Eunethta Joint Action 3 WP4 VENETOCLAX with a HYPOMETHYLATING AGENT for the TREATMENT of ADULT PATIENTS with NEWLY DIAGNOSED
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

214120Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 214120Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number NDA 214120 Application Type Type 3 Priority or Standard Priority Submit Date 3/3/2020 Received Date 3/3/2020 PDUFA Goal Date 9/3/2020 Office/Division OOD/DHM1 Review Completion Date 9/1/2020 Applicant Celgene Corporation Established Name Azacitidine (Proposed) Trade Name Onureg Pharmacologic Class Nucleoside metabolic inhibitor Formulations Tablet (200 mg, 300 mg) (b) (4) Applicant Proposed Indication/Population Recommendation on Regulatory Regular approval Action Recommended Indication/ For continued treatment of adult patients with acute Population myeloid leukemia who achieved first complete remission (CR) or complete remission with incomplete blood count recovery (CRi) following intensive induction chemotherapy and are not able to complete intensive curative therapy. SNOMED CT for the Recommended 91861009 Indication/Population Recommended Dosing Regimen 300 mg orally daily on Days 1 through 14 of each 28-day cycle Reference ID: 4664570 NDA Multidisciplinary Review and Evaluation NDA 214120 Onureg (azacitidine tablets) TABLE OF CONTENTS TABLE OF CONTENTS ................................................................................................................................... 2 TABLE OF TABLES ....................................................................................................................................... -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
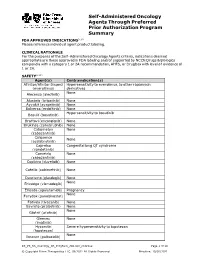
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Expression of Genes by Hypomethylating Agents
Wolff et al. Cell Communication and Signaling (2017) 15:13 DOI 10.1186/s12964-017-0168-z REVIEW Open Access The double-edged sword of (re)expression of genes by hypomethylating agents: from viral mimicry to exploitation as priming agents for targeted immune checkpoint modulation Florian Wolff1, Michael Leisch2, Richard Greil2,3,4, Angela Risch1,4 and Lisa Pleyer2,3,4* Abstract Hypomethylating agents (HMAs) have been widely used over the last decade, approved for use in myelodysplastic syndrome (MDS), chronic myelomonocytic leukemia (CMML) and acute myeloid leukemia (AML). The proposed central mechanism of action of HMAs, is the reversal of aberrant methylation in tumor cells, thus reactivating CpG-island promoters and leading to (re)expression of tumor suppressor genes. Recent investigations into the mode of action of azacitidine (AZA) and decitabine (DAC) have revealed new molecular mechanisms that impinge on tumor immunity via induction of an interferon response, through activation of endogenous retroviral elements (ERVs) that are normally epigenetically silenced. Although the global demethylation of DNA by HMAs can induce anti-tumor effects, it can also upregulate the expression of inhibitory immune checkpoint receptors and their ligands, resulting in secondary resistance to HMAs. Recent studies have, however, suggested that this could be exploited to prime or (re)sensitize tumors to immune checkpoint inhibitor therapies. In recent years, immune checkpoints have been targeted by novel therapies, with the aim of (re)activating the host immune system to specifically eliminate malignant cells. Antibodies blocking checkpoint receptors have been FDA-approved for some solid tumors and a plethora of clinical trials testing these and other checkpoint inhibitors are under way. -

