A Novel CDK9 Inhibitor Increases the Efficacy of Venetoclax (ABT-199) in Multiple Models of Hematologic Malignancies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Prospective, Multicenter, Phase-II Trial of Ibrutinib Plus Venetoclax In
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 A prospective, multicenter, phase-II trial of ibrutinib plus venetoclax in patients with creatinine clearance ≥ 30 ml/min who have relapsed or refractory chronic lymphocytic leukemia (RR-CLL) with or without TP53 aberrations HOVON 141 CLL / VIsion Trial of the HOVON and Nordic CLL study groups PROTOCOL Principal Investigator : Arnon P Kater (HOVON) Carsten U Niemann (Nordic CLL study Group)) Sponsor : HOVON EudraCT number : 2016-002599-29 ; Page 1 of 107 Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 LOCAL INVESTIGATOR SIGNATURE PAGE Local site name: Signature of Local Investigator Date Printed Name of Local Investigator By my signature, I agree to personally supervise the conduct of this study in my affiliation and to ensure its conduct in compliance with the protocol, informed consent, IRB/EC procedures, the Declaration of Helsinki, ICH Good Clinical Practices guideline, the EU directive Good Clinical Practice (2001-20-EG), and local regulations governing the conduct of clinical studies. -

Selective Targeting of Cyclin E1-Amplified High-Grade Serous Ovarian Cancer by Cyclin-Dependent Kinase 2 and AKT Inhibition
Published OnlineFirst September 23, 2016; DOI: 10.1158/1078-0432.CCR-16-0620 Biology of Human Tumors Clinical Cancer Research Selective Targeting of Cyclin E1-Amplified High-Grade Serous Ovarian Cancer by Cyclin- Dependent Kinase 2 and AKT Inhibition George Au-Yeung1,2, Franziska Lang1, Walid J. Azar1, Chris Mitchell1, Kate E. Jarman3, Kurt Lackovic3,4, Diar Aziz5, Carleen Cullinane1,6, Richard B. Pearson1,2,7, Linda Mileshkin2,8, Danny Rischin2,8, Alison M. Karst9, Ronny Drapkin10, Dariush Etemadmoghadam1,2,5, and David D.L. Bowtell1,2,7,11 Abstract Purpose: Cyclin E1 (CCNE1) amplification is associated with Results: We validate CDK2 as a therapeutic target by demon- primary treatment resistance and poor outcome in high-grade strating selective sensitivity to gene suppression. However, we found serous ovarian cancer (HGSC). Here, we explore approaches to that dinaciclib did not trigger amplicon-dependent sensitivity in a target CCNE1-amplified cancers and potential strategies to over- panel of HGSC cell lines. A high-throughput compound screen come resistance to targeted agents. identified synergistic combinations in CCNE1-amplified HGSC, Experimental Design: To examine dependency on CDK2 in including dinaciclib and AKT inhibitors. Analysis of genomic data CCNE1-amplified HGSC, we utilized siRNA and conditional from TCGA demonstrated coamplification of CCNE1 and AKT2. shRNA gene suppression, and chemical inhibition using dina- Overexpression of Cyclin E1 and AKT isoforms, in addition to ciclib, a small-molecule CDK2 inhibitor. High-throughput mutant TP53, imparted malignant characteristics in untransformed compound screening was used to identify selective synergistic fallopian tube secretory cells, the dominant site of origin of HGSC. -

