Current Challenges and Unmet Medical Needs in Myelodysplastic Syndromes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
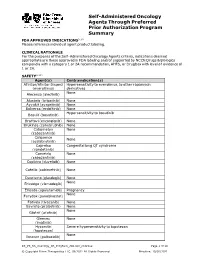
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Us Anti-Doping Agency
2019U.S. ANTI-DOPING AGENCY WALLET CARDEXAMPLES OF PROHIBITED AND PERMITTED SUBSTANCES AND METHODS Effective Jan. 1 – Dec. 31, 2019 CATEGORIES OF SUBSTANCES PROHIBITED AT ALL TIMES (IN AND OUT-OF-COMPETITION) • Non-Approved Substances: investigational drugs and pharmaceuticals with no approval by a governmental regulatory health authority for human therapeutic use. • Anabolic Agents: androstenediol, androstenedione, bolasterone, boldenone, clenbuterol, danazol, desoxymethyltestosterone (madol), dehydrochlormethyltestosterone (DHCMT), Prasterone (dehydroepiandrosterone, DHEA , Intrarosa) and its prohormones, drostanolone, epitestosterone, methasterone, methyl-1-testosterone, methyltestosterone (Covaryx, EEMT, Est Estrogens-methyltest DS, Methitest), nandrolone, oxandrolone, prostanozol, Selective Androgen Receptor Modulators (enobosarm, (ostarine, MK-2866), andarine, LGD-4033, RAD-140). stanozolol, testosterone and its metabolites or isomers (Androgel), THG, tibolone, trenbolone, zeranol, zilpaterol, and similar substances. • Beta-2 Agonists: All selective and non-selective beta-2 agonists, including all optical isomers, are prohibited. Most inhaled beta-2 agonists are prohibited, including arformoterol (Brovana), fenoterol, higenamine (norcoclaurine, Tinospora crispa), indacaterol (Arcapta), levalbuterol (Xopenex), metaproternol (Alupent), orciprenaline, olodaterol (Striverdi), pirbuterol (Maxair), terbutaline (Brethaire), vilanterol (Breo). The only exceptions are albuterol, formoterol, and salmeterol by a metered-dose inhaler when used -

BCBSVT Specialty Drug List Effective 2021.07.01.Xlsx
Effective Date: 07/01/2021 SPECIALTY DRUG LIST Revised Date: 05/07/2021 DOSAGE EXCLUDED ON NATIONAL DRUG CLASS DRUG NAME GENERIC NAME FORM PERFORMANCE FORMULARY ANEMIA ARANESP SOLN DARBEPOETIN ALFA SOLN INJ ANEMIA ARANESP SOSY DARBEPOETIN ALFA SOLN PREFILLED SYRINGE ANEMIA EPOGEN SOLN EPOETIN ALFA INJ X ANEMIA PROCRIT SOLN EPOETIN ALFA INJ X ANEMIA REBLOZYL SOLR LUSPATERCEPT-AAMT FOR SUBCUTANEOUS INJ ANEMIA RETACRIT SOLN EPOETIN ALFA-EPBX INJ ANTI-GOUT AGENT KRYSTEXXA SOLN PEGLOTICASE INJ (FOR IV INFUSION) ANTI-INFECTIVE PREVYMIS SOLN LETERMOVIR IV SOLN ANTI-INFECTIVE PREVYMIS TABS LETERMOVIR TAB ASTHMA CINQAIR SOLN RESLIZUMAB IV INFUSION SOLN ASTHMA FASENRA SOSY BENRALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE ASTHMA FASENRA PEN SOAJ BENRALIZUMAB SUBCUTANEOUS SOLN AUTO-INJECTOR ASTHMA NUCALA SOAJ MEPOLIZUMAB SUBCUTANEOUS SOLUTION AUTO-INJECTOR ASTHMA NUCALA SOLR MEPOLIZUMAB FOR INJ ASTHMA NUCALA SOSY MEPOLIZUMAB SUBCUTANEOUS SOLUTION PREF SYRINGE ASTHMA XOLAIR SOLR OMALIZUMAB FOR INJ ASTHMA XOLAIR SOSY OMALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE CARDIOVASCULAR VYNDAMAX CAPS TAFAMIDIS CAP CARDIOVASCULAR VYNDAQEL CAPS TAFAMIDIS MEGLUMINE (CARDIAC) CAP CENTRAL NERVOUS SYSTEM AGENTS AUSTEDO TABS DEUTETRABENAZINE TAB CENTRAL NERVOUS SYSTEM AGENTS ENSPRYNG SOSY SATRALIZUMAB-MWGE SUBCUTANEOUS SOLN PREF SYRINGE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ CAPS TASIMELTEON CAPSULE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ LQ SUSP TASIMELTEON ORAL SUSP CHEMOTHERAPY PROTECTANT AMIFOSTINE SOLR AMIFOSTINE CRYSTALLINE FOR INJ CHEMOTHERAPY PROTECTANT ELITEK -

