Split Fill Program Drug List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
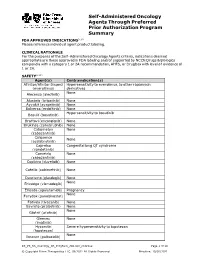
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

BCBSVT Specialty Drug List Effective 2021.07.01.Xlsx
Effective Date: 07/01/2021 SPECIALTY DRUG LIST Revised Date: 05/07/2021 DOSAGE EXCLUDED ON NATIONAL DRUG CLASS DRUG NAME GENERIC NAME FORM PERFORMANCE FORMULARY ANEMIA ARANESP SOLN DARBEPOETIN ALFA SOLN INJ ANEMIA ARANESP SOSY DARBEPOETIN ALFA SOLN PREFILLED SYRINGE ANEMIA EPOGEN SOLN EPOETIN ALFA INJ X ANEMIA PROCRIT SOLN EPOETIN ALFA INJ X ANEMIA REBLOZYL SOLR LUSPATERCEPT-AAMT FOR SUBCUTANEOUS INJ ANEMIA RETACRIT SOLN EPOETIN ALFA-EPBX INJ ANTI-GOUT AGENT KRYSTEXXA SOLN PEGLOTICASE INJ (FOR IV INFUSION) ANTI-INFECTIVE PREVYMIS SOLN LETERMOVIR IV SOLN ANTI-INFECTIVE PREVYMIS TABS LETERMOVIR TAB ASTHMA CINQAIR SOLN RESLIZUMAB IV INFUSION SOLN ASTHMA FASENRA SOSY BENRALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE ASTHMA FASENRA PEN SOAJ BENRALIZUMAB SUBCUTANEOUS SOLN AUTO-INJECTOR ASTHMA NUCALA SOAJ MEPOLIZUMAB SUBCUTANEOUS SOLUTION AUTO-INJECTOR ASTHMA NUCALA SOLR MEPOLIZUMAB FOR INJ ASTHMA NUCALA SOSY MEPOLIZUMAB SUBCUTANEOUS SOLUTION PREF SYRINGE ASTHMA XOLAIR SOLR OMALIZUMAB FOR INJ ASTHMA XOLAIR SOSY OMALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE CARDIOVASCULAR VYNDAMAX CAPS TAFAMIDIS CAP CARDIOVASCULAR VYNDAQEL CAPS TAFAMIDIS MEGLUMINE (CARDIAC) CAP CENTRAL NERVOUS SYSTEM AGENTS AUSTEDO TABS DEUTETRABENAZINE TAB CENTRAL NERVOUS SYSTEM AGENTS ENSPRYNG SOSY SATRALIZUMAB-MWGE SUBCUTANEOUS SOLN PREF SYRINGE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ CAPS TASIMELTEON CAPSULE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ LQ SUSP TASIMELTEON ORAL SUSP CHEMOTHERAPY PROTECTANT AMIFOSTINE SOLR AMIFOSTINE CRYSTALLINE FOR INJ CHEMOTHERAPY PROTECTANT ELITEK -

