Recognizing Toxicites of Oral Oncolytics in the Management of Hematologic Malignancies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Stanford Chem-H Presentation (PDF)
KiNativ® In situ kinase profiling Stanford University ChEM-H confidential @KiNativPlatform Principle of the KiNativ platform • ATP (or ADP) acyl phosphate binds to, and covalently modifies Lysine residues in the active site • Thus, ATP acyl phosphate with a desthiobiotin tag can be used capture and quantitate kinases in a complex lysate Acyl phosphate Desthiobiotin tag ATP 2 ATP acyl phosphate probe covalently modifies kinase in the active site Lysine 2 Lysine 1 3 ATP acyl phosphate probe covalently modifies kinase in the active site Lysine 2 Lysine 1 4 Samples trypsinized, probe-labeled peptides captured with streptavidin, and analyzed by targeted LC-MS2 Identification Quantitation Explicit determination of peptide Integration of signal from MS2 sequence and probe modification site fragment ions from MS2 spectrum 5 Comprehensive Coverage of Protein and Lipid Kinases Protein kinases Atypical kinases Green: Kinases detected on KiNativ Red: Kinases not detected on KiNativ ~80% of known protein and atypical kinases identified on the platform http://www.kinativ.com/coverage/protein-lipid.html 6 Profiling compound(s) on the KiNativ platform Control sample – add probe Sample: Lysate derived from any cell line or tissue from ANY species Treated sample – add inhibitor followed by probe Inhibited kinase Green: Kinases Blue: Probe Gray: Non-kinases Red: Inhibitor 7 Profiling compound(s) on the KiNativ platform Control sample – add probe MS signalMS Sample: Lysate derived from any cell line or tissue from ANY species Treated sample – add inhibitor -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
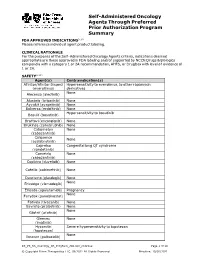
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Refractory Early T-Cell Precursor Acute Lymphoblastic Leukemia
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2019 Venetoclax and Bortezomib in Relapsed/Refractory Early T-Cell Precursor Acute Lymphoblastic Leukemia La Starza, Roberta ; Cambò, Benedetta ; Pierini, Antonio ; Bornhauser, Beat ; Montanaro, Anna ; Bourquin, Jean-Pierre ; Mecucci, Cristina ; Roti, Giovanni DOI: https://doi.org/10.1200/PO.19.00172 Posted at the Zurich Open Repository and Archive, University of Zurich ZORA URL: https://doi.org/10.5167/uzh-198023 Journal Article Published Version The following work is licensed under a Creative Commons: Attribution 4.0 International (CC BY 4.0) License. Originally published at: La Starza, Roberta; Cambò, Benedetta; Pierini, Antonio; Bornhauser, Beat; Montanaro, Anna; Bourquin, Jean-Pierre; Mecucci, Cristina; Roti, Giovanni (2019). Venetoclax and Bortezomib in Relapsed/Refrac- tory Early T-Cell Precursor Acute Lymphoblastic Leukemia. JCO precision oncology, 3:PO.19.00172. DOI: https://doi.org/10.1200/PO.19.00172 case report Venetoclax and Bortezomib in Relapsed/ Refractory Early T-Cell Precursor Acute Lymphoblastic Leukemia Roberta La Starza, MD, PhD1; Benedetta Cambo,` MD2; Antonio Pierini, MD, PhD1; Beat Bornhauser, PhD3; Anna Montanaro2; Jean-Pierre Bourquin, MD, PhD3; Cristina Mecucci, MD, PhD1; and Giovanni Roti, MD, PhD2 INTRODUCTION CD2, CD4, CD8, and CD1a and positive for human Although in the past three decades we welcomed the leukocyte antigen (HLA-DR), CD38, CD117, CD33, advent of targeted therapies in -

