentators Consultees Commentators (no right to submit or appeal) Company General • AbbVie (venetoclax) • All Wales Therapeutics and Toxicology Centre Patient/carer groups • Allied Health Professionals Federation • African Caribbean Leukaemia Trust • British National Formulary • Anthony Nolan • Care Quality Commission • Black Health Agency • Department of Health, Social Services • Bloodwise and Public Safety for Northern Ireland • Cancer Black Care • Hospital Information Services – • Cancer Equality Jehovah’s Witnesses • Cancer52 • Healthcare Improvement Scotland • DKMS • Medicines and Healthcare products • HAWC Regulatory Agency • Helen Rollason Cancer Charity • National Association of Primary Care • Independent Cancer Patients Voice • National Pharmacy Association • Leukaemia Cancer Society • NHS Alliance • Leukaemia CARE • NHS Blood and Transplant • Lymphoma Action • NHS Confederation • Macmillan Cancer Support • Scottish Medicines Consortium • Maggie’s Centres • Welsh Health Specialised Services • Marie Curie Committee • Muslim Council of Britain • South Asian Health Foundation Possible comparator companies • Specialised Healthcare Alliance • Accord Healthcare Ltd (cytarabine) • Tenovus Cancer Care • Bristol-Meyers Squibb Pharmaceuticals Ltd -

A Novel CDK9 Inhibitor Increases the Efficacy of Venetoclax (ABT-199) in Multiple Models of Hematologic Malignancies
Leukemia (2020) 34:1646–1657 https://doi.org/10.1038/s41375-019-0652-0 ARTICLE Molecular targets for therapy A novel CDK9 inhibitor increases the efficacy of venetoclax (ABT-199) in multiple models of hematologic malignancies 1 1 2,3 4 1 5 6 Darren C. Phillips ● Sha Jin ● Gareth P. Gregory ● Qi Zhang ● John Xue ● Xiaoxian Zhao ● Jun Chen ● 1 1 1 1 1 1 Yunsong Tong ● Haichao Zhang ● Morey Smith ● Stephen K. Tahir ● Rick F. Clark ● Thomas D. Penning ● 2,7 3 5 1 4 2,7 Jennifer R. Devlin ● Jake Shortt ● Eric D. Hsi ● Daniel H. Albert ● Marina Konopleva ● Ricky W. Johnstone ● 8 1 Joel D. Leverson ● Andrew J. Souers Received: 27 November 2018 / Revised: 18 October 2019 / Accepted: 13 November 2019 / Published online: 11 December 2019 © The Author(s) 2019 Abstract MCL-1 is one of the most frequently amplified genes in cancer, facilitating tumor initiation and maintenance and enabling resistance to anti-tumorigenic agents including the BCL-2 selective inhibitor venetoclax. The expression of MCL-1 is maintained via P-TEFb-mediated transcription, where the kinase CDK9 is a critical component. Consequently, we developed a series of potent small-molecule inhibitors of CDK9, exemplified by the orally active A-1592668, with CDK selectivity profiles 1234567890();,: 1234567890();,: that are distinct from related molecules that have been extensively studied clinically. Short-term treatment with A-1592668 rapidly downregulates RNA pol-II (Ser 2) phosphorylation resulting in the loss of MCL-1 protein and apoptosis in MCL-1- dependent hematologic tumor cell lines. This cell death could be attenuated by either inhibiting caspases or overexpressing BCL-2 protein. -

Phenotype-Based Drug Screening Reveals Association Between Venetoclax Response and Differentiation Stage in Acute Myeloid Leukemia
Acute Myeloid Leukemia SUPPLEMENTARY APPENDIX Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia Heikki Kuusanmäki, 1,2 Aino-Maija Leppä, 1 Petri Pölönen, 3 Mika Kontro, 2 Olli Dufva, 2 Debashish Deb, 1 Bhagwan Yadav, 2 Oscar Brück, 2 Ashwini Kumar, 1 Hele Everaus, 4 Bjørn T. Gjertsen, 5 Merja Heinäniemi, 3 Kimmo Porkka, 2 Satu Mustjoki 2,6 and Caroline A. Heckman 1 1Institute for Molecular Medicine Finland, Helsinki Institute of Life Science, University of Helsinki, Helsinki; 2Hematology Research Unit, Helsinki University Hospital Comprehensive Cancer Center, Helsinki; 3Institute of Biomedicine, School of Medicine, University of Eastern Finland, Kuopio, Finland; 4Department of Hematology and Oncology, University of Tartu, Tartu, Estonia; 5Centre for Cancer Biomarkers, De - partment of Clinical Science, University of Bergen, Bergen, Norway and 6Translational Immunology Research Program and Department of Clinical Chemistry and Hematology, University of Helsinki, Helsinki, Finland ©2020 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2018.214882 Received: December 17, 2018. Accepted: July 8, 2019. Pre-published: July 11, 2019. Correspondence: CAROLINE A. HECKMAN - [email protected] HEIKKI KUUSANMÄKI - [email protected] Supplemental Material Phenotype-based drug screening reveals an association between venetoclax response and differentiation stage in acute myeloid leukemia Authors: Heikki Kuusanmäki1, 2, Aino-Maija -

