| Oral Chemotherapy Monitoring & Counseling
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Prospective, Multicenter, Phase-II Trial of Ibrutinib Plus Venetoclax In
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 A prospective, multicenter, phase-II trial of ibrutinib plus venetoclax in patients with creatinine clearance ≥ 30 ml/min who have relapsed or refractory chronic lymphocytic leukemia (RR-CLL) with or without TP53 aberrations HOVON 141 CLL / VIsion Trial of the HOVON and Nordic CLL study groups PROTOCOL Principal Investigator : Arnon P Kater (HOVON) Carsten U Niemann (Nordic CLL study Group)) Sponsor : HOVON EudraCT number : 2016-002599-29 ; Page 1 of 107 Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 LOCAL INVESTIGATOR SIGNATURE PAGE Local site name: Signature of Local Investigator Date Printed Name of Local Investigator By my signature, I agree to personally supervise the conduct of this study in my affiliation and to ensure its conduct in compliance with the protocol, informed consent, IRB/EC procedures, the Declaration of Helsinki, ICH Good Clinical Practices guideline, the EU directive Good Clinical Practice (2001-20-EG), and local regulations governing the conduct of clinical studies. -

Study Protocol
Clovis Oncology, Inc. Clinical Protocol Oral rucaparib (CO-338) CO-338-014 7 July 2016 CONFIDENTIAL A Multicenter, Randomized, Double-Blind, Placebo-Controlled Phase 3 Study of Rucaparib as Switch Maintenance Following Platinum-Based Chemotherapy in Patients with Platinum-Sensitive, High-Grade Serous or Endometrioid Epithelial Ovarian, Primary Peritoneal or Fallopian Tube Cancer Protocol Number: CO-338-014 Investigational Product: Rucaparib (CO-338) Eudra CT Number: IND Number: Development Phase: Phase 3 Indications Studied: Platinum-sensitive, high-grade serous and endometrioid epithelial ovarian, primary peritoneal, and fallopian tube cancer Sponsor Name and Address: Clovis Oncology, Inc. 5500 Flatiron Parkway Suite 100 Boulder, CO 80301 USA Phone Number: 303-625-5000 Facsimile Number: 303-245-0360 Responsible Medical Officer: Compliance Statement: This study will be conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki, clinical research guidelines established by the Code of Federal Regulations (Title 21, CFR Parts 50, 56, and 312), and ICH GCP Guidelines. Essential study documents will be archived in accordance with applicable regulations. CONFIDENTIALITY STATEMENT The information in this document contains commercial information and trade secrets that are privileged or confidential and may not be disclosed unless such disclosure is required by applicable laws and regulations. In any event, persons to whom the information is disclosed must be informed that the information is privileged or confidential and may not be further disclosed by them. These restrictions on disclosure will apply equally to all future information supplied to you which is indicated as privileged or confidential. 1 Clovis Oncology, Inc. Clinical Protocol Oral rucaparib (CO-338) CO-338-014 Coordinating Investigators for the Study Coordinating Investigator for North America: Coordinating Investigator for Europe, Middle East, and Asia Pacific: 2 Clovis Oncology, Inc. -

Multi-Discipline Review/Summary, Clinical, Non-Clinical
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209115Orig1s000 MULTI-DISCIPLINE REVIEW Summary / Clinical / Non-Clinical NDA/BLA Multi-disciplinary Review and Evaluation NDA 209115 Rubraca (rucaparib) 1 NDA/BLA Multi-disciplinary Review and Evaluation Application Type NDA Application Number(s) 209115 Priority or Standard Priority Submit Date(s) June 23, 2016 Received Date(s) June 23, 2016 PDUFA Goal Date February 23, 2017 Division/Office DOP1/OHOP Review Completion Date November 22, 2016 Established Name Rucaparib (Proposed) Trade Name RUBRACA Pharmacologic Class Poly (ADP-Ribose) Polymerase 1 inhibitor Code name AG-014669, PF-01367338, Applicant Clovis Oncology, Inc. Formulation(s) Oral tablet Dosing Regimen 600 mg PO BID Applicant Proposed Rubraca is indicated as monotherapy treatment of advanced ovarian Indication(s)/Population(s) cancer in patients with deleterious BRCA-mutated tumors, inclusive of both germline BRCA and somatic BRCA mutations (as detected by an FDA approved test), and who have been treated with two or more chemotherapies. Recommendation on Accelerated approval Regulatory Action Recommended Rubraca™ is indicated as monotherapy for the treatment of patients Indication(s)/Population(s) with deleterious BRCA mutation (germline and/or somatic) associated (if applicable) advanced ovarian cancer who have been treated with two or more chemotherapies. Select patients for therapy based on an FDA-approved companion diagnostic for Rubraca. 1-1 Version date: February 1, 2016 for initial rollout (NME/original BLA reviews) Reference ID: 40178304028244 NDA/BLA Multi-disciplinary Review and Evaluation NDA 209115 Rubraca (rucaparib) Contents 1 NDA/BLA Multi-disciplinary Review and Evaluation .......................................................................... 1-1 Reviewers of Multi-Disciplinary Review and Evaluation ........................................................................... -