Identification of Candidate Repurposable Drugs to Combat COVID-19 Using a Signature-Based Approach
www.nature.com/scientificreports OPEN Identifcation of candidate repurposable drugs to combat COVID‑19 using a signature‑based approach Sinead M. O’Donovan1,10, Ali Imami1,10, Hunter Eby1, Nicholas D. Henkel1, Justin Fortune Creeden1, Sophie Asah1, Xiaolu Zhang1, Xiaojun Wu1, Rawan Alnafsah1, R. Travis Taylor2, James Reigle3,4, Alexander Thorman6, Behrouz Shamsaei4, Jarek Meller4,5,6,7,8 & Robert E. McCullumsmith1,9* The COVID‑19 pandemic caused by the novel SARS‑CoV‑2 is more contagious than other coronaviruses and has higher rates of mortality than infuenza. Identifcation of efective therapeutics is a crucial tool to treat those infected with SARS‑CoV‑2 and limit the spread of this novel disease globally. We deployed a bioinformatics workfow to identify candidate drugs for the treatment of COVID‑19. Using an “omics” repository, the Library of Integrated Network‑Based Cellular Signatures (LINCS), we simultaneously probed transcriptomic signatures of putative COVID‑19 drugs and publicly available SARS‑CoV‑2 infected cell lines to identify novel therapeutics. We identifed a shortlist of 20 candidate drugs: 8 are already under trial for the treatment of COVID‑19, the remaining 12 have antiviral properties and 6 have antiviral efcacy against coronaviruses specifcally, in vitro. All candidate drugs are either FDA approved or are under investigation. Our candidate drug fndings are discordant with (i.e., reverse) SARS‑CoV‑2 transcriptome signatures generated in vitro, and a subset are also identifed in transcriptome signatures generated from COVID‑19 patient samples, like the MEK inhibitor selumetinib. Overall, our fndings provide additional support for drugs that are already being explored as therapeutic agents for the treatment of COVID‑19 and identify promising novel targets that are worthy of further investigation. -

Cstone Pharmaceuticals 基石藥業
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. The forward-looking statements made in this announcement relate only to the events or information as of the date on which the statements are made in this announcement. Except as required by law, we undertake no obligation to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise, after the date on which the statements are made or to reflect the occurrence of unanticipated events. You should read this announcement completely and with the understanding that our actual future results or performance may be materially different from what we expect. In this announcement, statements of, or references to, our intentions or those of any of our directors and/or our Company are made as of the date of this announcement. Any of these intentions may alter in light of future development. CStone Pharmaceuticals 基 石 藥 業 (Incorporated in the Cayman Islands with limited liability) (Stock Code: 2616) VOLUNTARY ANNOUNCEMENT CSTONE SUCCESSFULLY HOSTED THE FIRST U.S. R&D DAY IN NEW YORK CStone Pharmaceuticals (the “Company” or “CStone”) announces that it successfully hosted its 2020 U.S. R&D Day in New York City, the United States on January 21, 2020. -

ESMO 2019 Update
ESMO 2019 Update Axel Grothey Director, GI Oncology Research West Cancer Center Research Institute Encorafenib plus Cetuximab With or Without Binimetinib for BRAF V600E–Mutant Metastatic Colorectal Cancer: Expanded Results from a Randomized, 3-Arm, Phase 3 Study vs. the Choice of Either Irinotecan or FOLFIRI plus Cetuximab (BEACON CRC) Josep Tabernero, Axel Grothey, Eric Van Cutsem, Rona Yaeger, Harpreet Wasan, Takayuki Yoshino, Jayesh Desai, Fortunato Ciardiello, Fotios Loupakis, Yong Sang Hong, Neeltje Steeghs, Tormod Kyrre Guren, Hendrik-Tobias Arkenau, Pilar Garcia-Alfonso, Ashwin Gollerkeri, Michael Pickard, Kati Maharry, Janna Christy-Bittel, Lisa Anderson, and Scott Kopetz BEACON CRC: Binimetinib, Encorafenib, And Cetuximab COmbiNed to Treat BRAF-mutant ColoRectal Cancer 2 Study Design Patients with BRAFV600E mCRC with disease progression after 1 or 2 prior regimens; ECOG PS of 0 or 1; and no prior treatment with any RAF inhibitor, MEK inhibitor, or EGFR inhibitor Phase 3 Primary Endpoints: Safety Lead-in ENCORAFENIB + Triplet therapy BINIMETINIB + ENCORAFENIB + BINIMETINIB + CETUXIMAB Triplet vs Control n = 205 CETUXIMAB N = 30 OS R Doublet therapy (All randomized Pts) Encorafenib 300 mg PO daily 1:1:1 ENCORAFENIB + CETUXIMAB Binimetinib 45 mg PO bid n = 205 Cetuximab standard weekly ORR – dosing Blinded Central Control arm Review FOLFIRI + CETUXIMAB, or (1st 331 randomized Pts) irinotecan + CETUXIMAB n = 205 Randomization was stratified by ECOG PS (0 vs. 1), prior use of irinotecan (yes vs. no), and cetuximab source (US-licensed vs. EU-approved) Secondary Endpoints: Doublet vs Control and Triplet vs Doublet - OS & ORR, PFS, Safety QOL Assessments: EORTC QOL Questionnaire (QLQ C30), Functional Assessment of Cancer Therapy Colon Cancer, EuroQol 5D5L, and Patient Global Impression of Change). -