Epigenetics in Clinical Practice: the Examples of Azacitidine and Decitabine in Myelodysplasia and Acute Myeloid Leukemia
Leukemia (2013) 27, 1803–1812 & 2013 Macmillan Publishers Limited All rights reserved 0887-6924/13 www.nature.com/leu SPOTLIGHT REVIEW Epigenetics in clinical practice: the examples of azacitidine and decitabine in myelodysplasia and acute myeloid leukemia EH Estey Randomized trials have clearly demonstrated that the hypomethylating agents azacitidine and decitabine are more effective than ‘best supportive care’(BSC) in reducing transfusion frequency in ‘low-risk’ myelodysplasia (MDS) and in prolonging survival compared with BSC or low-dose ara-C in ‘high-risk’ MDS or acute myeloid leukemia (AML) with 21–30% blasts. They also appear equivalent to conventional induction chemotherapy in AML with 420% blasts and as conditioning regimens before allogeneic transplant (hematopoietic cell transplant, HCT) in MDS. Although azacitidine or decitabine are thus the standard to which newer therapies should be compared, here we discuss whether the improvement they afford in overall survival is sufficient to warrant a designation as a standard in treating individual patients. We also discuss pre- and post-treatment covariates, including assays of methylation to predict response, different schedules of administration, combinations with other active agents and use in settings other than active disease, in particular post HCT. We note that rational development of this class of drugs awaits delineation of how much of their undoubted effect in fact results from hypomethylation and reactivation of gene expression. Leukemia (2013) 27, 1803–1812; doi:10.1038/leu.2013.173 -

Biological Heterogeneity of Chondrosarcoma: from (Epi) Genetics Through Stemness and Deregulated Signaling to Immunophenotype
cancers Review Biological Heterogeneity of Chondrosarcoma: From (Epi) Genetics through Stemness and Deregulated Signaling to Immunophenotype Agnieszka Zaj ˛ac 1 , Sylwia K. Król 2 , Piotr Rutkowski 1 and Anna M. Czarnecka 1,3,* 1 Department of Soft Tissue/Bone Sarcoma and Melanoma, Maria Sklodowska-Curie National Research Institute of Oncology, 02-781 Warsaw, Poland; [email protected] (A.Z.); [email protected] (P.R.) 2 Department of Molecular and Translational Oncology, Maria Sklodowska-Curie National Research Institute of Oncology, 02-781 Warsaw, Poland; [email protected] 3 Department of Experimental Pharmacology, Mossakowski Medical Research Centre, Polish Academy of Sciences, 02-176 Warsaw, Poland * Correspondence: [email protected] Simple Summary: Chondrosarcoma (ChS) is the second most frequently diagnosed malignant bone tumor of cartilaginous origin and is generally resistant to standard treatment options. In this paper, we aim to review the current state of the knowledge regarding ChS. We discuss the genetic, epigenetic, and molecular abnormalities underlying its substantial biological and clinical heterogeneity. This review summarizes the critical genetic and molecular drivers of ChS development and progression, contributing to its radio- and chemotherapy resistance. We describe genomic aberrations and point mutations, as well as epigenetic modifications and deregulated signal transduction pathways. We Citation: Zaj ˛ac,A.; Król, S.K.; provide an insight into the stem-like characteristics and immunophenotype of ChS. The paper also Rutkowski, P.; Czarnecka, A.M. outlines potential diagnostic and prognostic biomarkers of ChS and recently identified novel targets Biological Heterogeneity of for future pharmacological interventions in patients. Chondrosarcoma: From (Epi) Genetics through Stemness and Abstract: Deregulated Signaling to Chondrosarcoma (ChS) is a primary malignant bone tumor. -