Sorafenib and Omacetaxine Mepesuccinate As a Safe and Effective Treatment for Acute Myeloid Leukemia Carrying Internal Tandem Du
Original Article Sorafenib and Omacetaxine Mepesuccinate as a Safe and Effective Treatment for Acute Myeloid Leukemia Carrying Internal Tandem Duplication of Fms-Like Tyrosine Kinase 3 Chunxiao Zhang, MSc1; Stephen S. Y. Lam, MBBS, PhD1; Garret M. K. Leung, MBBS1; Sze-Pui Tsui, MSc2; Ning Yang, PhD1; Nelson K. L. Ng, PhD1; Ho-Wan Ip, MBBS2; Chun-Hang Au, PhD3; Tsun-Leung Chan, PhD3; Edmond S. K. Ma, MBBS3; Sze-Fai Yip, MBBS4; Harold K. K. Lee, MBChB5; June S. M. Lau, MBChB6; Tsan-Hei Luk, MBChB6; Wa Li, MBChB7; Yok-Lam Kwong, MD 1; and Anskar Y. H. Leung, MD, PhD 1 BACKGROUND: Omacetaxine mepesuccinate (OME) has antileukemic effects against acute myeloid leukemia (AML) carrying an internal tandem duplication of Fms-like tyrosine kinase 3 (FLT3-ITD). A phase 2 clinical trial was conducted to evaluate a combina- tion treatment of sorafenib and omacetaxine mepesuccinate (SOME). METHODS: Relapsed or refractory (R/R) or newly diagnosed patients were treated with sorafenib (200-400 mg twice daily) and OME (2 mg daily) for 7 (first course) or 5 days (second course on- ward) every 21 days until disease progression or allogeneic hematopoietic stem cell transplantation (HSCT). The primary endpoint was composite complete remission, which was defined as complete remission (CR) plus complete remission with incomplete hematologic recovery (CRi). Secondary endpoints were leukemia-free survival (LFS) and overall survival (OS). RESULTS: Thirty-nine R/R patients and 5 newly diagnosed patients were recruited. Among the R/R patients, 28 achieved CR or CRi. Two patients showed partial remission, and 9 patients did not respond. -

Potential Biomarkers for Treatment Response to the BCL-2 Inhibitor Venetoclax: State of the Art and Future Directions
cancers Review Potential Biomarkers for Treatment Response to the BCL-2 Inhibitor Venetoclax: State of the Art and Future Directions Haneen T. Salah 1 , Courtney D. DiNardo 2 , Marina Konopleva 2 and Joseph D. Khoury 3,* 1 College of Medicine, Alfaisal University, Riyadh 11533, Saudi Arabia; [email protected] 2 Department of Leukemia, The University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA; [email protected] (C.D.D.); [email protected] (M.K.) 3 Department of Hematopathology, The University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA * Correspondence: [email protected] Simple Summary: Apoptosis dysergulation is vital to oncogenesis. Efforts to mitigate this cancer hallmark have been ongoing for decades, focused mostly on inhibiting BCL-2, a key anti-apoptosis effector. The approval of venetoclax, a selective BCL-2 inhibitor, for clinical use has been a turning point in the field of oncology. While resulting in impressive improvement in objective outcomes, particularly for patients with chronic lymphocytic leukemia/small lymphocytic lymphoma and acute myeloid leukemia, the use of venetoclax has exposed a variety of resistance mechanisms to BCL-2 inhibition. As the field continues to move forward, improved understanding of such mechanisms and the potential biomarkers that could be harnessed to optimize patient selection for therapies that include venetoclax and next-generation BCL-2 inhibitors are gaining increased importance. Abstract: Intrinsic apoptotic pathway dysregulation plays an essential role in all cancers, particularly hematologic malignancies. This role has led to the development of multiple therapeutic agents Citation: Salah, H.T.; DiNardo, C.D.; targeting this pathway. -

