Venclyxto, INN-Venetoclax;
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Prospective, Multicenter, Phase-II Trial of Ibrutinib Plus Venetoclax In
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 A prospective, multicenter, phase-II trial of ibrutinib plus venetoclax in patients with creatinine clearance ≥ 30 ml/min who have relapsed or refractory chronic lymphocytic leukemia (RR-CLL) with or without TP53 aberrations HOVON 141 CLL / VIsion Trial of the HOVON and Nordic CLL study groups PROTOCOL Principal Investigator : Arnon P Kater (HOVON) Carsten U Niemann (Nordic CLL study Group)) Sponsor : HOVON EudraCT number : 2016-002599-29 ; Page 1 of 107 Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 LOCAL INVESTIGATOR SIGNATURE PAGE Local site name: Signature of Local Investigator Date Printed Name of Local Investigator By my signature, I agree to personally supervise the conduct of this study in my affiliation and to ensure its conduct in compliance with the protocol, informed consent, IRB/EC procedures, the Declaration of Helsinki, ICH Good Clinical Practices guideline, the EU directive Good Clinical Practice (2001-20-EG), and local regulations governing the conduct of clinical studies. -

214120Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 214120Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number NDA 214120 Application Type Type 3 Priority or Standard Priority Submit Date 3/3/2020 Received Date 3/3/2020 PDUFA Goal Date 9/3/2020 Office/Division OOD/DHM1 Review Completion Date 9/1/2020 Applicant Celgene Corporation Established Name Azacitidine (Proposed) Trade Name Onureg Pharmacologic Class Nucleoside metabolic inhibitor Formulations Tablet (200 mg, 300 mg) (b) (4) Applicant Proposed Indication/Population Recommendation on Regulatory Regular approval Action Recommended Indication/ For continued treatment of adult patients with acute Population myeloid leukemia who achieved first complete remission (CR) or complete remission with incomplete blood count recovery (CRi) following intensive induction chemotherapy and are not able to complete intensive curative therapy. SNOMED CT for the Recommended 91861009 Indication/Population Recommended Dosing Regimen 300 mg orally daily on Days 1 through 14 of each 28-day cycle Reference ID: 4664570 NDA Multidisciplinary Review and Evaluation NDA 214120 Onureg (azacitidine tablets) TABLE OF CONTENTS TABLE OF CONTENTS ................................................................................................................................... 2 TABLE OF TABLES ....................................................................................................................................... -

The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia
International Journal of Molecular Sciences Review The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia Marta Weronika Lato 1 , Anna Przysucha 1, Sylwia Grosman 1, Joanna Zawitkowska 2 and Monika Lejman 3,* 1 Student Scientific Society, Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] (M.W.L.); [email protected] (A.P.); [email protected] (S.G.) 2 Department of Pediatric Hematology, Oncology and Transplantology, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 3 Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland * Correspondence: [email protected] Abstract: Childhood acute lymphoblastic leukemia is a genetically heterogeneous cancer that ac- counts for 10–15% of T-cell acute lymphoblastic leukemia (T-ALL) cases. The T-ALL event-free survival rate (EFS) is 85%. The evaluation of structural and numerical chromosomal changes is important for a comprehensive biological characterization of T-ALL, but there are currently no ge- netic prognostic markers. Despite chemotherapy regimens, steroids, and allogeneic transplantation, relapse is the main problem in children with T-ALL. Due to the development of high-throughput molecular methods, the ability to define subgroups of T-ALL has significantly improved in the last few years. The profiling of the gene expression of T-ALL has led to the identification of T-ALL subgroups, and it is important in determining prognostic factors and choosing an appropriate treatment. Novel therapies targeting molecular aberrations offer promise in achieving better first remission with the Citation: Lato, M.W.; Przysucha, A.; hope of preventing relapse. -