The Influence of Inflammation on Anemia in CKD Patients
International Journal of Molecular Sciences Review The Influence of Inflammation on Anemia in CKD Patients Anna Gluba-Brzózka 1,* , Beata Franczyk 1, Robert Olszewski 2 and Jacek Rysz 1 1 Department of Nephrology, Hypertension and Family Medicine, Medical University of Lodz, 90-549 Lodz, Poland; [email protected] (B.F.); [email protected] (J.R.) 2 Department of Geriatrics, National Institute of Geriatrics Rheumatology and Rehabilitation and Department of Ultrasound, Institute of Fundamental Technological Research, Polish Academy of Sciences, Warsaw, Poland (IPPT PAN), 02-106 Warsaw, Poland; [email protected] * Correspondence: [email protected] Received: 18 November 2019; Accepted: 19 January 2020; Published: 22 January 2020 Abstract: Anemia is frequently observed in the course of chronic kidney disease (CKD) and it is associated with diminishing the quality of a patient’s life. It also enhances morbidity and mortality and hastens the CKD progression rate. Patients with CKD frequently suffer from a chronic inflammatory state which is related to a vast range of underlying factors. The results of studies have demonstrated that persistent inflammation may contribute to the variability in Hb levels and hyporesponsiveness to erythropoietin stimulating agents (ESA), which are frequently observed in CKD patients. The understanding of the impact of inflammatory cytokines on erythropoietin production and hepcidin synthesis will enable one to unravel the net of interactions of multiple factors involved in the pathogenesis of the anemia of chronic disease. It seems that anti-cytokine and anti-oxidative treatment strategies may be the future of pharmacological interventions aiming at the treatment of inflammation-associated hyporesponsiveness to ESA. -

Analytical Approaches in Human Sports Drug Testing
Received: 13 November 2018 Accepted: 18 November 2018 DOI: 10.1002/dta.2549 ANNUAL BANNED‐ SUBSTANCE REVIEW Annual banned‐substance review: Analytical approaches in human sports drug testing Mario Thevis1,2 | Tiia Kuuranne3 | Hans Geyer1,2 1 Center for Preventive Doping Research ‐ Institute of Biochemistry, German Sport Abstract University Cologne, Cologne, Germany A number of high profile revelations concerning anti‐doping rule violations over the 2 European Monitoring Center for Emerging past 12 months have outlined the importance of tackling prevailing challenges and Doping Agents, Cologne, Germany reducing the limitations of the current anti‐doping system. At this time, the necessity 3 Swiss Laboratory for Doping Analyses, University Center of Legal Medicine, Genève to enhance, expand, and improve analytical test methods in response to the sub- and Lausanne, Centre Hospitalier Universitaire stances outlined in the World Anti‐Doping Agency (WADA) Prohibited List represents Vaudois and University of Lausanne, Epalinges, Switzerland an increasingly crucial task for modern sports drug testing programs. The ability to Correspondence improve analytical testing methods often relies on the expedient application of novel Mario Thevis, Institute of Biochemistry ‐ Center for Preventive Doping Research, information regarding superior target analytes for sports drug testing assays, drug German Sport University Cologne, Am elimination profiles, and alternative sample matrices, together with recent advances Sportpark Müngersdorf 6, 50933 Cologne, Germany. in instrumental developments. This annual banned‐substance review evaluates litera- Email: thevis@dshs‐koeln.de ture published between October 2017 and September 2018 offering an in‐depth Funding information evaluation of developments in these arenas and their potential application to Federal Ministry of the Interior, Federal Republic of Germany; Manfred‐Donike‐Insti- substances reported in WADA's 2018 Prohibited List. -

Publication Final Minutes CHMP 16-19 September 2019
19 November 2019 EMA/CHMP/599241/2019 Inspections, Human Medicines Pharmacovigilance and Committees Division Committee for medicinal products for human use (CHMP) Final Minutes for the meeting on 16-19 September 2019 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in the minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, the minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on-going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2019. -