(INN) for Pharmaceutical Substances" WHO/EMP/RHT/TSN/2018.1
INN Working Document 20.484 13/07/2020 Addendum1 to "The use of stems in the selection of International Nonproprietary names (INN) for pharmaceutical substances" WHO/EMP/RHT/TSN/2018.1 Programme on International Nonproprietary Names (INN) Medicines and Health Products World Health Organization, Geneva © World Health Organization 2020 - All rights reserved. The contents of this document may not be reviewed, abstracted, quoted, referenced, reproduced, transmitted, distributed, translated or adapted, in part or in whole, in any form or by any means, without explicit prior authorization of the WHO INN Programme. This document contains the collective views of the INN Expert Group and does not necessarily represent the decisions or the stated policy of the World Health Organization. Addendum1 to "The use of stem s in the selection of International Nonproprietary Names (INN) for pharmaceutical substances" - WHO/EMP/RHT/TSN/2018.1 1 This addendum is a cumulative list of all new stems selected by the INN Expert Group since the publication of "The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances" 2018. -adenant adenosine receptors antagonists ciforadenant (118), preladenant (99), taminadenant (120), tozadenant (106), vipadenant (103) -caftor cystic fibrosis transmembrane regulator (CFTR) protein modulators, correctors, and amplifiers bamocaftor (121), deutivacaftor (118), elexacaftor (121), galicaftor (119), icenticaftor (122), ivacaftor (104), lumacaftor (105), navocaftor (121), nesolicaftor -

Standard Oncology Criteria C16154-A
Prior Authorization Criteria Standard Oncology Criteria Policy Number: C16154-A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE DUE BEFORE 03/2016 12/2/2020 1/26/2022 HCPCS CODING TYPE OF CRITERIA LAST P&T APPROVAL/VERSION N/A RxPA Q1 2021 20210127C16154-A PRODUCTS AFFECTED: See dosage forms DRUG CLASS: Antineoplastic ROUTE OF ADMINISTRATION: Variable per drug PLACE OF SERVICE: Retail Pharmacy, Specialty Pharmacy, Buy and Bill- please refer to specialty pharmacy list by drug AVAILABLE DOSAGE FORMS: Abraxane (paclitaxel protein-bound) Cabometyx (cabozantinib) Erwinaze (asparaginase) Actimmune (interferon gamma-1b) Calquence (acalbrutinib) Erwinia (chrysantemi) Adriamycin (doxorubicin) Campath (alemtuzumab) Ethyol (amifostine) Adrucil (fluorouracil) Camptosar (irinotecan) Etopophos (etoposide phosphate) Afinitor (everolimus) Caprelsa (vandetanib) Evomela (melphalan) Alecensa (alectinib) Casodex (bicalutamide) Fareston (toremifene) Alimta (pemetrexed disodium) Cerubidine (danorubicin) Farydak (panbinostat) Aliqopa (copanlisib) Clolar (clofarabine) Faslodex (fulvestrant) Alkeran (melphalan) Cometriq (cabozantinib) Femara (letrozole) Alunbrig (brigatinib) Copiktra (duvelisib) Firmagon (degarelix) Arimidex (anastrozole) Cosmegen (dactinomycin) Floxuridine Aromasin (exemestane) Cotellic (cobimetinib) Fludara (fludarbine) Arranon (nelarabine) Cyramza (ramucirumab) Folotyn (pralatrexate) Arzerra (ofatumumab) Cytosar-U (cytarabine) Fusilev (levoleucovorin) Asparlas (calaspargase pegol-mknl Cytoxan (cyclophosphamide) -