Publication Final Minutes CHMP 16-19 September 2019
19 November 2019 EMA/CHMP/599241/2019 Inspections, Human Medicines Pharmacovigilance and Committees Division Committee for medicinal products for human use (CHMP) Final Minutes for the meeting on 16-19 September 2019 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in the minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, the minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on-going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2019. -
Recognizing Toxicites of Oral Oncolytics in the Management of Hematologic Malignancies
Recognizing Toxicites of Oral Oncolytics in the Management of Hematologic Malignancies David Reeves, PharmD, BCOP Associate Professor of Pharmacy Practice Butler University Clinical Pharmacy Specialist – Hematology/Oncology Franciscan Health Indianapolis Objectives & Disclosure Identify common adverse effects associated with oral oncolytic therapies utilized to treat hematologic malignancies Propose a strategy to manage a patient experiencing an adverse effect while receiving an oral oncolytic agent Disclosure – I have no conflicts of interest to disclose – All materials and content presented do not infringe or violate any copyright, trademark, patent or intellectual property rights of any person or entity, nor do they promote or endorse any product, service, or device which may or is at the time of the program not approved by any governing agency Common Toxicities Rash/Dermatologic Nausea/Vomiting Diarrhea Cardiac toxicities toxicities Electrolyte Infection Myelosuppression Hepatotoxicity abnormalities Tumor lysis Fatigue Hypothyroidism Pneumonitis syndrome Human Kinome Nature Immunology. 2009;10:356-60. PeerJ. 2013;1:e126. Impact of Oral Oncolytic Toxicity ESAS-r Symptom Score (%) Mild Moderate Severe Symptom (0-3) (4-6) (7-10) Eight oncology practices in Pain 80 15 5 Michigan Tiredness 65 21 14 Drowsiness 75 16 9 • Investigation of patient-reported Nausea 92 6 2 outcomes Appetite 79 13 8 • Evaluate symptom burden of patients Shortness of Breath 87 9 3 prescribed oral oncolytics before each Depression 86 11 3 outpatient visit Anxiety 87 10 3 Well-being 66 21 13 1,235 ESAS-r surveys collected Constipation 87 10 3 Diarrhea 92 5 3 Tingling/numbness 81 12 6 • Symptoms categorized as mild, Mouth sores 96 3 1 moderate or severe ESA-r: revised Edmonton Symptom Assessment System J Oncol Pract. -

Oncology Orals Solid Tumors
Oncology Oral Medications Solid Tumors Enrollment Form Fax Referral To: 1-800-323-2445 Phone: 1-800-237-2767 Email Referral To: [email protected] Six Simple Steps to Submitting a Referral 1 PATIENT INFORMATION (Complete or include demographic sheet) Patient Name: _______________________________________ Address: ____________________________ City, State, ZIP Code: ___________________________________ Preferred Contact Methods: Phone (primary # provided below) Text (cell # provided below) Email (email provided below) Note: Carrier charges may apply. If unable to contact via text or email, Specialty Pharmacy will attempt to contact by phone. Primary Phone: ____________________________ Alternate Phone: ________________________________ Primary Language: _________________________________ DOB: __________________ Gender: Male Female Email: __________________________________ Last Four of SSN: ________ 2 PRESCRIBER INFORMATION Prescriber’s Name: _________________________________________________________________ State License #: _____________________________________ NPI #: _____________________ DEA #: _____________________ Group or Hospital: _______________________________________________________________ Address: ______________________________________________ City, State, ZIP Code: ______________________________________________________________ Phone: ______________________ Fax: ______________________ Contact Person: ________________________ Contact’s Phone: _______________________ 3 INSURANCE INFORMATION Please fax copy of prescription -

Advances in the Treatment of Acute Myeloid Leukemia: New Drugs and New Challenges
Published OnlineFirst February 3, 2020; DOI: 10.1158/2159-8290.CD-19-1011 REVIEW Advances in the Treatment of Acute Myeloid Leukemia: New Drugs and New Challenges Nicholas J. Short , Marina Konopleva , Tapan M. Kadia , Gautam Borthakur , Farhad Ravandi , Courtney D. DiNardo , and Naval Daver ABSTRACT The therapeutic armamentarium of acute myeloid leukemia (AML) has rapidly expanded in the past few years, driven largely by translational research into its genomic landscape and an improved understanding of mechanisms of resistance to conventional thera- pies. However, primary and secondary drug resistance remains a substantial problem for most patients. Research into the mechanisms of resistance to these new agents is informing the development of the next class of AML drugs and the design of combination regimens aimed at optimally exploiting thera- peutic vulnerabilities, with the ultimate goal of eradicating all subclones of the disease and increasing cure rates in AML. Signifi cance: AML is a heterogeneous disease, characterized by a broad spectrum of molecular altera- tions that infl uence clinical outcomes and also provide potential targets for drug development. This review discusses the current and emerging therapeutic landscape of AML, highlighting novel classes of drugs and how our expanding knowledge of mechanisms of resistance are informing future therapies and providing new opportunities for effective combination strategies. INTRODUCTION importance of the apoptotic machinery in chemotherapy resistance and AML propagation has also led to the devel- Driven by intense basic and translational research, the opment of apoptosis-inducing therapies that appear to be past 10 to 15 years have greatly improved our understanding effi cacious irrespective of the presence or absence of targeta- of the pathobiology and genetic diversity of acute myeloid ble genetic mutations ( 6, 7 ). -