2020 Medicaid Preapproval Criteria
2020 Medicaid Preapproval Criteria ABILIFY MAINTENA ................................................................................................................................................................ 10 ACTHAR HP ............................................................................................................................................................................ 11 ACTIMMUNE ......................................................................................................................................................................... 13 ADAGEN & REVCOVI ............................................................................................................................................................. 14 ADCIRCA ................................................................................................................................................................................ 15 ADEMPAS .............................................................................................................................................................................. 16 AFINITOR ............................................................................................................................................................................... 18 AFINITOR DISPERZ ................................................................................................................................................................. 19 ALDURAZYME ....................................................................................................................................................................... -
Presentation Title
The COMMANDS trial: a phase 3 study of the efficacy and safety of luspatercept versus epoetin alfa for the treatment of anemia due to Revised International Prognostic Scoring System Very Low-, Low-, or Intermediate-risk myelodysplastic syndromes in erythropoiesis stimulating agent-naive patients who require red blood cell transfusions Matteo Della Porta,1,2 Uwe Platzbecker,3 Valeria Santini,4 Guillermo Garcia-Manero,5 Rami S. Komrokji,6 Rodrigo Ito,7 Pierre Fenaux8 1Cancer Center IRCCS Humanitas Research Hospital, Milan, Italy; 2Department of Biomedical Sciences, Humanitas University, Milan, Italy; 3Medical Clinic and Policlinic 1, Hematology and Cellular Therapy, University Hospital Leipzig, Leipzig, Germany; 4Azienda Ospedaliero-Universitaria Careggi, University of Florence, Florence, Italy; 5Department of Leukemia, University of Texas MD Anderson Cancer Center, Houston, TX; 6Moffitt Cancer Center, Tampa, FL; 7Bristol Myers Squibb, Princeton, NJ; 8Service d'Hématologie Séniors, Hôpital Saint-Louis, Université Paris 7, Paris, France Presentation 2198 Presenting author disclosures M.D.P.: no conflicts of interest to disclose. 2 Introduction and objectives Introduction • Studies of epoetin alfa and darbepoetin alfa have demonstrated efficacy among patients with LR-MDS, but the patient population in which a clinically significant effect is observed may be limited1,2 • Luspatercept, a first-in-class erythroid maturation agent with a mechanism of action distinct from ESAs,3 is approved by the US FDA for the treatment of anemia failing an -
Recognizing Toxicites of Oral Oncolytics in the Management of Hematologic Malignancies
Recognizing Toxicites of Oral Oncolytics in the Management of Hematologic Malignancies David Reeves, PharmD, BCOP Associate Professor of Pharmacy Practice Butler University Clinical Pharmacy Specialist – Hematology/Oncology Franciscan Health Indianapolis Objectives & Disclosure Identify common adverse effects associated with oral oncolytic therapies utilized to treat hematologic malignancies Propose a strategy to manage a patient experiencing an adverse effect while receiving an oral oncolytic agent Disclosure – I have no conflicts of interest to disclose – All materials and content presented do not infringe or violate any copyright, trademark, patent or intellectual property rights of any person or entity, nor do they promote or endorse any product, service, or device which may or is at the time of the program not approved by any governing agency Common Toxicities Rash/Dermatologic Nausea/Vomiting Diarrhea Cardiac toxicities toxicities Electrolyte Infection Myelosuppression Hepatotoxicity abnormalities Tumor lysis Fatigue Hypothyroidism Pneumonitis syndrome Human Kinome Nature Immunology. 2009;10:356-60. PeerJ. 2013;1:e126. Impact of Oral Oncolytic Toxicity ESAS-r Symptom Score (%) Mild Moderate Severe Symptom (0-3) (4-6) (7-10) Eight oncology practices in Pain 80 15 5 Michigan Tiredness 65 21 14 Drowsiness 75 16 9 • Investigation of patient-reported Nausea 92 6 2 outcomes Appetite 79 13 8 • Evaluate symptom burden of patients Shortness of Breath 87 9 3 prescribed oral oncolytics before each Depression 86 11 3 outpatient visit Anxiety 87 10 3 Well-being 66 21 13 1,235 ESAS-r surveys collected Constipation 87 10 3 Diarrhea 92 5 3 Tingling/numbness 81 12 6 • Symptoms categorized as mild, Mouth sores 96 3 1 moderate or severe ESA-r: revised Edmonton Symptom Assessment System J Oncol Pract. -