Expression of Genes by Hypomethylating Agents
Wolff et al. Cell Communication and Signaling (2017) 15:13 DOI 10.1186/s12964-017-0168-z REVIEW Open Access The double-edged sword of (re)expression of genes by hypomethylating agents: from viral mimicry to exploitation as priming agents for targeted immune checkpoint modulation Florian Wolff1, Michael Leisch2, Richard Greil2,3,4, Angela Risch1,4 and Lisa Pleyer2,3,4* Abstract Hypomethylating agents (HMAs) have been widely used over the last decade, approved for use in myelodysplastic syndrome (MDS), chronic myelomonocytic leukemia (CMML) and acute myeloid leukemia (AML). The proposed central mechanism of action of HMAs, is the reversal of aberrant methylation in tumor cells, thus reactivating CpG-island promoters and leading to (re)expression of tumor suppressor genes. Recent investigations into the mode of action of azacitidine (AZA) and decitabine (DAC) have revealed new molecular mechanisms that impinge on tumor immunity via induction of an interferon response, through activation of endogenous retroviral elements (ERVs) that are normally epigenetically silenced. Although the global demethylation of DNA by HMAs can induce anti-tumor effects, it can also upregulate the expression of inhibitory immune checkpoint receptors and their ligands, resulting in secondary resistance to HMAs. Recent studies have, however, suggested that this could be exploited to prime or (re)sensitize tumors to immune checkpoint inhibitor therapies. In recent years, immune checkpoints have been targeted by novel therapies, with the aim of (re)activating the host immune system to specifically eliminate malignant cells. Antibodies blocking checkpoint receptors have been FDA-approved for some solid tumors and a plethora of clinical trials testing these and other checkpoint inhibitors are under way. -

Epigenetics in Clinical Practice: the Examples of Azacitidine and Decitabine in Myelodysplasia and Acute Myeloid Leukemia
Leukemia (2013) 27, 1803–1812 & 2013 Macmillan Publishers Limited All rights reserved 0887-6924/13 www.nature.com/leu SPOTLIGHT REVIEW Epigenetics in clinical practice: the examples of azacitidine and decitabine in myelodysplasia and acute myeloid leukemia EH Estey Randomized trials have clearly demonstrated that the hypomethylating agents azacitidine and decitabine are more effective than ‘best supportive care’(BSC) in reducing transfusion frequency in ‘low-risk’ myelodysplasia (MDS) and in prolonging survival compared with BSC or low-dose ara-C in ‘high-risk’ MDS or acute myeloid leukemia (AML) with 21–30% blasts. They also appear equivalent to conventional induction chemotherapy in AML with 420% blasts and as conditioning regimens before allogeneic transplant (hematopoietic cell transplant, HCT) in MDS. Although azacitidine or decitabine are thus the standard to which newer therapies should be compared, here we discuss whether the improvement they afford in overall survival is sufficient to warrant a designation as a standard in treating individual patients. We also discuss pre- and post-treatment covariates, including assays of methylation to predict response, different schedules of administration, combinations with other active agents and use in settings other than active disease, in particular post HCT. We note that rational development of this class of drugs awaits delineation of how much of their undoubted effect in fact results from hypomethylation and reactivation of gene expression. Leukemia (2013) 27, 1803–1812; doi:10.1038/leu.2013.173 -
Draft Matrix Post Referral PDF 189 KB
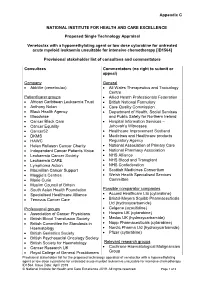
Appendix C NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Proposed Single Technology Appraisal Venetoclax with a hypomethylating agent or low dose cytarabine for untreated acute myeloid leukaemia unsuitable for intensive chemotherapy [ID1564] Provisional stakeholder list of consultees and commentators Consultees Commentators (no right to submit or appeal) Company General • AbbVie (venetoclax) • All Wales Therapeutics and Toxicology Centre Patient/carer groups • Allied Health Professionals Federation • African Caribbean Leukaemia Trust • British National Formulary • Anthony Nolan • Care Quality Commission • Black Health Agency • Department of Health, Social Services • Bloodwise and Public Safety for Northern Ireland • Cancer Black Care • Hospital Information Services – • Cancer Equality Jehovah’s Witnesses • Cancer52 • Healthcare Improvement Scotland • DKMS • Medicines and Healthcare products • HAWC Regulatory Agency • Helen Rollason Cancer Charity • National Association of Primary Care • Independent Cancer Patients Voice • National Pharmacy Association • Leukaemia Cancer Society • NHS Alliance • Leukaemia CARE • NHS Blood and Transplant • Lymphoma Action • NHS Confederation • Macmillan Cancer Support • Scottish Medicines Consortium • Maggie’s Centres • Welsh Health Specialised Services • Marie Curie Committee • Muslim Council of Britain • South Asian Health Foundation Possible comparator companies • Specialised Healthcare Alliance • Accord Healthcare Ltd (cytarabine) • Tenovus Cancer Care • Bristol-Meyers Squibb Pharmaceuticals Ltd -

