Oncogenic Mechanisms and Therapeutic Targeting of Metabolism in Leukemia and Lymphoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Prospective, Multicenter, Phase-II Trial of Ibrutinib Plus Venetoclax In
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 A prospective, multicenter, phase-II trial of ibrutinib plus venetoclax in patients with creatinine clearance ≥ 30 ml/min who have relapsed or refractory chronic lymphocytic leukemia (RR-CLL) with or without TP53 aberrations HOVON 141 CLL / VIsion Trial of the HOVON and Nordic CLL study groups PROTOCOL Principal Investigator : Arnon P Kater (HOVON) Carsten U Niemann (Nordic CLL study Group)) Sponsor : HOVON EudraCT number : 2016-002599-29 ; Page 1 of 107 Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 LOCAL INVESTIGATOR SIGNATURE PAGE Local site name: Signature of Local Investigator Date Printed Name of Local Investigator By my signature, I agree to personally supervise the conduct of this study in my affiliation and to ensure its conduct in compliance with the protocol, informed consent, IRB/EC procedures, the Declaration of Helsinki, ICH Good Clinical Practices guideline, the EU directive Good Clinical Practice (2001-20-EG), and local regulations governing the conduct of clinical studies. -

The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia
International Journal of Molecular Sciences Review The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia Marta Weronika Lato 1 , Anna Przysucha 1, Sylwia Grosman 1, Joanna Zawitkowska 2 and Monika Lejman 3,* 1 Student Scientific Society, Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] (M.W.L.); [email protected] (A.P.); [email protected] (S.G.) 2 Department of Pediatric Hematology, Oncology and Transplantology, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 3 Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland * Correspondence: [email protected] Abstract: Childhood acute lymphoblastic leukemia is a genetically heterogeneous cancer that ac- counts for 10–15% of T-cell acute lymphoblastic leukemia (T-ALL) cases. The T-ALL event-free survival rate (EFS) is 85%. The evaluation of structural and numerical chromosomal changes is important for a comprehensive biological characterization of T-ALL, but there are currently no ge- netic prognostic markers. Despite chemotherapy regimens, steroids, and allogeneic transplantation, relapse is the main problem in children with T-ALL. Due to the development of high-throughput molecular methods, the ability to define subgroups of T-ALL has significantly improved in the last few years. The profiling of the gene expression of T-ALL has led to the identification of T-ALL subgroups, and it is important in determining prognostic factors and choosing an appropriate treatment. Novel therapies targeting molecular aberrations offer promise in achieving better first remission with the Citation: Lato, M.W.; Przysucha, A.; hope of preventing relapse. -