The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia
International Journal of Molecular Sciences Review The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia Marta Weronika Lato 1 , Anna Przysucha 1, Sylwia Grosman 1, Joanna Zawitkowska 2 and Monika Lejman 3,* 1 Student Scientific Society, Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] (M.W.L.); [email protected] (A.P.); [email protected] (S.G.) 2 Department of Pediatric Hematology, Oncology and Transplantology, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 3 Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland * Correspondence: [email protected] Abstract: Childhood acute lymphoblastic leukemia is a genetically heterogeneous cancer that ac- counts for 10–15% of T-cell acute lymphoblastic leukemia (T-ALL) cases. The T-ALL event-free survival rate (EFS) is 85%. The evaluation of structural and numerical chromosomal changes is important for a comprehensive biological characterization of T-ALL, but there are currently no ge- netic prognostic markers. Despite chemotherapy regimens, steroids, and allogeneic transplantation, relapse is the main problem in children with T-ALL. Due to the development of high-throughput molecular methods, the ability to define subgroups of T-ALL has significantly improved in the last few years. The profiling of the gene expression of T-ALL has led to the identification of T-ALL subgroups, and it is important in determining prognostic factors and choosing an appropriate treatment. Novel therapies targeting molecular aberrations offer promise in achieving better first remission with the Citation: Lato, M.W.; Przysucha, A.; hope of preventing relapse. -
Draft Matrix Post Referral PDF 189 KB
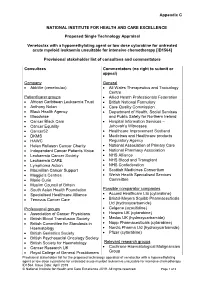
Appendix C NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Proposed Single Technology Appraisal Venetoclax with a hypomethylating agent or low dose cytarabine for untreated acute myeloid leukaemia unsuitable for intensive chemotherapy [ID1564] Provisional stakeholder list of consultees and commentators Consultees Commentators (no right to submit or appeal) Company General • AbbVie (venetoclax) • All Wales Therapeutics and Toxicology Centre Patient/carer groups • Allied Health Professionals Federation • African Caribbean Leukaemia Trust • British National Formulary • Anthony Nolan • Care Quality Commission • Black Health Agency • Department of Health, Social Services • Bloodwise and Public Safety for Northern Ireland • Cancer Black Care • Hospital Information Services – • Cancer Equality Jehovah’s Witnesses • Cancer52 • Healthcare Improvement Scotland • DKMS • Medicines and Healthcare products • HAWC Regulatory Agency • Helen Rollason Cancer Charity • National Association of Primary Care • Independent Cancer Patients Voice • National Pharmacy Association • Leukaemia Cancer Society • NHS Alliance • Leukaemia CARE • NHS Blood and Transplant • Lymphoma Action • NHS Confederation • Macmillan Cancer Support • Scottish Medicines Consortium • Maggie’s Centres • Welsh Health Specialised Services • Marie Curie Committee • Muslim Council of Britain • South Asian Health Foundation Possible comparator companies • Specialised Healthcare Alliance • Accord Healthcare Ltd (cytarabine) • Tenovus Cancer Care • Bristol-Meyers Squibb Pharmaceuticals Ltd -

The CDK4/6 Inhibitor LY2835219 Has Potent Activity in Combination with Mtor Inhibitor in Head and Neck Squamous Cell Carcinoma
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 7, No. 12 The CDK4/6 inhibitor LY2835219 has potent activity in combination with mTOR inhibitor in head and neck squamous cell carcinoma Bo Mi Ku1,*, Seong Yoon Yi3,*, Jiae Koh1, Yeon-Hee Bae1, Jong-Mu Sun2, Se-hoon Lee2, Jin Seok Ahn2, Keunchil Park2, Myung-Ju Ahn2 1 Samsung Biomedical Research Institute, Seoul, Korea 2 Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea 3 Division of Hematology-Oncology, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Gyeonggi-do, Korea *These authors contributed equally to this work Correspondence to: Myung-Ju Ahn, e-mail: [email protected] Keywords: head and neck cancer, CDK4/6 inhibitor, mTOR, cell cycle, targeted therapy Received: September 15, 2015 Accepted: January 23, 2016 Published: February 21, 2016 ABSTRACT Deletion of CDKN2A (p16) or amplification ofCCND1 (cyclin D1) occurs commonly in head and neck squamous cell carcinoma (HNSCC) and induces sustained cyclin- dependent kinase (CDK) 4/6 activation. Here, we report the antiproliferative activity of LY2835219, a selective CDK4/6 inhibitor through inhibition of CDK4/6-dependent Ser780 phosphorylation in retinoblastoma (RB) and induction of cell cycle arrest in HNSCC cells. In addition, we demonstrated the antitumor effects of HNSCC xenografts to LY2835219 in vivo. Given the limited effect in HNSCC as a single-agent treatment with LY2835219, a combinational strategy is required to enhance antitumor activity. At the molecular level, we found that LY2835219 inhibited activation of AKT and ERK, but not mTOR. The combination of LY2835219 with mTOR inhibitor was found to be more effective than either drug alone in vitro and in vivo. -