Refractory Acute Myeloid Leukemia
TRANSLATIONAL AND BJBMS REVIEW ARTICLE CLINICAL RESEARCH Recent advances of targeted therapy in relapsed/ refractory acute myeloid leukemia Jiale Ma1,2, Zheng Ge1* ABSTRACT Despite advances in the understanding of disease pathobiology, treatment for relapsed or refractory acute myeloid leukemia (R/R AML) remains challenging. The prognosis of R/R AML remains extremely poor despite chemotherapy and bone marrow transplants. Discoveries on recurrent and novel genetic mutations, such as FLT3-ITD and IDH1/IDH2, critical signaling pathways, and unique molecular markers expressed on the surface of leukemic cells have been under investigation for the management of R/R AML. Other than monoclonal antibod- ies, diabodies, and triabodies are new targeted therapies developed in recent years and will be the new direction of immunotherapy. Targeted agents combined intensive regimens can be viable options for salvage therapy and as bridges to allogeneic transplant. Future directions will focus on novel, efficient and targeted combinations, low-toxicity maintenance, and individualized precision strategies. Here, we review the major recent advances of targeted therapies in the treatment of R/R AML. KEYWORDS: Relapsed/refractory acute myeloid leukemia; targeted therapy; novel genetic mutations; immunotherapy INTRODUCTION idarubicin, and granulocyte colony-stimulating factor) [3,4], CLAG (cladribine, cytarabine, and G-CSF) [5,6], and MEC Acute myeloid leukemia (AML) is a clinically and (mitoxantrone, etoposide, and cytarabine). In patients fit for biologically heterogeneous disease, characterized by clonal intensive chemotherapy, the complete remission (CR) rates proliferation of myeloid precursors. Acquired somatic muta- range from 44% to 59.4% and the overall survival (OS) ranges tions accumulated in hematopoietic stem and progenitor from 6.2 to 8.7 months [7]. -

Phase 1/2 Trial of Glasdegib in Patients with Primary Or Secondary Myelofibrosis Previously Treated with Ruxolitinib
Leukemia Research 79 (2019) 38–44 Contents lists available at ScienceDirect Leukemia Research journal homepage: www.elsevier.com/locate/leukres Research paper Phase 1/2 trial of glasdegib in patients with primary or secondary myelofibrosis previously treated with ruxolitinib T ⁎ Aaron T. Gerdsa, , Tetsuzo Tauchib, Ellen Ritchiec, Michael Deiningerd, Catriona Jamiesone, Ruben Mesaf, Mark Heaneyg, Norio Komatsuh, Hironobu Minamii, Yun Suj, Naveed Shaikk, Xiaoxi Zhangl, Christine DiRienzom, Mirjana Zeremskin, Geoffrey Chano, Moshe Talpazp a Leukemia and Myeloid Disorders Program, Department of Hematology and Medical Oncology, Taussig Cancer Institute, 9500 Euclid Avenue, Cleveland, OH 44195, USA b Tokyo Medical University, 6-1-1 Shinjuku, Shinjuku-ku, Tokyo 160-8402, Japan c Weill Cornell Medical College of Cornell University, 1300 York Ave, New York, NY 10065, USA d Huntsman Cancer Institute, University of Utah, 2000 Circle of Hope Dr, Salt Lake City, UT 84112, USA e Moores Cancer Center, University of California, San Diego, 3855 Health Sciences Dr, La Jolla, CA 92093, USA f UT Health San Antonio Cancer Center, 7979 Wurzbach Rd, San Antonio, TX 78229, USA g Columbia University Medical Center, 630 West 168th St, New York, NY 10032, USA h Juntendo University School of Medicine, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan i Division of Medical Oncology /Hematology, Department of Medicine, Kobe University Hospital and Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe 650-0017, Japan j Pfizer Inc, 235 East 42nd St, New York, NY 10017, USA k Pfizer Inc, 10555 Science Center Drive, San Diego, CA, 92121 USA l Pfizer Inc, 235 East 42nd St, New York, NY 10017, USA m Pfizer Inc, 235 East 42nd St, New York, NY 10017, USA n Pfizer Inc, 10555 Science Center Drive, San Diego, CA, 92121, United States o Pfizer Inc, 235 East 42nd St, New York, NY 10017, USA p Comprehensive Cancer Center, University of Michigan, 1500 East Medical Center Dr, Ann Arbor, MI 48109, USA ARTICLE INFO ABSTRACT Keywords: Glasdegib is a potent and selective oral inhibitor of the Hedgehog pathway. -