BCBSVT Specialty Drug List Effective 2021.07.01.Xlsx
Effective Date: 07/01/2021 SPECIALTY DRUG LIST Revised Date: 05/07/2021 DOSAGE EXCLUDED ON NATIONAL DRUG CLASS DRUG NAME GENERIC NAME FORM PERFORMANCE FORMULARY ANEMIA ARANESP SOLN DARBEPOETIN ALFA SOLN INJ ANEMIA ARANESP SOSY DARBEPOETIN ALFA SOLN PREFILLED SYRINGE ANEMIA EPOGEN SOLN EPOETIN ALFA INJ X ANEMIA PROCRIT SOLN EPOETIN ALFA INJ X ANEMIA REBLOZYL SOLR LUSPATERCEPT-AAMT FOR SUBCUTANEOUS INJ ANEMIA RETACRIT SOLN EPOETIN ALFA-EPBX INJ ANTI-GOUT AGENT KRYSTEXXA SOLN PEGLOTICASE INJ (FOR IV INFUSION) ANTI-INFECTIVE PREVYMIS SOLN LETERMOVIR IV SOLN ANTI-INFECTIVE PREVYMIS TABS LETERMOVIR TAB ASTHMA CINQAIR SOLN RESLIZUMAB IV INFUSION SOLN ASTHMA FASENRA SOSY BENRALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE ASTHMA FASENRA PEN SOAJ BENRALIZUMAB SUBCUTANEOUS SOLN AUTO-INJECTOR ASTHMA NUCALA SOAJ MEPOLIZUMAB SUBCUTANEOUS SOLUTION AUTO-INJECTOR ASTHMA NUCALA SOLR MEPOLIZUMAB FOR INJ ASTHMA NUCALA SOSY MEPOLIZUMAB SUBCUTANEOUS SOLUTION PREF SYRINGE ASTHMA XOLAIR SOLR OMALIZUMAB FOR INJ ASTHMA XOLAIR SOSY OMALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE CARDIOVASCULAR VYNDAMAX CAPS TAFAMIDIS CAP CARDIOVASCULAR VYNDAQEL CAPS TAFAMIDIS MEGLUMINE (CARDIAC) CAP CENTRAL NERVOUS SYSTEM AGENTS AUSTEDO TABS DEUTETRABENAZINE TAB CENTRAL NERVOUS SYSTEM AGENTS ENSPRYNG SOSY SATRALIZUMAB-MWGE SUBCUTANEOUS SOLN PREF SYRINGE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ CAPS TASIMELTEON CAPSULE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ LQ SUSP TASIMELTEON ORAL SUSP CHEMOTHERAPY PROTECTANT AMIFOSTINE SOLR AMIFOSTINE CRYSTALLINE FOR INJ CHEMOTHERAPY PROTECTANT ELITEK -

Demethylation and Upregulation of an Oncogene Post Hypomethylating Treatment
medRxiv preprint doi: https://doi.org/10.1101/2020.07.21.20157776; this version posted July 26, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. Title: Demethylation and upregulation of an oncogene post hypomethylating treatment Authors: Yao-Chung Liu1,2,3,4°, Emiliano Fabiani5°, Junsu Kwon6°, Chong Gao1, Giulia Falconi5, Lia Valentini5, Carmelo Gurnari5, Yanjing V. Liu6, Adrianna I. Jones7, Junyu Yang1, Henry Yang6, Julie A. I. Thoms8, Ashwin Unnikrishnan9, John E. Pimanda8,9,10, Rongqing Pan11, Maria Teresa Voso5*, Daniel G. Tenen6,7*, Li Chai1* Affiliations: 1Department of Pathology, Brigham and Women's Hospital, Boston, MA 02115, USA 2Division of Hematology, Department of Medicine, Taipei Veterans General Hospital, Taipei, Taiwan 3Faculty of Medicine, School of Medicine, National Yang-Ming University, Taipei, Taiwan 4Program in Molecular Medicine, School of Life Science, National Yang-Ming University, Taipei, Taiwan 5Department of Biomedicine and Prevention, University of Tor Vergata, Rome, Italy 6Cancer Science Institute of Singapore, National University of Singapore, 117599, Singapore 7Harvard Stem Cell Institute, Harvard Medical School, Boston, MA 02115 USA 8School of Medical Sciences and Lowy Cancer Research Centre, Faculty of Medicine, UNSW Sydney, NSW 2052, Australia 9Prince of Wales Clinical School and Lowy Cancer Research Centre, Faculty of Medicine, UNSW Sydney, NSW 2052, Australia 10Department of Haematology, Prince of Wales Hospital, Randwick, NSW 2031, Australia 11 Department of Medical Oncology, Dana-Farber Cancer Institute, Boston, MA, 02115 °These authors contibute equally to this work *Co-corresponding authors: [email protected], [email protected], and [email protected] The authors have declared that no conflict of interest exists. -