PARP Inhibitors Sensitize Ewing Sarcoma Cells to Temozolomide
Published OnlineFirst October 5, 2015; DOI: 10.1158/1535-7163.MCT-15-0587 Cancer Biology and Signal Transduction Molecular Cancer Therapeutics PARP Inhibitors Sensitize Ewing Sarcoma Cells to Temozolomide-Induced Apoptosis via the Mitochondrial Pathway Florian Engert1, Cornelius Schneider1, Lilly Magdalena Weib1,2,3, Marie Probst1,and Simone Fulda1,2,3 Abstract Ewing sarcoma has recently been reported to be sensitive to that subsequent to DNA damage-imposed checkpoint activa- poly(ADP)-ribose polymerase (PARP) inhibitors. Searching for tion and G2 cell-cycle arrest, olaparib/TMZ cotreatment causes synergistic drug combinations, we tested several PARP inhibi- downregulation of the antiapoptotic protein MCL-1, followed by tors (talazoparib, niraparib, olaparib, veliparib) together with activation of the proapoptotic proteins BAX and BAK, mitochon- chemotherapeutics. Here, we report that PARP inhibitors syner- drial outer membrane permeabilization (MOMP), activation of gize with temozolomide (TMZ) or SN-38 to induce apoptosis caspases, and caspase-dependent cell death. Overexpression of a and also somewhat enhance the cytotoxicity of doxorubicin, nondegradable MCL-1 mutant or BCL-2, knockdown of NOXA or etoposide, or ifosfamide, whereas actinomycin D and vincris- BAX and BAK, or the caspase inhibitor N-benzyloxycarbonyl-Val- tine show little synergism. Furthermore, triple therapy of ola- Ala-Asp-fluoromethylketone (zVAD.fmk) all significantly reduce parib, TMZ, and SN-38 is significantly more effective compared olaparib/TMZ-mediated apoptosis. These findings emphasize with double or monotherapy. Mechanistic studies revealed that the role of PARP inhibitors for chemosensitization of Ewing the mitochondrial pathway of apoptosis plays a critical role in sarcoma with important implications for further (pre)clinical mediating the synergy of PARP inhibition and TMZ. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia
International Journal of Molecular Sciences Review The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia Marta Weronika Lato 1 , Anna Przysucha 1, Sylwia Grosman 1, Joanna Zawitkowska 2 and Monika Lejman 3,* 1 Student Scientific Society, Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] (M.W.L.); [email protected] (A.P.); [email protected] (S.G.) 2 Department of Pediatric Hematology, Oncology and Transplantology, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 3 Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland * Correspondence: [email protected] Abstract: Childhood acute lymphoblastic leukemia is a genetically heterogeneous cancer that ac- counts for 10–15% of T-cell acute lymphoblastic leukemia (T-ALL) cases. The T-ALL event-free survival rate (EFS) is 85%. The evaluation of structural and numerical chromosomal changes is important for a comprehensive biological characterization of T-ALL, but there are currently no ge- netic prognostic markers. Despite chemotherapy regimens, steroids, and allogeneic transplantation, relapse is the main problem in children with T-ALL. Due to the development of high-throughput molecular methods, the ability to define subgroups of T-ALL has significantly improved in the last few years. The profiling of the gene expression of T-ALL has led to the identification of T-ALL subgroups, and it is important in determining prognostic factors and choosing an appropriate treatment. Novel therapies targeting molecular aberrations offer promise in achieving better first remission with the Citation: Lato, M.W.; Przysucha, A.; hope of preventing relapse. -

Withdrawal Assessment Report - Orphan Maintenance
17 January 2019 EMA/22653/2019 Committee for Orphan Medicinal Products Withdrawal Assessment Report - Orphan Maintenance Rubraca (rucaparib) Treatment of ovarian cancer EU/3/12/1049 (EMA/OD/085/12) Sponsor: Clovis Oncology UK Limited Note Assessment report as adopted by the COMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2019. Reproduction is authorised provided the source is acknowledged Table of contents 1. Product and administrative information .................................................. 3 2. Grounds for the COMP opinion at the designation stage .......................... 5 3. Review of criteria for orphan designation at the time of type II variation .................................................................................................................... 5 Article 3(1)(a) of Regulation (EC) No 141/2000 .............................................................. 5 Article 3(1)(b) of Regulation (EC) No 141/2000 .............................................................. 6 4. COMP list of issues .................................................................................. 8 Withdrawal Assessment Report - Orphan Maintenance EMA/22653/2019 Page 2/8 1. Product and administrative information Product Active substance Rucaparib International Non-Proprietary -