Current Challenges and Unmet Medical Needs in Myelodysplastic Syndromes
Leukemia (2021) 35:2182–2198 https://doi.org/10.1038/s41375-021-01265-7 REVIEW ARTICLE Myelodysplastic syndrome Current challenges and unmet medical needs in myelodysplastic syndromes 1,2,3 1,2,3 4 4 Uwe Platzbecker ● Anne Sophie Kubasch ● Collin Homer-Bouthiette ● Thomas Prebet Received: 4 January 2021 / Revised: 1 April 2021 / Accepted: 26 April 2021 / Published online: 28 May 2021 © The Author(s) 2021. This article is published with open access Abstract Myelodysplastic syndromes (MDS) represent a heterogeneous group of myeloid neoplasms that are characterized by ineffective hematopoiesis, variable cytopenias, and a risk of progression to acute myeloid leukemia. Most patients with MDS are affected by anemia and anemia-related symptoms, which negatively impact their quality of life. While many patients with MDS have lower-risk disease and are managed by existing treatments, there currently is no clear standard of care for many patients. For patients with higher-risk disease, the treatment priority is changing the natural history of the disease by delaying disease progression to acute myeloid leukemia and improving overall survival. However, existing treatments for MDS are generally not curative and many patients experience relapse or resistance to first-line treatment. Thus, there remains 1234567890();,: 1234567890();,: an unmet need for new, more effective but tolerable strategies to manage MDS. Recent advances in molecular diagnostics have improved our understanding of the pathogenesis of MDS, and it is becoming clear that the diverse nature of genetic abnormalities that drive MDS demands a complex and personalized treatment approach. This review will discuss some of the challenges related to the current MDS treatment landscape, as well as new approaches currently in development. -

Standard Oncology Criteria C16154-A
Prior Authorization Criteria Standard Oncology Criteria Policy Number: C16154-A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE DUE BEFORE 03/2016 12/2/2020 1/26/2022 HCPCS CODING TYPE OF CRITERIA LAST P&T APPROVAL/VERSION N/A RxPA Q1 2021 20210127C16154-A PRODUCTS AFFECTED: See dosage forms DRUG CLASS: Antineoplastic ROUTE OF ADMINISTRATION: Variable per drug PLACE OF SERVICE: Retail Pharmacy, Specialty Pharmacy, Buy and Bill- please refer to specialty pharmacy list by drug AVAILABLE DOSAGE FORMS: Abraxane (paclitaxel protein-bound) Cabometyx (cabozantinib) Erwinaze (asparaginase) Actimmune (interferon gamma-1b) Calquence (acalbrutinib) Erwinia (chrysantemi) Adriamycin (doxorubicin) Campath (alemtuzumab) Ethyol (amifostine) Adrucil (fluorouracil) Camptosar (irinotecan) Etopophos (etoposide phosphate) Afinitor (everolimus) Caprelsa (vandetanib) Evomela (melphalan) Alecensa (alectinib) Casodex (bicalutamide) Fareston (toremifene) Alimta (pemetrexed disodium) Cerubidine (danorubicin) Farydak (panbinostat) Aliqopa (copanlisib) Clolar (clofarabine) Faslodex (fulvestrant) Alkeran (melphalan) Cometriq (cabozantinib) Femara (letrozole) Alunbrig (brigatinib) Copiktra (duvelisib) Firmagon (degarelix) Arimidex (anastrozole) Cosmegen (dactinomycin) Floxuridine Aromasin (exemestane) Cotellic (cobimetinib) Fludara (fludarbine) Arranon (nelarabine) Cyramza (ramucirumab) Folotyn (pralatrexate) Arzerra (ofatumumab) Cytosar-U (cytarabine) Fusilev (levoleucovorin) Asparlas (calaspargase pegol-mknl Cytoxan (cyclophosphamide) -