Nick-Thomas.Pdf
Innovating Pre-Clinical Drug Development Towards an Integrated Approach to Investigative Toxicology in Human Cell Models Nick Thomas PhD Principal Scientist Cell Technologies GE Healthcare ELRIG Pharmaceutical Flow Cytometry & Imaging 2012 10-11th October 2012, AstraZeneca, Alderley Park Drug Toxicology Current issues – problems & solutions Using animal models to reflect Quality and robustness of Testing multiple endpoints human responses toxicity cell models leading to false-positives • animals ≠ humans • scarcity of primary cells/tissues • multiple testing increases • animal ≠ animal • source variability sensitivity at cost of specificity • cross species testing may • more abundant models • different assay combinations increase sensitivity but (immortalized/genetically yield varying predictivity decrease specificity engineered cells) may have • testing multiple endpoints leads • metabolism & MOA ? reduced predictivity to false positives Sensitivity Specificity Assay Combinations Integrate range of predictive Integrate robust human stem Integrate and standardize human cell models cell derived models most predictive parameters Cytiva™ Cardiomyocytes H7 hESC Cardiomyocytes 109 Expansion Differentiation 0 5 10 15 20 25 30 Media 1 Media 2 Growth Factors Feed Cytiva Cardiomyocytes DNA Troponin I DNA Connexin 43 Troponin I HCA Biochemical Assays Patch Clamp Impedance Multi-Electrode Arrays Respiration HCA Biochemical Assays Patch Clamp Impedance Multi-Electrode Arrays Respiration Cardiotoxicity Profiling of Anticancer Drugs Cytiva Cardiomyocytes & IN Cell Analyzer Cardiotoxicity & Anticancer Drugs Drug Pipelines Toxicity in Drug Development Hepatotoxicity Nephrotoxicity Cardiotoxicity Rhabdomyolysis Other Data from: Drug pipeline: Q411. Mak H.C. 2012 Data from; Wilke RA et al. Nature Reviews Drug Discovery Nature Biotechnol. 30,15 2007 6, 904-916 Cardiotoxicity of Anticancer Drugs Off Target On Target : Off Therapy DOX GATA4 ROS Bcl2 Cell Death Adapted from; Kobayashi S. -
Draft Matrix Post Referral PDF 189 KB
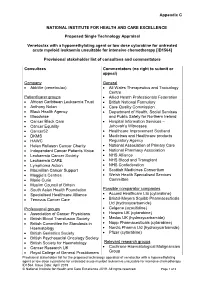
Appendix C NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Proposed Single Technology Appraisal Venetoclax with a hypomethylating agent or low dose cytarabine for untreated acute myeloid leukaemia unsuitable for intensive chemotherapy [ID1564] Provisional stakeholder list of consultees and commentators Consultees Commentators (no right to submit or appeal) Company General • AbbVie (venetoclax) • All Wales Therapeutics and Toxicology Centre Patient/carer groups • Allied Health Professionals Federation • African Caribbean Leukaemia Trust • British National Formulary • Anthony Nolan • Care Quality Commission • Black Health Agency • Department of Health, Social Services • Bloodwise and Public Safety for Northern Ireland • Cancer Black Care • Hospital Information Services – • Cancer Equality Jehovah’s Witnesses • Cancer52 • Healthcare Improvement Scotland • DKMS • Medicines and Healthcare products • HAWC Regulatory Agency • Helen Rollason Cancer Charity • National Association of Primary Care • Independent Cancer Patients Voice • National Pharmacy Association • Leukaemia Cancer Society • NHS Alliance • Leukaemia CARE • NHS Blood and Transplant • Lymphoma Action • NHS Confederation • Macmillan Cancer Support • Scottish Medicines Consortium • Maggie’s Centres • Welsh Health Specialised Services • Marie Curie Committee • Muslim Council of Britain • South Asian Health Foundation Possible comparator companies • Specialised Healthcare Alliance • Accord Healthcare Ltd (cytarabine) • Tenovus Cancer Care • Bristol-Meyers Squibb Pharmaceuticals Ltd -

A Novel CDK9 Inhibitor Increases the Efficacy of Venetoclax (ABT-199) in Multiple Models of Hematologic Malignancies
Leukemia (2020) 34:1646–1657 https://doi.org/10.1038/s41375-019-0652-0 ARTICLE Molecular targets for therapy A novel CDK9 inhibitor increases the efficacy of venetoclax (ABT-199) in multiple models of hematologic malignancies 1 1 2,3 4 1 5 6 Darren C. Phillips ● Sha Jin ● Gareth P. Gregory ● Qi Zhang ● John Xue ● Xiaoxian Zhao ● Jun Chen ● 1 1 1 1 1 1 Yunsong Tong ● Haichao Zhang ● Morey Smith ● Stephen K. Tahir ● Rick F. Clark ● Thomas D. Penning ● 2,7 3 5 1 4 2,7 Jennifer R. Devlin ● Jake Shortt ● Eric D. Hsi ● Daniel H. Albert ● Marina Konopleva ● Ricky W. Johnstone ● 8 1 Joel D. Leverson ● Andrew J. Souers Received: 27 November 2018 / Revised: 18 October 2019 / Accepted: 13 November 2019 / Published online: 11 December 2019 © The Author(s) 2019 Abstract MCL-1 is one of the most frequently amplified genes in cancer, facilitating tumor initiation and maintenance and enabling resistance to anti-tumorigenic agents including the BCL-2 selective inhibitor venetoclax. The expression of MCL-1 is maintained via P-TEFb-mediated transcription, where the kinase CDK9 is a critical component. Consequently, we developed a series of potent small-molecule inhibitors of CDK9, exemplified by the orally active A-1592668, with CDK selectivity profiles 1234567890();,: 1234567890();,: that are distinct from related molecules that have been extensively studied clinically. Short-term treatment with A-1592668 rapidly downregulates RNA pol-II (Ser 2) phosphorylation resulting in the loss of MCL-1 protein and apoptosis in MCL-1- dependent hematologic tumor cell lines. This cell death could be attenuated by either inhibiting caspases or overexpressing BCL-2 protein. -