BCBSVT Specialty Drug List Effective 2021.07.01.Xlsx
Effective Date: 07/01/2021 SPECIALTY DRUG LIST Revised Date: 05/07/2021 DOSAGE EXCLUDED ON NATIONAL DRUG CLASS DRUG NAME GENERIC NAME FORM PERFORMANCE FORMULARY ANEMIA ARANESP SOLN DARBEPOETIN ALFA SOLN INJ ANEMIA ARANESP SOSY DARBEPOETIN ALFA SOLN PREFILLED SYRINGE ANEMIA EPOGEN SOLN EPOETIN ALFA INJ X ANEMIA PROCRIT SOLN EPOETIN ALFA INJ X ANEMIA REBLOZYL SOLR LUSPATERCEPT-AAMT FOR SUBCUTANEOUS INJ ANEMIA RETACRIT SOLN EPOETIN ALFA-EPBX INJ ANTI-GOUT AGENT KRYSTEXXA SOLN PEGLOTICASE INJ (FOR IV INFUSION) ANTI-INFECTIVE PREVYMIS SOLN LETERMOVIR IV SOLN ANTI-INFECTIVE PREVYMIS TABS LETERMOVIR TAB ASTHMA CINQAIR SOLN RESLIZUMAB IV INFUSION SOLN ASTHMA FASENRA SOSY BENRALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE ASTHMA FASENRA PEN SOAJ BENRALIZUMAB SUBCUTANEOUS SOLN AUTO-INJECTOR ASTHMA NUCALA SOAJ MEPOLIZUMAB SUBCUTANEOUS SOLUTION AUTO-INJECTOR ASTHMA NUCALA SOLR MEPOLIZUMAB FOR INJ ASTHMA NUCALA SOSY MEPOLIZUMAB SUBCUTANEOUS SOLUTION PREF SYRINGE ASTHMA XOLAIR SOLR OMALIZUMAB FOR INJ ASTHMA XOLAIR SOSY OMALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE CARDIOVASCULAR VYNDAMAX CAPS TAFAMIDIS CAP CARDIOVASCULAR VYNDAQEL CAPS TAFAMIDIS MEGLUMINE (CARDIAC) CAP CENTRAL NERVOUS SYSTEM AGENTS AUSTEDO TABS DEUTETRABENAZINE TAB CENTRAL NERVOUS SYSTEM AGENTS ENSPRYNG SOSY SATRALIZUMAB-MWGE SUBCUTANEOUS SOLN PREF SYRINGE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ CAPS TASIMELTEON CAPSULE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ LQ SUSP TASIMELTEON ORAL SUSP CHEMOTHERAPY PROTECTANT AMIFOSTINE SOLR AMIFOSTINE CRYSTALLINE FOR INJ CHEMOTHERAPY PROTECTANT ELITEK -