Eunethta Joint Action 3 WP4 VENETOCLAX with a HYPOMETHYLATING AGENT for the TREATMENT of ADULT PATIENTS with NEWLY DIAGNOSED
PTJA16 - Venetoclax for acute myeloid leukaemia EUnetHTA Joint Action 3 WP4 Relative effectiveness assessment of pharmaceutical technologies VENETOCLAX WITH A HYPOMETHYLATING AGENT FOR THE TREATMENT OF ADULT PATIENTS WITH NEWLY DIAGNOSED ACUTE MYELOID LEUKAEMIA (AML) WHO ARE INELIGIBLE FOR INTENSIVE CHEMOTHERAPY Project ID: PTJA16 Assessment Report Version 2.0, 03 September 2021 Template version 2.2, April 2020 This Assessment was started as part of the project / joint action ‘724130 / EUnetHTA JA3’ w hich has received funding from the European Union’s Health Programme (2014- 2020). Even though EUnetHTA JA3 has formaly ended in May 2021, the authors of this assessment continued their commitment to finalize this assessment under the agreed methodology of EUnetHTA Joint Action 3. September 21 EUnetHTA Joint Action 3 WP4 1 PTJA16 - Venetoclax for acute myeloid leukaemia DOCUMENT HISTORY AND CONTRIBUTORS Version Date Description V0.1 10/05/2021 First draft V0.2 04/06/2021 Input from dedicated reviewers has been processed V0.3 21/06/2021 Input from medical editor and manufacturer(s) has been processed V1.0 08/07/2021 Final assessment report V2.0 03/09/2021 The following corrections were made: Table 4.16 “Summary of findings for venetoclax + azacitidine versus azacitidine alone in AML”. For the outcome “Treatment discontinuations due to AEs” (mean follow-up 1 month) the reported Relative effect [95% CI] RR 1.28 [1.12–1.46] is corrected to RR 1.21 [0.82-1.78 ]. Table A3 “GRADE - Venetoclax + azacitidine compared to azacitidine + placebo for adult patients with newly-diagnosed acute myeloid leukaemia (AML) who are ineligible for intensive chemotherapy (VIALE-A)”. -

FDA Approval Summary: Glasdegib for Newly Diagnosed Acute Myeloid Leukemia Kelly J
Published OnlineFirst May 7, 2019; DOI: 10.1158/1078-0432.CCR-19-0365 CCR Drug Updates Clinical Cancer Research FDA Approval Summary: Glasdegib for Newly Diagnosed Acute Myeloid Leukemia Kelly J. Norsworthy1, Kunthel By1, Sriram Subramaniam1, Luning Zhuang1, Pedro L. Del Valle1, Donna Przepiorka1, Yuan-Li Shen1, Christopher M. Sheth1, Chao Liu1, Ruby Leong1, Kirsten B. Goldberg2, Ann T. Farrell1, and Richard Pazdur2 Abstract On November 21, 2018, the FDA approved glasdegib 95% confidence interval, 0.30–0.71; one-sided stratified (Daurismo; Pfizer), a small-molecule Hedgehog inhibitor, log-rank P ¼ 0.0002). Median OS was 8.3 months with the in combination with low-dose cytarabine (LDAC) for treat- combination and 4.3 months with LDAC alone. Common ment of newly diagnosed acute myeloid leukemia (AML) in adverse reactions included cytopenias, fatigue, hemorrhage, adults 75 years or with comorbidities that preclude use of febrile neutropenia, musculoskeletal pain, nausea, edema, intensive induction chemotherapy. Evidence of clinical dyspnea, decreased appetite, dysgeusia, mucositis, constipa- benefit came from Study BRIGHT AML 1003, a randomized tion, and rash. The label includes a boxed warning for embryo- trial comparing glasdegibþLDAC with LDAC alone for treat- fetal toxicity and a warning for QT interval prolongation. There ment of newly diagnosed AML in 115 patients either 75 is a limitation of use for patients with moderate-to-severe years old or 55 years old with preexisting comorbidities. hepatic and severe renal impairment; trials studying glasdegib Efficacy was established by improved overall survival (OS) in these patient populations are required as a condition of this with the combination compared with LDAC alone (HR, 0.46; approval.