Related Kinases (VRK) Bound to Small-Molecule Inhibitors Identifies Different P-Loop Conformations
Structural characterization of human Vaccinia- Related Kinases (VRK) bound to small-molecule inhibitors identifies different P-loop conformations Rafael M. Couñago1,2*, Charles K. Allerston3, Pavel Savitsky3, Hatylas Azevedo4, Paulo H Godoi1,5, Carrow I. Wells6, Alessandra Mascarello4, Fernando H. de Souza Gama4, Katlin B. Massirer1,2, William J. Zuercher6, Cristiano R.W. Guimarães4 and Opher Gileadi1,3 1. Structural Genomics Consortium, Universidade Estadual de Campinas — UNICAMP, Campinas, SP, Brazil. 2. Centro de Biologia Molecular e Engenharia Genética, Universidade Estadual de Campinas, Campinas, SP, Brazil. 3. Structural Genomics Consortium and Target Discovery Institute, Nuffield Department of Clinical Medicine, University of Oxford, UK. 4. Aché Laboratórios Farmacêuticos SA, Guarulhos, SP, Brazil. 5. Department of Biochemistry and Tissue Biology, Institute of Biology, State University of Campinas, Campinas, Brazil. 6. Structural Genomics Consortium, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill, NC, USA. *Correspondence to Rafael M. Couñago: [email protected] (RMC) Supplementary information 1 SUPPLEMENTARY METHODS PKIS results analyses - hierarchical cluster analysis (HCL) A hierarchical clustering (HCL) analysis was performed to group kinases based on their inhibition patterns across the compounds. The average distance clustering method was employed, using sample tree selection and sample leaf order optimization. The distance metric used was the Pearson correlation and the HCL analysis was performed in the TmeV software 1. SUPPLEMENTARY REFERENCES 1 Saeed, A. I. et al. TM4: a free, open-source system for microarray data management and analysis. BioTechniques 34, 374-378, (2003). SUPPLEMENTARY FIGURES LEGENDS Supplementary Figure S1: Hierarchical clustering analysis of PKIS data. Hierarchical clustering analysis of PKIS data. -

Modifications to the Harmonized Tariff Schedule of the United States To
U.S. International Trade Commission COMMISSIONERS Shara L. Aranoff, Chairman Daniel R. Pearson, Vice Chairman Deanna Tanner Okun Charlotte R. Lane Irving A. Williamson Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement the Dominican Republic- Central America-United States Free Trade Agreement With Respect to Costa Rica Publication 4038 December 2008 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 18, 2008, set forth in the Appendix hereto, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement the Dominican Republic- Central America-United States Free Trade Agreement, as approved in the Dominican Republic-Central America- United States Free Trade Agreement Implementation Act, with respect to Costa Rica. (This page is intentionally blank) Annex I Effective with respect to goods that are entered, or withdrawn from warehouse for consumption, on or after January 1, 2009, the Harmonized Tariff Schedule of the United States (HTS) is modified as provided herein, with bracketed matter included to assist in the understanding of proclaimed modifications. The following supersedes matter now in the HTS. (1). General note 4 is modified as follows: (a). by deleting from subdivision (a) the following country from the enumeration of independent beneficiary developing countries: Costa Rica (b). -

Targeting the Function of the HER2 Oncogene in Human Cancer Therapeutics
Oncogene (2007) 26, 6577–6592 & 2007 Nature Publishing Group All rights reserved 0950-9232/07 $30.00 www.nature.com/onc REVIEW Targeting the function of the HER2 oncogene in human cancer therapeutics MM Moasser Department of Medicine, Comprehensive Cancer Center, University of California, San Francisco, CA, USA The year 2007 marks exactly two decades since human HER3 (erbB3) and HER4 (erbB4). The importance of epidermal growth factor receptor-2 (HER2) was func- HER2 in cancer was realized in the early 1980s when a tionally implicated in the pathogenesis of human breast mutationally activated form of its rodent homolog neu cancer (Slamon et al., 1987). This finding established the was identified in a search for oncogenes in a carcinogen- HER2 oncogene hypothesis for the development of some induced rat tumorigenesis model(Shih et al., 1981). Its human cancers. An abundance of experimental evidence human homologue, HER2 was simultaneously cloned compiled over the past two decades now solidly supports and found to be amplified in a breast cancer cell line the HER2 oncogene hypothesis. A direct consequence (King et al., 1985). The relevance of HER2 to human of this hypothesis was the promise that inhibitors of cancer was established when it was discovered that oncogenic HER2 would be highly effective treatments for approximately 25–30% of breast cancers have amplifi- HER2-driven cancers. This treatment hypothesis has led cation and overexpression of HER2 and these cancers to the development and widespread use of anti-HER2 have worse biologic behavior and prognosis (Slamon antibodies (trastuzumab) in clinical management resulting et al., 1989). -