August 2019 New Drugs
August 2019 Learn more New drugs Drug name Therapeutic category Indication(s) Launch information Manufacturer(s) ® † Inrebic (fedratinib) * Treatment of adult patients with intermediate-2 or high-risk Janus kinase 2 inhibitor primary or secondary (post-polycythemia vera or post- August 19, 2019 Celgene essential thrombocythemia) myelofibrosis ™ Nourianz (istradefylline)* A2A adenosine receptor Adjunctive treatment to levodopa/carbidopa in adult patients TBD antagonist with Parkinson’s disease experiencing “off” episodes Kyowa Kirin † Part of a combination regimen with Sirturo (bedaquiline) and Pretomanid * linezolid for the treatment of adults with pulmonary Nitroimidazole End of 2019 extensively drug resistant or treatment-intolerant or TB Alliance nonresponsive multidrug-resistant tuberculosis ™ Rinvoq (upadacitinib)* Treatment of adults with moderately to severely active Janus kinase inhibitor rheumatoid arthritis who have had an inadequate response or August 19, 2019 AbbVie intolerance to methotrexate Riomet ER™ (metformin) Adjunct to diet and exercise to improve glycemic control in extended-release oral suspension Biguanide adults and pediatric patients 10 years of age and older with TBD type 2 diabetes mellitus Sun Pharma 1 RxHighlights August 2019 Drug name Therapeutic category Indication(s) Launch information Manufacturer(s) Treatment of adult patients with metastatic non-small cell lung cancer whose tumors are ROS1-positive; treatment of adult ™ † and pediatric patients 12 years of age and older with solid Rozlytrek (entrectinib) -

Immunotherapy in Myeloproliferative Diseases
cells Review Immunotherapy in Myeloproliferative Diseases Lukas M. Braun 1,2 and Robert Zeiser 1,3,4,5,* 1 Department of Medicine I, Medical Center—University of Freiburg, Faculty of Medicine, University of Freiburg, 79106 Freiburg, Germany; [email protected] 2 Faculty of Biology, University of Freiburg, 79104 Freiburg, Germany 3 German Cancer Consortium (DKTK) Partner Site Freiburg, German Cancer Research Center (DKFZ), 69120 Heidelberg, Germany 4 Comprehensive Cancer Center Freiburg (CCCF), University of Freiburg, 79106 Freiburg, Germany 5 Centre for Biological Signalling Studies (BIOSS) and Centre for Integrative Biological Signalling Studies (CIBSS), University of Freiburg, 79104 Freiburg, Germany * Correspondence: [email protected] Received: 9 June 2020; Accepted: 23 June 2020; Published: 26 June 2020 Abstract: Myeloproliferative diseases, including myeloproliferative neoplasms (MPN) and myelodysplastic syndromes (MDS), are driven by genetic abnormalities and increased inflammatory signaling and are at high risk to transform into acute myeloid leukemia (AML). Myeloid-derived suppressor cells were reported to enhance leukemia immune escape by suppressing an effective anti-tumor immune response. MPNs are a potentially immunogenic disease as shown by their response to interferon-α treatment and allogeneic hematopoietic stem-cell transplantation (allo-HSCT). Novel immunotherapeutic approaches such as immune checkpoint inhibition, tumor vaccination, or cellular therapies using target-specific lymphocytes have so far not shown strong therapeutic efficacy. Potential reasons could be the pro-inflammatory and immunosuppressive microenvironment in the bone marrow of patients with MPN, driving tumor immune escape. In this review, we discuss the biology of MPNs with respect to the pro-inflammatory milieu in the bone marrow (BM) and potential immunotherapeutic approaches. -

New Century Health Policy Changes April 2021
Policy # Drug(s) Type of Change Brief Description of Policy Change new Pepaxto (melphalan flufenamide) n/a n/a new Fotivda (tivozanib) n/a n/a new Cosela (trilaciclib) n/a n/a Add inclusion criteria: NSCLC UM ONC_1089 Libtayo (cemiplimab‐rwlc) Negative change 2.Libtayo (cemiplimab) may be used as montherapy in members with locally advanced, recurrent/metastatic NSCLC, with PD‐L1 ≥ 50%, negative for actionable molecular markers (ALK, EGFR, or ROS‐1) Add inclusion criteria: a.As a part of primary/de�ni�ve/cura�ve‐intent concurrent chemo radia�on (Erbitux + Radia�on) as a single agent for members with a UM ONC_1133 Erbitux (Cetuximab) Positive change contraindication and/or intolerance to cisplatin use OR B.Head and Neck Cancers ‐ For recurrent/metasta�c disease as a single agent, or in combination with chemotherapy. Add inclusion criteria: UM ONC_1133 Erbitux (Cetuximab) Negative change NOTE: Erbitux (cetuximab) + Braftovi (encorafenib) is NCH preferred L1 pathway for second‐line or subsequent therapy in the metastatic setting, for BRAFV600E positive colorectal cancer.. Add inclusion criteria: B.HER‐2 Posi�ve Breast Cancer i.Note #1: For adjuvant (post‐opera�ve) use in members who did not receive neoadjuvant therapy/received neoadjuvant therapy and did not have any residual disease in the breast and/or axillary lymph nodes, Perjeta (pertuzumab) use is restricted to node positive stage II and III disease only. ii.Note #2: Perjeta (pertuzumab) use in the neoadjuvant (pre‐opera�ve) se�ng requires radiographic (e.g., breast MRI, CT) and/or pathologic confirmation of ipsilateral (same side) axillary nodal involvement. -