A Novel CDK9 Inhibitor Increases the Efficacy of Venetoclax (ABT-199) in Multiple Models of Hematologic Malignancies
Leukemia (2020) 34:1646–1657 https://doi.org/10.1038/s41375-019-0652-0 ARTICLE Molecular targets for therapy A novel CDK9 inhibitor increases the efficacy of venetoclax (ABT-199) in multiple models of hematologic malignancies 1 1 2,3 4 1 5 6 Darren C. Phillips ● Sha Jin ● Gareth P. Gregory ● Qi Zhang ● John Xue ● Xiaoxian Zhao ● Jun Chen ● 1 1 1 1 1 1 Yunsong Tong ● Haichao Zhang ● Morey Smith ● Stephen K. Tahir ● Rick F. Clark ● Thomas D. Penning ● 2,7 3 5 1 4 2,7 Jennifer R. Devlin ● Jake Shortt ● Eric D. Hsi ● Daniel H. Albert ● Marina Konopleva ● Ricky W. Johnstone ● 8 1 Joel D. Leverson ● Andrew J. Souers Received: 27 November 2018 / Revised: 18 October 2019 / Accepted: 13 November 2019 / Published online: 11 December 2019 © The Author(s) 2019 Abstract MCL-1 is one of the most frequently amplified genes in cancer, facilitating tumor initiation and maintenance and enabling resistance to anti-tumorigenic agents including the BCL-2 selective inhibitor venetoclax. The expression of MCL-1 is maintained via P-TEFb-mediated transcription, where the kinase CDK9 is a critical component. Consequently, we developed a series of potent small-molecule inhibitors of CDK9, exemplified by the orally active A-1592668, with CDK selectivity profiles 1234567890();,: 1234567890();,: that are distinct from related molecules that have been extensively studied clinically. Short-term treatment with A-1592668 rapidly downregulates RNA pol-II (Ser 2) phosphorylation resulting in the loss of MCL-1 protein and apoptosis in MCL-1- dependent hematologic tumor cell lines. This cell death could be attenuated by either inhibiting caspases or overexpressing BCL-2 protein. -

Biological Heterogeneity of Chondrosarcoma: from (Epi) Genetics Through Stemness and Deregulated Signaling to Immunophenotype
cancers Review Biological Heterogeneity of Chondrosarcoma: From (Epi) Genetics through Stemness and Deregulated Signaling to Immunophenotype Agnieszka Zaj ˛ac 1 , Sylwia K. Król 2 , Piotr Rutkowski 1 and Anna M. Czarnecka 1,3,* 1 Department of Soft Tissue/Bone Sarcoma and Melanoma, Maria Sklodowska-Curie National Research Institute of Oncology, 02-781 Warsaw, Poland; [email protected] (A.Z.); [email protected] (P.R.) 2 Department of Molecular and Translational Oncology, Maria Sklodowska-Curie National Research Institute of Oncology, 02-781 Warsaw, Poland; [email protected] 3 Department of Experimental Pharmacology, Mossakowski Medical Research Centre, Polish Academy of Sciences, 02-176 Warsaw, Poland * Correspondence: [email protected] Simple Summary: Chondrosarcoma (ChS) is the second most frequently diagnosed malignant bone tumor of cartilaginous origin and is generally resistant to standard treatment options. In this paper, we aim to review the current state of the knowledge regarding ChS. We discuss the genetic, epigenetic, and molecular abnormalities underlying its substantial biological and clinical heterogeneity. This review summarizes the critical genetic and molecular drivers of ChS development and progression, contributing to its radio- and chemotherapy resistance. We describe genomic aberrations and point mutations, as well as epigenetic modifications and deregulated signal transduction pathways. We Citation: Zaj ˛ac,A.; Król, S.K.; provide an insight into the stem-like characteristics and immunophenotype of ChS. The paper also Rutkowski, P.; Czarnecka, A.M. outlines potential diagnostic and prognostic biomarkers of ChS and recently identified novel targets Biological Heterogeneity of for future pharmacological interventions in patients. Chondrosarcoma: From (Epi) Genetics through Stemness and Abstract: Deregulated Signaling to Chondrosarcoma (ChS) is a primary malignant bone tumor. -