Identification of Candidate Repurposable Drugs to Combat COVID-19 Using a Signature-Based Approach
www.nature.com/scientificreports OPEN Identifcation of candidate repurposable drugs to combat COVID‑19 using a signature‑based approach Sinead M. O’Donovan1,10, Ali Imami1,10, Hunter Eby1, Nicholas D. Henkel1, Justin Fortune Creeden1, Sophie Asah1, Xiaolu Zhang1, Xiaojun Wu1, Rawan Alnafsah1, R. Travis Taylor2, James Reigle3,4, Alexander Thorman6, Behrouz Shamsaei4, Jarek Meller4,5,6,7,8 & Robert E. McCullumsmith1,9* The COVID‑19 pandemic caused by the novel SARS‑CoV‑2 is more contagious than other coronaviruses and has higher rates of mortality than infuenza. Identifcation of efective therapeutics is a crucial tool to treat those infected with SARS‑CoV‑2 and limit the spread of this novel disease globally. We deployed a bioinformatics workfow to identify candidate drugs for the treatment of COVID‑19. Using an “omics” repository, the Library of Integrated Network‑Based Cellular Signatures (LINCS), we simultaneously probed transcriptomic signatures of putative COVID‑19 drugs and publicly available SARS‑CoV‑2 infected cell lines to identify novel therapeutics. We identifed a shortlist of 20 candidate drugs: 8 are already under trial for the treatment of COVID‑19, the remaining 12 have antiviral properties and 6 have antiviral efcacy against coronaviruses specifcally, in vitro. All candidate drugs are either FDA approved or are under investigation. Our candidate drug fndings are discordant with (i.e., reverse) SARS‑CoV‑2 transcriptome signatures generated in vitro, and a subset are also identifed in transcriptome signatures generated from COVID‑19 patient samples, like the MEK inhibitor selumetinib. Overall, our fndings provide additional support for drugs that are already being explored as therapeutic agents for the treatment of COVID‑19 and identify promising novel targets that are worthy of further investigation. -

Cyclacel's CYC065 CDK Inhibitor Demonstrates Synergy With
Cyclacel’s CYC065 CDK Inhibitor Demonstrates Synergy With Venetoclax By Dual Targeting Of Chronic Lymphocytic Leukemia April 17, 2018 Suppression of both BCl-2 and Mcl-1 anti-apoptotic proteins is a novel strategy in CLL BERKELEY HEIGHTS, N.J., April 17, 2018 (GLOBE NEWSWIRE) -- Cyclacel Pharmaceuticals, Inc. (NASDAQ:CYCC) (NASDAQ:CYCCP) ("Cyclacel" or the "Company"), a biopharmaceutical company developing oral therapies that target various phases of cell cycle control for the treatment of cancer and other serious disorders, today announced the presentation by investigators led by William Plunkett, PhD, Professor and Deputy Chair, Department of Experimental Therapeutics, The University of Texas MD Anderson Cancer Center, Houston, Texas, of preclinical data demonstrating strong synergy between Cyclacel’s CDK2/9 inhibitor, CYC065, and the Bcl-2 inhibitor, venetoclax (ABT-199, AbbVie) in chronic lymphocytic leukemia (CLL) samples obtained from patients. The data were presented at the American Association for Cancer Research (AACR) Annual Meeting being held April 14-18, 2018 in Chicago, Illinois. “The MD Anderson data show that the combination of CYC065 and venetoclax is strongly synergistic in primary CLL cells from patients, including those with 17p deletions. In addition, the combination was active in two CLL samples which were resistant to either agent alone. These findings support the hypothesis that dual targeting of the Mcl-1- and Bcl-2-dependent mechanisms could induce synergistic cell death by apoptosis,” said Spiro Rombotis, President and Chief Executive Officer of Cyclacel. “Last weekend during the same AACR conference, we reported that CYC065 durably suppresses Mcl-1, a member of the Bcl-2 family of survival proteins, in patients with advanced solid tumors1. -

Pharmacologic Properties of AG-012986, a Pan-Cyclin- Dependent Kinase Inhibitor with Antitumor Efficacy
818 Pharmacologic properties of AG-012986, a pan-cyclin- dependent kinase inhibitor with antitumor efficacy Cathy Zhang,1 Karen Lundgren,1 Zhengming Yan,1 optimization of AG-012986 provided guidance for select- Maria E. Arango,1 Sharon Price,1 Andrea Huber,1 ing a treatment schedule to achieve the best antitumor Joseph Higgins,1 Gabriel Troche,1 efficacy while minimizing the risk of adverse side effects. Judith Skaptason,2 Tatiana Koudriakova,2 [Mol Cancer Ther 2008;7(4):818–28] Jim Nonomiya,4 Michelle Yang,5 1 1 1 Patrick O’Connor, Steve Bender, Gerrit Los, Introduction Cristina Lewis,4 and Bart Jessen3 Cyclin-dependent kinases (CDK) and their regulatory Departments of 1Cancer Biology, 2Pharmacokinetics, Dynamics cyclin partners play critical roles in cell cycle control and and Metabolism, 3Drug Safety Research and Development, the regulation of cell transcription. Progression through 4 5 Biochemical Pharmacology, and Medicinal Chemistry, the different stages of cell cycle is governed by the Pfizer Global Research and Development, La Jolla, California activities of the CDK1, CDK2, CDK4, CDK6, and possibly CDK3. CDK4/cyclin D, CDK6/cyclin D, and CDK2/cyclin E Abstract phosphorylate the retinoblastoma (Rb) protein at multiple AG-012986 is a multitargeted cyclin-dependent kinase sites, which results in activation of the E2F family of (CDK) inhibitor active against CDK1, CDK2, CDK4/6, transcription factors and serves as a trigger for cells to CDK5, and CDK9, with selectivity over a diverse panel of advance beyond the G1 checkpoint into S phase (1–3). non-CDK kinases. Here, we report the potent antitumor During S phase, CDK2/cyclin A phosphorylates several efficacies of AG-012986 against multiple tumor lines proteins, including E2F, to regulate progression through in vitro and in vivo. -