TIBSOVO® (Ivosidenib) Oral
PHARMACY COVERAGE GUIDELINES ORIGINAL EFFECTIVE DATE: 9/20/2018 SECTION: DRUGS LAST REVIEW DATE: 8/19/2021 LAST CRITERIA REVISION DATE: 8/19/2021 ARCHIVE DATE: TIBSOVO® (ivosidenib) oral Coverage for services, procedures, medical devices and drugs are dependent upon benefit eligibility as outlined in the member's specific benefit plan. This Pharmacy Coverage Guideline must be read in its entirety to determine coverage eligibility, if any. This Pharmacy Coverage Guideline provides information related to coverage determinations only and does not imply that a service or treatment is clinically appropriate or inappropriate. The provider and the member are responsible for all decisions regarding the appropriateness of care. Providers should provide BCBSAZ complete medical rationale when requesting any exceptions to these guidelines. The section identified as “Description” defines or describes a service, procedure, medical device or drug and is in no way intended as a statement of medical necessity and/or coverage. The section identified as “Criteria” defines criteria to determine whether a service, procedure, medical device or drug is considered medically necessary or experimental or investigational. State or federal mandates, e.g., FEP program, may dictate that any drug, device or biological product approved by the U.S. Food and Drug Administration (FDA) may not be considered experimental or investigational and thus the drug, device or biological product may be assessed only on the basis of medical necessity. Pharmacy Coverage Guidelines are subject to change as new information becomes available. For purposes of this Pharmacy Coverage Guideline, the terms "experimental" and "investigational" are considered to be interchangeable. BLUE CROSS®, BLUE SHIELD® and the Cross and Shield Symbols are registered service marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield Plans. -

FORM 20-F 2013 UNITED STATES SECURITIES and EXCHANGE COMMISSION Washington, D.C
FORM 20-F 2013 UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 20-F (Mark One) Ⅺ REGISTRATION STATEMENT PURSUANT TO SECTION 12(b) OR (g) OF THE SECURITIES EXCHANGE ACT OF 1934 OR ࠚ ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the fiscal year ended December 31, 2013 OR Ⅺ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 OR Ⅺ SHELL COMPANY REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 Date of event requiring this shell company report. For the transition period from to Commission File Number: 001-31368 Sanofi (Exact name of registrant as specified in its charter) N/A (Translation of registrant’s name into English) France (Jurisdiction of incorporation or organization) 54, Rue La Boetie,´ 75008 Paris, France (Address of principal executive offices) Karen Linehan, Executive Vice President Legal Affairs and General Counsel 54, Rue La Boetie´ , 75008 Paris, France. Fax: 011 + 33 1 53 77 43 03. Tel: 011 + 33 1 53 77 40 00 (Name, Telephone, E-mail and/or Facsimile number and Address of Company Contact Person) Securities registered or to be registered pursuant to Section 12(b) of the Act: Title of each class: Name of each exchange on which registered: American Depositary Shares, each New York Stock Exchange representing one half of one ordinary share, par value e2 per share Ordinary shares, par value e2 per share New York Stock Exchange (for listing purposes only) Contingent Value Rights NASDAQ Global Market Securities registered pursuant to Section 12(g) of the Act: None The number of outstanding shares of each of the issuer’s classes of capital or common stock as of December 31, 2013 was: Ordinary shares: 1,324,320,881 Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act.