Phenotype-Based Drug Screening Reveals Association Between Venetoclax Response and Differentiation Stage in Acute Myeloid Leukemia
Acute Myeloid Leukemia SUPPLEMENTARY APPENDIX Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia Heikki Kuusanmäki, 1,2 Aino-Maija Leppä, 1 Petri Pölönen, 3 Mika Kontro, 2 Olli Dufva, 2 Debashish Deb, 1 Bhagwan Yadav, 2 Oscar Brück, 2 Ashwini Kumar, 1 Hele Everaus, 4 Bjørn T. Gjertsen, 5 Merja Heinäniemi, 3 Kimmo Porkka, 2 Satu Mustjoki 2,6 and Caroline A. Heckman 1 1Institute for Molecular Medicine Finland, Helsinki Institute of Life Science, University of Helsinki, Helsinki; 2Hematology Research Unit, Helsinki University Hospital Comprehensive Cancer Center, Helsinki; 3Institute of Biomedicine, School of Medicine, University of Eastern Finland, Kuopio, Finland; 4Department of Hematology and Oncology, University of Tartu, Tartu, Estonia; 5Centre for Cancer Biomarkers, De - partment of Clinical Science, University of Bergen, Bergen, Norway and 6Translational Immunology Research Program and Department of Clinical Chemistry and Hematology, University of Helsinki, Helsinki, Finland ©2020 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2018.214882 Received: December 17, 2018. Accepted: July 8, 2019. Pre-published: July 11, 2019. Correspondence: CAROLINE A. HECKMAN - [email protected] HEIKKI KUUSANMÄKI - [email protected] Supplemental Material Phenotype-based drug screening reveals an association between venetoclax response and differentiation stage in acute myeloid leukemia Authors: Heikki Kuusanmäki1, 2, Aino-Maija -

Sorafenib and Omacetaxine Mepesuccinate As a Safe and Effective Treatment for Acute Myeloid Leukemia Carrying Internal Tandem Du
Original Article Sorafenib and Omacetaxine Mepesuccinate as a Safe and Effective Treatment for Acute Myeloid Leukemia Carrying Internal Tandem Duplication of Fms-Like Tyrosine Kinase 3 Chunxiao Zhang, MSc1; Stephen S. Y. Lam, MBBS, PhD1; Garret M. K. Leung, MBBS1; Sze-Pui Tsui, MSc2; Ning Yang, PhD1; Nelson K. L. Ng, PhD1; Ho-Wan Ip, MBBS2; Chun-Hang Au, PhD3; Tsun-Leung Chan, PhD3; Edmond S. K. Ma, MBBS3; Sze-Fai Yip, MBBS4; Harold K. K. Lee, MBChB5; June S. M. Lau, MBChB6; Tsan-Hei Luk, MBChB6; Wa Li, MBChB7; Yok-Lam Kwong, MD 1; and Anskar Y. H. Leung, MD, PhD 1 BACKGROUND: Omacetaxine mepesuccinate (OME) has antileukemic effects against acute myeloid leukemia (AML) carrying an internal tandem duplication of Fms-like tyrosine kinase 3 (FLT3-ITD). A phase 2 clinical trial was conducted to evaluate a combina- tion treatment of sorafenib and omacetaxine mepesuccinate (SOME). METHODS: Relapsed or refractory (R/R) or newly diagnosed patients were treated with sorafenib (200-400 mg twice daily) and OME (2 mg daily) for 7 (first course) or 5 days (second course on- ward) every 21 days until disease progression or allogeneic hematopoietic stem cell transplantation (HSCT). The primary endpoint was composite complete remission, which was defined as complete remission (CR) plus complete remission with incomplete hematologic recovery (CRi). Secondary endpoints were leukemia-free survival (LFS) and overall survival (OS). RESULTS: Thirty-nine R/R patients and 5 newly diagnosed patients were recruited. Among the R/R patients, 28 achieved CR or CRi. Two patients showed partial remission, and 9 patients did not respond. -