Publication Final Minutes CHMP 16-19 September 2019
19 November 2019 EMA/CHMP/599241/2019 Inspections, Human Medicines Pharmacovigilance and Committees Division Committee for medicinal products for human use (CHMP) Final Minutes for the meeting on 16-19 September 2019 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in the minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, the minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on-going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2019. -

A Phase II Study of Omacetaxine (OM) in Patients with Intermediate-1 and Higher Risk Myelodysplastic Syndrome (MDS) Post Hypomethylating Agent (HMA) Failure 2013-0870
Protocol Page A Phase II Study of Omacetaxine (OM) in Patients with Intermediate-1 and Higher Risk Myelodysplastic Syndrome (MDS) post Hypomethylating Agent (HMA) Failure 2013-0870 Core Protocol Information Short Title Omacetaxine in Patients with Intermediate-1 and Higher Risk MDS post HMA Failure Study Chair: Elias Jabbour Additional Contact: Jhinelle L. Graham Vicky H. Zoeller Leukemia Protocol Review Group Additional Memo Recipients: Recipients List OPR Recipients (for OPR use only) None Study Staff Recipients None Department: Leukemia Phone: 713-792-4764 Unit: 0428 Full Title: A Phase II Study of Omacetaxine (OM) in Patients with Intermediate-1 and Higher Risk Myelodysplastic Syndrome (MDS) post Hypomethylating Agent (HMA) Failure Protocol Type: Standard Protocol Protocol Phase: Phase II Version Status: Activated -- Closed to new patient entry as of 08/05/2018 Version: 08 Document Status: Saved as "Final" Submitted by: Vicky H. Zoeller--9/11/2017 12:24:33 PM OPR Action: Accepted by: Margaret Okoloise -- 9/14/2017 12:09:50 PM Which Committee will review this protocol? The Clinical Research Committee - (CRC) Protocol Body 2013-0870 March 6, 2017 1 A Phase II Study of Omacetaxine (OM) in Patients with Intermediate-1 and Higher Risk Myelodysplastic Syndrome (MDS) post Hypomethylating Agent (HMA) Failure 2013-0870 March 6, 2017 2 Table of Contents 1.0 Objectives .................................................................................................. 3 2.0 Background .............................................................................................. -