Oncology Orals Solid Tumors
Oncology Oral Medications Solid Tumors Enrollment Form Fax Referral To: 1-800-323-2445 Phone: 1-800-237-2767 Email Referral To: [email protected] Six Simple Steps to Submitting a Referral 1 PATIENT INFORMATION (Complete or include demographic sheet) Patient Name: _______________________________________ Address: ____________________________ City, State, ZIP Code: ___________________________________ Preferred Contact Methods: Phone (primary # provided below) Text (cell # provided below) Email (email provided below) Note: Carrier charges may apply. If unable to contact via text or email, Specialty Pharmacy will attempt to contact by phone. Primary Phone: ____________________________ Alternate Phone: ________________________________ Primary Language: _________________________________ DOB: __________________ Gender: Male Female Email: __________________________________ Last Four of SSN: ________ 2 PRESCRIBER INFORMATION Prescriber’s Name: _________________________________________________________________ State License #: _____________________________________ NPI #: _____________________ DEA #: _____________________ Group or Hospital: _______________________________________________________________ Address: ______________________________________________ City, State, ZIP Code: ______________________________________________________________ Phone: ______________________ Fax: ______________________ Contact Person: ________________________ Contact’s Phone: _______________________ 3 INSURANCE INFORMATION Please fax copy of prescription -

Advances in the Treatment of Acute Myeloid Leukemia: New Drugs and New Challenges
Published OnlineFirst February 3, 2020; DOI: 10.1158/2159-8290.CD-19-1011 REVIEW Advances in the Treatment of Acute Myeloid Leukemia: New Drugs and New Challenges Nicholas J. Short , Marina Konopleva , Tapan M. Kadia , Gautam Borthakur , Farhad Ravandi , Courtney D. DiNardo , and Naval Daver ABSTRACT The therapeutic armamentarium of acute myeloid leukemia (AML) has rapidly expanded in the past few years, driven largely by translational research into its genomic landscape and an improved understanding of mechanisms of resistance to conventional thera- pies. However, primary and secondary drug resistance remains a substantial problem for most patients. Research into the mechanisms of resistance to these new agents is informing the development of the next class of AML drugs and the design of combination regimens aimed at optimally exploiting thera- peutic vulnerabilities, with the ultimate goal of eradicating all subclones of the disease and increasing cure rates in AML. Signifi cance: AML is a heterogeneous disease, characterized by a broad spectrum of molecular altera- tions that infl uence clinical outcomes and also provide potential targets for drug development. This review discusses the current and emerging therapeutic landscape of AML, highlighting novel classes of drugs and how our expanding knowledge of mechanisms of resistance are informing future therapies and providing new opportunities for effective combination strategies. INTRODUCTION importance of the apoptotic machinery in chemotherapy resistance and AML propagation has also led to the devel- Driven by intense basic and translational research, the opment of apoptosis-inducing therapies that appear to be past 10 to 15 years have greatly improved our understanding effi cacious irrespective of the presence or absence of targeta- of the pathobiology and genetic diversity of acute myeloid ble genetic mutations ( 6, 7 ). -

Refractory Acute Myeloid Leukemia
TRANSLATIONAL AND BJBMS REVIEW ARTICLE CLINICAL RESEARCH Recent advances of targeted therapy in relapsed/ refractory acute myeloid leukemia Jiale Ma1,2, Zheng Ge1* ABSTRACT Despite advances in the understanding of disease pathobiology, treatment for relapsed or refractory acute myeloid leukemia (R/R AML) remains challenging. The prognosis of R/R AML remains extremely poor despite chemotherapy and bone marrow transplants. Discoveries on recurrent and novel genetic mutations, such as FLT3-ITD and IDH1/IDH2, critical signaling pathways, and unique molecular markers expressed on the surface of leukemic cells have been under investigation for the management of R/R AML. Other than monoclonal antibod- ies, diabodies, and triabodies are new targeted therapies developed in recent years and will be the new direction of immunotherapy. Targeted agents combined intensive regimens can be viable options for salvage therapy and as bridges to allogeneic transplant. Future directions will focus on novel, efficient and targeted combinations, low-toxicity maintenance, and individualized precision strategies. Here, we review the major recent advances of targeted therapies in the treatment of R/R AML. KEYWORDS: Relapsed/refractory acute myeloid leukemia; targeted therapy; novel genetic mutations; immunotherapy INTRODUCTION idarubicin, and granulocyte colony-stimulating factor) [3,4], CLAG (cladribine, cytarabine, and G-CSF) [5,6], and MEC Acute myeloid leukemia (AML) is a clinically and (mitoxantrone, etoposide, and cytarabine). In patients fit for biologically heterogeneous disease, characterized by clonal intensive chemotherapy, the complete remission (CR) rates proliferation of myeloid precursors. Acquired somatic muta- range from 44% to 59.4% and the overall survival (OS) ranges tions accumulated in hematopoietic stem and progenitor from 6.2 to 8.7 months [7].