Demethylation and Upregulation of an Oncogene Post Hypomethylating Treatment
medRxiv preprint doi: https://doi.org/10.1101/2020.07.21.20157776; this version posted July 26, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. Title: Demethylation and upregulation of an oncogene post hypomethylating treatment Authors: Yao-Chung Liu1,2,3,4°, Emiliano Fabiani5°, Junsu Kwon6°, Chong Gao1, Giulia Falconi5, Lia Valentini5, Carmelo Gurnari5, Yanjing V. Liu6, Adrianna I. Jones7, Junyu Yang1, Henry Yang6, Julie A. I. Thoms8, Ashwin Unnikrishnan9, John E. Pimanda8,9,10, Rongqing Pan11, Maria Teresa Voso5*, Daniel G. Tenen6,7*, Li Chai1* Affiliations: 1Department of Pathology, Brigham and Women's Hospital, Boston, MA 02115, USA 2Division of Hematology, Department of Medicine, Taipei Veterans General Hospital, Taipei, Taiwan 3Faculty of Medicine, School of Medicine, National Yang-Ming University, Taipei, Taiwan 4Program in Molecular Medicine, School of Life Science, National Yang-Ming University, Taipei, Taiwan 5Department of Biomedicine and Prevention, University of Tor Vergata, Rome, Italy 6Cancer Science Institute of Singapore, National University of Singapore, 117599, Singapore 7Harvard Stem Cell Institute, Harvard Medical School, Boston, MA 02115 USA 8School of Medical Sciences and Lowy Cancer Research Centre, Faculty of Medicine, UNSW Sydney, NSW 2052, Australia 9Prince of Wales Clinical School and Lowy Cancer Research Centre, Faculty of Medicine, UNSW Sydney, NSW 2052, Australia 10Department of Haematology, Prince of Wales Hospital, Randwick, NSW 2031, Australia 11 Department of Medical Oncology, Dana-Farber Cancer Institute, Boston, MA, 02115 °These authors contibute equally to this work *Co-corresponding authors: [email protected], [email protected], and [email protected] The authors have declared that no conflict of interest exists. -

A Phase II Study of Omacetaxine (OM) in Patients with Intermediate-1 and Higher Risk Myelodysplastic Syndrome (MDS) Post Hypomethylating Agent (HMA) Failure 2013-0870
Protocol Page A Phase II Study of Omacetaxine (OM) in Patients with Intermediate-1 and Higher Risk Myelodysplastic Syndrome (MDS) post Hypomethylating Agent (HMA) Failure 2013-0870 Core Protocol Information Short Title Omacetaxine in Patients with Intermediate-1 and Higher Risk MDS post HMA Failure Study Chair: Elias Jabbour Additional Contact: Jhinelle L. Graham Vicky H. Zoeller Leukemia Protocol Review Group Additional Memo Recipients: Recipients List OPR Recipients (for OPR use only) None Study Staff Recipients None Department: Leukemia Phone: 713-792-4764 Unit: 0428 Full Title: A Phase II Study of Omacetaxine (OM) in Patients with Intermediate-1 and Higher Risk Myelodysplastic Syndrome (MDS) post Hypomethylating Agent (HMA) Failure Protocol Type: Standard Protocol Protocol Phase: Phase II Version Status: Activated -- Closed to new patient entry as of 08/05/2018 Version: 08 Document Status: Saved as "Final" Submitted by: Vicky H. Zoeller--9/11/2017 12:24:33 PM OPR Action: Accepted by: Margaret Okoloise -- 9/14/2017 12:09:50 PM Which Committee will review this protocol? The Clinical Research Committee - (CRC) Protocol Body 2013-0870 March 6, 2017 1 A Phase II Study of Omacetaxine (OM) in Patients with Intermediate-1 and Higher Risk Myelodysplastic Syndrome (MDS) post Hypomethylating Agent (HMA) Failure 2013-0870 March 6, 2017 2 Table of Contents 1.0 Objectives .................................................................................................. 3 2.0 Background .............................................................................................. -