Cancer Drug Pharmacology Table
CANCER DRUG PHARMACOLOGY TABLE Cytotoxic Chemotherapy Drugs are classified according to the BC Cancer Drug Manual Monographs, unless otherwise specified (see asterisks). Subclassifications are in brackets where applicable. Alkylating Agents have reactive groups (usually alkyl) that attach to Antimetabolites are structural analogues of naturally occurring molecules DNA or RNA, leading to interruption in synthesis of DNA, RNA, or required for DNA and RNA synthesis. When substituted for the natural body proteins. substances, they disrupt DNA and RNA synthesis. bendamustine (nitrogen mustard) azacitidine (pyrimidine analogue) busulfan (alkyl sulfonate) capecitabine (pyrimidine analogue) carboplatin (platinum) cladribine (adenosine analogue) carmustine (nitrosurea) cytarabine (pyrimidine analogue) chlorambucil (nitrogen mustard) fludarabine (purine analogue) cisplatin (platinum) fluorouracil (pyrimidine analogue) cyclophosphamide (nitrogen mustard) gemcitabine (pyrimidine analogue) dacarbazine (triazine) mercaptopurine (purine analogue) estramustine (nitrogen mustard with 17-beta-estradiol) methotrexate (folate analogue) hydroxyurea pralatrexate (folate analogue) ifosfamide (nitrogen mustard) pemetrexed (folate analogue) lomustine (nitrosurea) pentostatin (purine analogue) mechlorethamine (nitrogen mustard) raltitrexed (folate analogue) melphalan (nitrogen mustard) thioguanine (purine analogue) oxaliplatin (platinum) trifluridine-tipiracil (pyrimidine analogue/thymidine phosphorylase procarbazine (triazine) inhibitor) -

ARIEL4: an International, Randomised Phase 3 Study Of
ARIEL4: An International, Randomised Phase 3 Study of Rucaparib vs Chemotherapy in BRCA1- or BRCA2-Mutated, Abstract ESGO7-0665 Relapsed Ovarian Cancer (OC) Rebecca S. Kristeleit,1 Domenica Lorusso,2 Ana Oaknin,3 Tamar Safra,4 Elizabeth M. Swisher,5 Igor M. Bondarenko,6 Tomasz Huzarski,7 Jaroslav Klat,8 Vladimir Moiseyenko,9 Róbert Póka,10 Luciana S. Viola,11 Chris Tankersley,12 Lara Maloney,12 Sandra Goble,12 Caro Unger,12 Adam Dowson,12 Heidi Giordano,12 Amit M. Oza13 1University College London Cancer Institute, London, UK; 2MITO and Unità di Ginecologia Oncologica, Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy; 3Vall d’Hebron University Hospital, Vall d’Hebron Institute of Oncology (VHIO), Barcelona, Spain; 4Sackler School of Medicine, Tel Aviv University and Tel Aviv Sourasky Medical Center, Tel Aviv, Israel; 5University of Washington, Seattle, WA, USA; 6Dnipropetrovsk Medical Academy, City Multiple-Discipline Clinical Hospital, Dnipropetrovsk, Ukraine; 7Private Health Care Innovative Medicine, Grzepnica, Poland; 8University Hospital Ostrava, Ostrava, Czech Republic; 9NN. Petrov Research Institute of Oncology Cancer Center, St. Petersburg, Russian Federation; 10Debrecen University Clinical Center, Debrecen, Hungary; 11Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil; 12Clovis Oncology, Inc., Boulder, CO, USA; 13Princess Margaret Cancer Centre, University Health Network, Toronto, ON, Canada INTRODUCTION • In high-grade OC, including fallopian tube and primary peritoneal cancer, ≈18% and ≈7% of -
Draft Matrix Post Referral PDF 189 KB
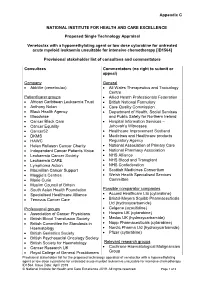
Appendix C NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Proposed Single Technology Appraisal Venetoclax with a hypomethylating agent or low dose cytarabine for untreated acute myeloid leukaemia unsuitable for intensive chemotherapy [ID1564] Provisional stakeholder list of consultees and commentators Consultees Commentators (no right to submit or appeal) Company General • AbbVie (venetoclax) • All Wales Therapeutics and Toxicology Centre Patient/carer groups • Allied Health Professionals Federation • African Caribbean Leukaemia Trust • British National Formulary • Anthony Nolan • Care Quality Commission • Black Health Agency • Department of Health, Social Services • Bloodwise and Public Safety for Northern Ireland • Cancer Black Care • Hospital Information Services – • Cancer Equality Jehovah’s Witnesses • Cancer52 • Healthcare Improvement Scotland • DKMS • Medicines and Healthcare products • HAWC Regulatory Agency • Helen Rollason Cancer Charity • National Association of Primary Care • Independent Cancer Patients Voice • National Pharmacy Association • Leukaemia Cancer Society • NHS Alliance • Leukaemia CARE • NHS Blood and Transplant • Lymphoma Action • NHS Confederation • Macmillan Cancer Support • Scottish Medicines Consortium • Maggie’s Centres • Welsh Health Specialised Services • Marie Curie Committee • Muslim Council of Britain • South Asian Health Foundation Possible comparator companies • Specialised Healthcare Alliance • Accord Healthcare Ltd (cytarabine) • Tenovus Cancer Care • Bristol-Meyers Squibb Pharmaceuticals Ltd -