Strategic Therapeutic Targeting to Overcome Venetoclax Resistance in Aggressive B-Cell Lymphomas Lan V
Published OnlineFirst April 17, 2018; DOI: 10.1158/1078-0432.CCR-17-3004 Cancer Therapy: Preclinical Clinical Cancer Research Strategic Therapeutic Targeting to Overcome Venetoclax Resistance in Aggressive B-cell Lymphomas Lan V. Pham1, Shengjian Huang2, Hui Zhang2, Jun Zhang1, Taylor Bell2, Shouhao Zhou3, Elizabeth Pogue1, Zhiyong Ding4, Laura Lam2, Jason Westin2, R. Eric Davis2, Ken H.Young1, L. Jeffrey Medeiros1, Richard J. Ford1, Krystle Nomie2, Leo Zhang2, and Michael Wang2,5 Abstract Purpose: B-cell lymphoma-2 (BCL-2), an antiapoptotic protein clax response were identified. We demonstrate that DLBCL and often dysregulated in B-cell lymphomas, promotes cell survival MCL cell lines, primary patient samples, and PDX mouse and provides protection from stress. A recent phase I first-in- models expressing high BCL-2 levels are extremely sensitive to human study of the BCL-2 inhibitor venetoclax in non-Hodgkin venetoclax treatment. Proteomics studies showed that veneto- lymphoma showed an overall response rate of 44%. These prom- clax substantially alters the expression levels and phosphory- ising clinical results prompted our examination of the biological lation status of key proteins involved in cellular processes, effects and mechanism of action underlying venetoclax activity in including the DNA damage response, cell metabolism, cell aggressive B-cell lymphoma, including mantle cell lymphoma growth/survival, and apoptosis. Short- and long-term exposure (MCL) and diffuse large B-cell lymphoma (DLBCL). to venetoclax inhibited PTEN expression, leading to enhanced Experimental Design: MCL and DLBCL cell lines, primary AKT pathway activation and concomitant susceptibility to patient samples, and in vivo patient-derived xenograft (PDX) PI3K/AKT inhibition. -

Hematology Profile Plus
175 Technology Drive, Suite 100, Irvine, CA 92618 Tel: 1-866-484-8870 genomictestingcooperative.com CLIA #: 05D2111917 CAP #: 9441547 Hematology Profile Plus Patient Name: Ordering Physician: Date of Birth: 10/11/1960 Physician ID: Gender (M/F): M Accession #: 100712 Client: Specimen Type: Tissue Case #: Specimen ID: Body Site: Lymph node MRN: Indication for Testing: C83.90 Non-follicular (diffuse) lymphoma unspecified, unspecified site Collected Date: 02/18/2019 Time: 12:00 AM Received Date: 08/07/2019 Time: 11:50 AM Reported Date: 08/20/2019 Time: 08:13 AM Test Description: This is a comprehensive molecular profile which uses next generation sequencing (NGS), fragment length analysis and Sanger Sequencing testing to identify molecular abnormalities in DNA of 177 genes and RNA in 68 genes implicated in hematologic neoplasms, including leukemia, lymphoma melanoma and MDS. Whenever possible, clinical relevance and implications of detected abnormalities are described below. Detected Genomic Alterations Detected Genomic Alterations PRDM1 CD79B (Double) CDK12 KDM6A HUWE1 ARHGEF12 SPOP Heterogeneity Heterogeneity There is a dominant abnormal clone with PRDM1 mutation. The CD79B, CDK12, KDM6A, HUWE1, ARHGEF12, and SPOP mutations are detected in subclones. Expression Expression Expression of B-cell markers (CD19, CD22, CD79A, Significantly high expression of PD-L1 and CTLA4 PAX5). However, CD79B mRNA is relatively low. mRNA High expression of Ki67 mRNA Expression profile consistent with ABC type 1 Diagnostic Implications Diagnostic Implications -

Treatment Protocol – Information for Healthcare Professionals
Early Access to Medicines Scheme – Treatment protocol – Information for healthcare professionals Introduction The aim of the Early Access to Medicines Scheme (EAMS) is to provide earlier availability of promising new unlicensed and ‘off label’ medicines to UK patients that have a high unmet clinical need. The medicinal products included in the scheme are those that are intended to treat, diagnose or prevent seriously debilitating or life threatening conditions where there are no adequate treatment options. More information about the scheme can be found here: http://www.mhra.gov.uk/Howweregulate/Innovation/EarlyaccesstomedicinesschemeEAMS/index. htm This information is intended for healthcare professionals and is provided by the pharmaceutical company that manufactures the medicine. This medicine does not yet have a licence (marketing authorisation) and the information is provided to assist the doctor in prescribing an unlicensed medicine. Guidance on prescribing unlicensed medicines can be found on the GMC webpage: http://www.gmc-uk.org/mobile/14327 The scientific opinion is based on the information supplied to the MHRA on the benefits and risks of a promising new medicine. As such this is a scientific opinion and should not be regarded as a medicine licensed by the MHRA or a future commitment by the MHRA to licence such a medicine. The prescribing doctor should also refer to the summary information on the pharmacovigilance system which is provided in the document ‘Early Access to Medicines Scheme – Treatment protocol – Information on the pharmacovigilance system’. EAMS Information for HCP Venetoclax Page 1 Information for the healthcare professionals: 1. NAME OF THE MEDICINAL PRODUCT Venetoclax 10 mg film-coated tablets Venetoclax 50 mg film-coated tablets Venetoclax 100 mg film-coated tablets 2.