Anticancer and Radiosensitizing Effects of the Cyclin-Dependent Kinase Inhibitors, AT7519 and SNS‑032, on Cervical Cancer
INTERNATIONAL JOURNAL OF ONCOLOGY 53: 703-712, 2018 Anticancer and radiosensitizing effects of the cyclin-dependent kinase inhibitors, AT7519 and SNS-032, on cervical cancer MI AE KANG1*, WONWOO KIM2*, HYE-RAM JO1,3, YOUNG-JOO SHIN4, MOON-HONG KIM5 and JAE-HOON JEONG1,3 1Division of Applied Radiation Bioscience, and 2Radiation Non-Clinic Center, Korea Institute of Radiological and Medical Science, Seoul 01812; 3Radiological and Medico-Oncological Sciences, Korea University of Science and Technology, Daejeon 34113; 4Department of Radiation Oncology, Inje University Sanggye Paik Hospital, Seoul 01757; 5Department of Obstetrics and Gynecology, Korea Institute of Radiological and Medical Sciences, Seoul 01812, Republic of Korea Received January 30, 2018; Accepted May 17, 2018 DOI: 10.3892/ijo.2018.4424 Abstract. Cyclin-dependent kinases (CDK) are considered the utilization of AT7519 and SNS-032 as part of an adjuvant to be potential targets of anticancer drugs that can interrupt treatment may help control cervical cancer progression. the uncontrolled division of cancer cells. In this study, we selected two selective CDK inhibitors, AT7519 and SNS-032, Introduction from current clinical trials and examined their anticancer and radiosensitizing effects in a cervical cancer model. SNS-032 Cyclin-dependent kinases (CDKs) are present in all known was found to be more potent than AT7519, with a lower half eukaryotes, and their regulatory functions during the cell cycle maximal inhibitory concentration (IC50) value. Both AT7519 are evolutionarily conserved. Cyclin-CDK complexes phos- and SNS-032 induced the apoptosis, premature senescence and phorylate specific substrates, according to the requirements cytostasis of cervical cancer cells, which led to the attenuation of a particular cell cycle phase. -

Journal Pre-Proof
Journal Pre-proof 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC † 5) F. Cardoso, S. Paluch-Shimon, E. Senkus, G. Curigliano, M.S. Aapro, F. André, C.H. Barrios, J. Bergh, G.S. Bhattacharyya, L. Biganzoli, F. Boyle, M.-J. Cardoso, L.A. Carey, J. Cortés, N.S. El Saghir, M. Elzayat, A. Eniu, L. Fallowfield, P.A. Francis, K. Gelmon, J. Gligorov, R. Haidinger, N. Harbeck, X. Hu, B. Kaufman, R. Kaur, B.E. Kiely, S.-B. Kim, N.U. Lin, S.A. Mertz, S. Neciosup, B.V. Offersen, S. Ohno, O. Pagani, A. Prat, F. Penault-Llorca, H.S. Rugo, G.W. Sledge, C. Thomssen, D.A. Vorobiof, T. Wiseman, B. Xu, L. Norton, A. Costa, E.P. Winer PII: S0923-7534(20)42460-3 DOI: https://doi.org/10.1016/j.annonc.2020.09.010 Reference: ANNONC 337 To appear in: Annals of Oncology Received Date: 21 August 2020 Revised Date: 15 September 2020 Accepted Date: 16 September 2020 Please cite this article as: Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, Barrios CH, Bergh J, Bhattacharyya GS, Biganzoli L, Boyle F, Cardoso MJ, Carey LA, Cortés J, El Saghir NS, Elzayat M, Eniu A, Fallowfield L, Francis PA, Gelmon K, Gligorov J, Haidinger R, Harbeck N, Hu X, Kaufman B, Kaur R, Kiely BE, Kim SB, Lin NU, Mertz SA, Neciosup S, Offersen BV, Ohno S, Pagani O, Prat A, Penault-Llorca F, Rugo HS, Sledge GW, Thomssen C, Vorobiof DA, Wiseman T, Xu B, Norton L, Costa A, Winer EP, 5th ESO-ESMO international consensus guidelines for advanced breast † cancer (ABC 5) , Annals of Oncology (2020), doi: https://doi.org/10.1016/j.annonc.2020.09.010. -