A Novel CDK9 Inhibitor Increases the Efficacy of Venetoclax (ABT-199) in Multiple Models of Hematologic Malignancies
Leukemia (2020) 34:1646–1657 https://doi.org/10.1038/s41375-019-0652-0 ARTICLE Molecular targets for therapy A novel CDK9 inhibitor increases the efficacy of venetoclax (ABT-199) in multiple models of hematologic malignancies 1 1 2,3 4 1 5 6 Darren C. Phillips ● Sha Jin ● Gareth P. Gregory ● Qi Zhang ● John Xue ● Xiaoxian Zhao ● Jun Chen ● 1 1 1 1 1 1 Yunsong Tong ● Haichao Zhang ● Morey Smith ● Stephen K. Tahir ● Rick F. Clark ● Thomas D. Penning ● 2,7 3 5 1 4 2,7 Jennifer R. Devlin ● Jake Shortt ● Eric D. Hsi ● Daniel H. Albert ● Marina Konopleva ● Ricky W. Johnstone ● 8 1 Joel D. Leverson ● Andrew J. Souers Received: 27 November 2018 / Revised: 18 October 2019 / Accepted: 13 November 2019 / Published online: 11 December 2019 © The Author(s) 2019 Abstract MCL-1 is one of the most frequently amplified genes in cancer, facilitating tumor initiation and maintenance and enabling resistance to anti-tumorigenic agents including the BCL-2 selective inhibitor venetoclax. The expression of MCL-1 is maintained via P-TEFb-mediated transcription, where the kinase CDK9 is a critical component. Consequently, we developed a series of potent small-molecule inhibitors of CDK9, exemplified by the orally active A-1592668, with CDK selectivity profiles 1234567890();,: 1234567890();,: that are distinct from related molecules that have been extensively studied clinically. Short-term treatment with A-1592668 rapidly downregulates RNA pol-II (Ser 2) phosphorylation resulting in the loss of MCL-1 protein and apoptosis in MCL-1- dependent hematologic tumor cell lines. This cell death could be attenuated by either inhibiting caspases or overexpressing BCL-2 protein. -
Management of Multiple Myeloma: the Changing Paradigm
Management of Multiple Myeloma: The Changing Paradigm Relapsed/Refractory Disease Jeffrey A. Zonder, MD Karmanos Cancer Institute Objectives • Discuss use of standard myeloma therapies when used as therapy after relapse • Consider patient and disease factors which might impact therapy decisions. • Describe off-label options for patients who are not protocol candidates. Line ≠ Line ≠ Line ≠ … POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLI LINE – DO NOT Define “Line” • A pre-defined course of therapy utilizing agents either simultaneously or sequentially – Len/Dex – Len/Dex ASCT – Vel/Dex ASCT Len/Dex – VDT-PACE ASCT TD ASCT VPT-PACE LD • Pts who have had the same # of “lines” of Rx may have had vastly different amounts of Rx What Is Relapsed/Refractory Disease? • Relapsed: recurrence after a response to therapy • Refractory: progression despite ongoing therapy What Do We Know About the Pt’s Myeloma? • What prior therapy has been used? • How well did it work? • Did the myeloma progress on active therapy? • High-risk cytogenetics/FISH/GEP? What Do We Know About the Patient? • Age • Other medical problems – Diabetes – Blood Clots • Lasting side effects from past therapies – Peripheral Neuropathy • Personal preferences and values Choosing Therapy for Relapsed/Refractory Myeloma Proteasome IMiDs Anthracyclines Alkylators Steroids HDACs Antibodies Inhibitors Thalidomide Bortezomib Doxil Melphalan Dex Panobinostat Elotuzumab Lenalidomide Carfilzomib Cytoxan Pred Vorinostat