Immunotherapy of MDS: You Can Run, but You Can’T Hide
Author Manuscript Published OnlineFirst on December 28, 2017; DOI: 10.1158/1078-0432.CCR-17-2960 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Immunotherapy of MDS: you can run, but you can’t hide Ephraim Joseph Fuchs, MD, MBA Division of Hematologic Malignancies, Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Baltimore, MD, USA e-mail: [email protected] Running title: Hypomethylating agents to enhance cancer vaccines for MDS Conflicts of Interest: The author has no conflicts of interest 1 Downloaded from clincancerres.aacrjournals.org on October 3, 2021. © 2017 American Association for Cancer Research. Author Manuscript Published OnlineFirst on December 28, 2017; DOI: 10.1158/1078-0432.CCR-17-2960 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Summary: The hypomethylating agent decitabine induces expression of the cancer testis antigen NY- ESO-1 in the myeloid cells of patients with myelodysplastic syndrome (MDS). MDS patients treated with decitabine and an NY-ESO-1 vaccine developed NY-ESO-1-specific T cell responses directed against their abnormal myeloid cells, raising hopes for combinatorial immunotherapy of this disease. In this issue of Clinical Cancer Research, Griffiths and colleagues conduct a phase I clinical trial in patients with myelodysplastic syndrome (MDS) of a combinatorial immunotherapy (Figure 1) comprising the hypomethylating agent decitabine plus a vaccine against the “cancer testis” antigen NY-ESO-1 (1). This strategy addresses a critical unmet need in cancer immunotherapy: the treatment of cancers with few available immunologic targets. The success of the immunologic checkpoint inhibitors (CIs) and of chimeric antigen receptor-modified T cells, or CAR T cells, has raised the level of enthusiasm for cancer immunotherapy to a fever pitch. -

Phenotype-Based Drug Screening Reveals Association Between Venetoclax Response and Differentiation Stage in Acute Myeloid Leukemia
Acute Myeloid Leukemia SUPPLEMENTARY APPENDIX Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia Heikki Kuusanmäki, 1,2 Aino-Maija Leppä, 1 Petri Pölönen, 3 Mika Kontro, 2 Olli Dufva, 2 Debashish Deb, 1 Bhagwan Yadav, 2 Oscar Brück, 2 Ashwini Kumar, 1 Hele Everaus, 4 Bjørn T. Gjertsen, 5 Merja Heinäniemi, 3 Kimmo Porkka, 2 Satu Mustjoki 2,6 and Caroline A. Heckman 1 1Institute for Molecular Medicine Finland, Helsinki Institute of Life Science, University of Helsinki, Helsinki; 2Hematology Research Unit, Helsinki University Hospital Comprehensive Cancer Center, Helsinki; 3Institute of Biomedicine, School of Medicine, University of Eastern Finland, Kuopio, Finland; 4Department of Hematology and Oncology, University of Tartu, Tartu, Estonia; 5Centre for Cancer Biomarkers, De - partment of Clinical Science, University of Bergen, Bergen, Norway and 6Translational Immunology Research Program and Department of Clinical Chemistry and Hematology, University of Helsinki, Helsinki, Finland ©2020 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2018.214882 Received: December 17, 2018. Accepted: July 8, 2019. Pre-published: July 11, 2019. Correspondence: CAROLINE A. HECKMAN - [email protected] HEIKKI KUUSANMÄKI - [email protected] Supplemental Material Phenotype-based drug screening reveals an association between venetoclax response and differentiation stage in acute myeloid leukemia Authors: Heikki Kuusanmäki1, 2, Aino-Maija