Elife-55845-Figures.Pdf
RESEARCH ARTICLE Figures and figure supplements Identification of a novel toxicophore in anti-cancer chemotherapeutics that targets mitochondrial respiratory complex I Zoe A Stephenson et al Stephenson et al. eLife 2020;9:e55845. DOI: https://doi.org/10.7554/eLife.55845 1 of 20 Research article Biochemistry and Chemical Biology Cancer Biology A) B) Mubritinib (µM) pHER2 (Y1221/1222) - HER2 p-HER2 (Y1221/1222) p-ACC (S-79) HER2 ACC ȕ-tubulin p-RPS6 (S-240/244) RPS6 ȕ-tubulin C) D) E) Untreated Mubritinib 120 125125 140 100 120 100100 80 100 7575 60 80 5050 40 60 HER2 activity HER2activity HER2 activity HER2activity Kinase activity Kinase activity 40 2525 20 (% relative to untreated) 20 (% relative to untreated) *** 00 0 (% relative to untreated) 0 Mubritinib (µM) F) G) Glucose Galactose 120 100 Glucose UntreatedUntreated 100 ns Galactose UntreatedUntreated 75 **** 80 Glucose Mubritinib (2 µ M ) 60 *** *** 50 Galactose MubritinibMubritinib (2 µ M ) **** 40 Live (%) cells Cellular ATP Cellular 25 **** **** 20 **** (% relative to untreated) 0 0 0 1 2 4 6 24 0 24 48 72 Mubritinib (hours) Time (hours) H) I i) I ii) Glucose Galactose Glucose Galactose DMSO Mubritinib Antimycin A Rotenone DMSO Mubritinib Antimycin A Rotenone ns **** **** **** **** 150 150 * ** 100 * *** 0 125 0 125 ** 80 100 100 60 75 75 40 50 50 BPM BPM relative to t BPM relative to t Cellular ATP Cellular 20 25 25 (% relative to untreated) 0 0 0 0 10 30 60 120 0 10 30 60 120 Time (minutes) Time (minutes) Figure 1. Mubritinib does not inhibit HER2, but inhibits ATP production and beat rate of cardiomyocytes. -

A Novel JAK1 Mutant Breast Implant-Associated Anaplastic Large Cell Lymphoma Patient-Derived Xenograft Fostering Pre- Clinical Discoveries
Cancers 2019 S1 of S18 Supplementary Materials: A Novel JAK1 Mutant Breast Implant-Associated Anaplastic Large Cell Lymphoma Patient-Derived Xenograft Fostering Pre- Clinical Discoveries Danilo Fiore, Luca Vincenzo Cappelli, Paul Zumbo, Jude M. Phillip, Zhaoqi Liu, Shuhua Cheng, Liron Yoffe, Paola Ghione, Federica Di Maggio, Ahmet Dogan, Inna Khodos, Elisa de Stanchina, Joseph Casano, Clarisse Kayembe, Wayne Tam, Doron Betel, Robin Foa’, Leandro Cerchietti, Raul Rabadan, Steven Horwitz, David M. Weinstock and Giorgio Inghirami A B C Figure S1. (A) Histology micrografts on IL89 PDTX show overall similarity between T1 T3 and T7 passages (upper panels). Immunohistochemical stains with the indicated antibodies (anti-CD3, anti- CD25 and anti-CD8 [x20]) (lower panels). (B) Flow cytometry panel comprehensive of the most represented surface T-cell lymphoma markers, including: CD2, CD3, CD4, CD5, CD8, CD16, CD25, CD30, CD56, TCRab, TCRgd. IL89 PDTX passage T3 is here depicted for illustration purposes. (C) Analysis of the TCR gamma specific rearrangement clonality in IL89 diagnostic sample and correspondent PDTX after 1 and 5 passages (T1 and T5). A WT Primary p.G1097D IL89 T1 p.G1097D IL89 T5 p.G1097D IL89 cell line B Figure S2. (A) Sanger sequencing confirms the presence of the JAK1 p.G1097D mutation in IL89 PDTX samples and in the cell line, but the mutation is undetectable in the primary due to the low sensitivity of the technique. (B) Manual backtracking of mutations in the primary tumor using deep sequencing data allowed for the identification of several hits at a very low VAF compared to the PDTX-T5. A B IL89 CTRL 30 CTRL Ruxoli?nib S 20 M Ruxoli?nib A R G 10 0 1 2 3 4 5 6 7 8 9 0 1 2 3 4 1 1 1 1 1 WEEKS AFTER ENGRAFTMENT Figure S3.