Immunotherapy of MDS: You Can Run, but You Can’T Hide
Author Manuscript Published OnlineFirst on December 28, 2017; DOI: 10.1158/1078-0432.CCR-17-2960 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Immunotherapy of MDS: you can run, but you can’t hide Ephraim Joseph Fuchs, MD, MBA Division of Hematologic Malignancies, Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Baltimore, MD, USA e-mail: [email protected] Running title: Hypomethylating agents to enhance cancer vaccines for MDS Conflicts of Interest: The author has no conflicts of interest 1 Downloaded from clincancerres.aacrjournals.org on October 3, 2021. © 2017 American Association for Cancer Research. Author Manuscript Published OnlineFirst on December 28, 2017; DOI: 10.1158/1078-0432.CCR-17-2960 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Summary: The hypomethylating agent decitabine induces expression of the cancer testis antigen NY- ESO-1 in the myeloid cells of patients with myelodysplastic syndrome (MDS). MDS patients treated with decitabine and an NY-ESO-1 vaccine developed NY-ESO-1-specific T cell responses directed against their abnormal myeloid cells, raising hopes for combinatorial immunotherapy of this disease. In this issue of Clinical Cancer Research, Griffiths and colleagues conduct a phase I clinical trial in patients with myelodysplastic syndrome (MDS) of a combinatorial immunotherapy (Figure 1) comprising the hypomethylating agent decitabine plus a vaccine against the “cancer testis” antigen NY-ESO-1 (1). This strategy addresses a critical unmet need in cancer immunotherapy: the treatment of cancers with few available immunologic targets. The success of the immunologic checkpoint inhibitors (CIs) and of chimeric antigen receptor-modified T cells, or CAR T cells, has raised the level of enthusiasm for cancer immunotherapy to a fever pitch. -
Recognizing Toxicites of Oral Oncolytics in the Management of Hematologic Malignancies
Recognizing Toxicites of Oral Oncolytics in the Management of Hematologic Malignancies David Reeves, PharmD, BCOP Associate Professor of Pharmacy Practice Butler University Clinical Pharmacy Specialist – Hematology/Oncology Franciscan Health Indianapolis Objectives & Disclosure Identify common adverse effects associated with oral oncolytic therapies utilized to treat hematologic malignancies Propose a strategy to manage a patient experiencing an adverse effect while receiving an oral oncolytic agent Disclosure – I have no conflicts of interest to disclose – All materials and content presented do not infringe or violate any copyright, trademark, patent or intellectual property rights of any person or entity, nor do they promote or endorse any product, service, or device which may or is at the time of the program not approved by any governing agency Common Toxicities Rash/Dermatologic Nausea/Vomiting Diarrhea Cardiac toxicities toxicities Electrolyte Infection Myelosuppression Hepatotoxicity abnormalities Tumor lysis Fatigue Hypothyroidism Pneumonitis syndrome Human Kinome Nature Immunology. 2009;10:356-60. PeerJ. 2013;1:e126. Impact of Oral Oncolytic Toxicity ESAS-r Symptom Score (%) Mild Moderate Severe Symptom (0-3) (4-6) (7-10) Eight oncology practices in Pain 80 15 5 Michigan Tiredness 65 21 14 Drowsiness 75 16 9 • Investigation of patient-reported Nausea 92 6 2 outcomes Appetite 79 13 8 • Evaluate symptom burden of patients Shortness of Breath 87 9 3 prescribed oral oncolytics before each Depression 86 11 3 outpatient visit Anxiety 87 10 3 Well-being 66 21 13 1,235 ESAS-r surveys collected Constipation 87 10 3 Diarrhea 92 5 3 Tingling/numbness 81 12 6 • Symptoms categorized as mild, Mouth sores 96 3 1 moderate or severe ESA-r: revised Edmonton Symptom Assessment System J Oncol Pract. -

Oncology Orals Solid Tumors
Oncology Oral Medications Solid Tumors Enrollment Form Fax Referral To: 1-800-323-2445 Phone: 1-800-237-2767 Email Referral To: [email protected] Six Simple Steps to Submitting a Referral 1 PATIENT INFORMATION (Complete or include demographic sheet) Patient Name: _______________________________________ Address: ____________________________ City, State, ZIP Code: ___________________________________ Preferred Contact Methods: Phone (primary # provided below) Text (cell # provided below) Email (email provided below) Note: Carrier charges may apply. If unable to contact via text or email, Specialty Pharmacy will attempt to contact by phone. Primary Phone: ____________________________ Alternate Phone: ________________________________ Primary Language: _________________________________ DOB: __________________ Gender: Male Female Email: __________________________________ Last Four of SSN: ________ 2 PRESCRIBER INFORMATION Prescriber’s Name: _________________________________________________________________ State License #: _____________________________________ NPI #: _____________________ DEA #: _____________________ Group or Hospital: _______________________________________________________________ Address: ______________________________________________ City, State, ZIP Code: ______________________________________________________________ Phone: ______________________ Fax: ______________________ Contact Person: ________________________ Contact’s Phone: _______________________ 3 INSURANCE INFORMATION Please fax copy of prescription