Phenotype-Based Drug Screening Reveals Association Between Venetoclax Response and Differentiation Stage in Acute Myeloid Leukemia
Acute Myeloid Leukemia SUPPLEMENTARY APPENDIX Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia Heikki Kuusanmäki, 1,2 Aino-Maija Leppä, 1 Petri Pölönen, 3 Mika Kontro, 2 Olli Dufva, 2 Debashish Deb, 1 Bhagwan Yadav, 2 Oscar Brück, 2 Ashwini Kumar, 1 Hele Everaus, 4 Bjørn T. Gjertsen, 5 Merja Heinäniemi, 3 Kimmo Porkka, 2 Satu Mustjoki 2,6 and Caroline A. Heckman 1 1Institute for Molecular Medicine Finland, Helsinki Institute of Life Science, University of Helsinki, Helsinki; 2Hematology Research Unit, Helsinki University Hospital Comprehensive Cancer Center, Helsinki; 3Institute of Biomedicine, School of Medicine, University of Eastern Finland, Kuopio, Finland; 4Department of Hematology and Oncology, University of Tartu, Tartu, Estonia; 5Centre for Cancer Biomarkers, De - partment of Clinical Science, University of Bergen, Bergen, Norway and 6Translational Immunology Research Program and Department of Clinical Chemistry and Hematology, University of Helsinki, Helsinki, Finland ©2020 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2018.214882 Received: December 17, 2018. Accepted: July 8, 2019. Pre-published: July 11, 2019. Correspondence: CAROLINE A. HECKMAN - [email protected] HEIKKI KUUSANMÄKI - [email protected] Supplemental Material Phenotype-based drug screening reveals an association between venetoclax response and differentiation stage in acute myeloid leukemia Authors: Heikki Kuusanmäki1, 2, Aino-Maija -

Sorafenib and Omacetaxine Mepesuccinate As a Safe and Effective Treatment for Acute Myeloid Leukemia Carrying Internal Tandem Du
Original Article Sorafenib and Omacetaxine Mepesuccinate as a Safe and Effective Treatment for Acute Myeloid Leukemia Carrying Internal Tandem Duplication of Fms-Like Tyrosine Kinase 3 Chunxiao Zhang, MSc1; Stephen S. Y. Lam, MBBS, PhD1; Garret M. K. Leung, MBBS1; Sze-Pui Tsui, MSc2; Ning Yang, PhD1; Nelson K. L. Ng, PhD1; Ho-Wan Ip, MBBS2; Chun-Hang Au, PhD3; Tsun-Leung Chan, PhD3; Edmond S. K. Ma, MBBS3; Sze-Fai Yip, MBBS4; Harold K. K. Lee, MBChB5; June S. M. Lau, MBChB6; Tsan-Hei Luk, MBChB6; Wa Li, MBChB7; Yok-Lam Kwong, MD 1; and Anskar Y. H. Leung, MD, PhD 1 BACKGROUND: Omacetaxine mepesuccinate (OME) has antileukemic effects against acute myeloid leukemia (AML) carrying an internal tandem duplication of Fms-like tyrosine kinase 3 (FLT3-ITD). A phase 2 clinical trial was conducted to evaluate a combina- tion treatment of sorafenib and omacetaxine mepesuccinate (SOME). METHODS: Relapsed or refractory (R/R) or newly diagnosed patients were treated with sorafenib (200-400 mg twice daily) and OME (2 mg daily) for 7 (first course) or 5 days (second course on- ward) every 21 days until disease progression or allogeneic hematopoietic stem cell transplantation (HSCT). The primary endpoint was composite complete remission, which was defined as complete remission (CR) plus complete remission with incomplete hematologic recovery (CRi). Secondary endpoints were leukemia-free survival (LFS) and overall survival (OS). RESULTS: Thirty-nine R/R patients and 5 newly diagnosed patients were recruited. Among the R/R patients, 28 achieved CR or CRi. Two patients showed partial remission, and 9 patients did not respond.