Table S1. Clinical Trials Implicating Galectins As Biomarkers (1)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Prospective, Multicenter, Phase-II Trial of Ibrutinib Plus Venetoclax In
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 A prospective, multicenter, phase-II trial of ibrutinib plus venetoclax in patients with creatinine clearance ≥ 30 ml/min who have relapsed or refractory chronic lymphocytic leukemia (RR-CLL) with or without TP53 aberrations HOVON 141 CLL / VIsion Trial of the HOVON and Nordic CLL study groups PROTOCOL Principal Investigator : Arnon P Kater (HOVON) Carsten U Niemann (Nordic CLL study Group)) Sponsor : HOVON EudraCT number : 2016-002599-29 ; Page 1 of 107 Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Levin M-D, et al. BMJ Open 2020; 10:e039168. doi: 10.1136/bmjopen-2020-039168 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open HOVON 141 CLL Version 4, 20 DEC 2018 LOCAL INVESTIGATOR SIGNATURE PAGE Local site name: Signature of Local Investigator Date Printed Name of Local Investigator By my signature, I agree to personally supervise the conduct of this study in my affiliation and to ensure its conduct in compliance with the protocol, informed consent, IRB/EC procedures, the Declaration of Helsinki, ICH Good Clinical Practices guideline, the EU directive Good Clinical Practice (2001-20-EG), and local regulations governing the conduct of clinical studies. -

PARP Inhibitors Sensitize Ewing Sarcoma Cells to Temozolomide
Published OnlineFirst October 5, 2015; DOI: 10.1158/1535-7163.MCT-15-0587 Cancer Biology and Signal Transduction Molecular Cancer Therapeutics PARP Inhibitors Sensitize Ewing Sarcoma Cells to Temozolomide-Induced Apoptosis via the Mitochondrial Pathway Florian Engert1, Cornelius Schneider1, Lilly Magdalena Weib1,2,3, Marie Probst1,and Simone Fulda1,2,3 Abstract Ewing sarcoma has recently been reported to be sensitive to that subsequent to DNA damage-imposed checkpoint activa- poly(ADP)-ribose polymerase (PARP) inhibitors. Searching for tion and G2 cell-cycle arrest, olaparib/TMZ cotreatment causes synergistic drug combinations, we tested several PARP inhibi- downregulation of the antiapoptotic protein MCL-1, followed by tors (talazoparib, niraparib, olaparib, veliparib) together with activation of the proapoptotic proteins BAX and BAK, mitochon- chemotherapeutics. Here, we report that PARP inhibitors syner- drial outer membrane permeabilization (MOMP), activation of gize with temozolomide (TMZ) or SN-38 to induce apoptosis caspases, and caspase-dependent cell death. Overexpression of a and also somewhat enhance the cytotoxicity of doxorubicin, nondegradable MCL-1 mutant or BCL-2, knockdown of NOXA or etoposide, or ifosfamide, whereas actinomycin D and vincris- BAX and BAK, or the caspase inhibitor N-benzyloxycarbonyl-Val- tine show little synergism. Furthermore, triple therapy of ola- Ala-Asp-fluoromethylketone (zVAD.fmk) all significantly reduce parib, TMZ, and SN-38 is significantly more effective compared olaparib/TMZ-mediated apoptosis. These findings emphasize with double or monotherapy. Mechanistic studies revealed that the role of PARP inhibitors for chemosensitization of Ewing the mitochondrial pathway of apoptosis plays a critical role in sarcoma with important implications for further (pre)clinical mediating the synergy of PARP inhibition and TMZ. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia
International Journal of Molecular Sciences Review The New Therapeutic Strategies in Pediatric T-Cell Acute Lymphoblastic Leukemia Marta Weronika Lato 1 , Anna Przysucha 1, Sylwia Grosman 1, Joanna Zawitkowska 2 and Monika Lejman 3,* 1 Student Scientific Society, Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] (M.W.L.); [email protected] (A.P.); [email protected] (S.G.) 2 Department of Pediatric Hematology, Oncology and Transplantology, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 3 Laboratory of Genetic Diagnostics, Medical University of Lublin, 20-093 Lublin, Poland * Correspondence: [email protected] Abstract: Childhood acute lymphoblastic leukemia is a genetically heterogeneous cancer that ac- counts for 10–15% of T-cell acute lymphoblastic leukemia (T-ALL) cases. The T-ALL event-free survival rate (EFS) is 85%. The evaluation of structural and numerical chromosomal changes is important for a comprehensive biological characterization of T-ALL, but there are currently no ge- netic prognostic markers. Despite chemotherapy regimens, steroids, and allogeneic transplantation, relapse is the main problem in children with T-ALL. Due to the development of high-throughput molecular methods, the ability to define subgroups of T-ALL has significantly improved in the last few years. The profiling of the gene expression of T-ALL has led to the identification of T-ALL subgroups, and it is important in determining prognostic factors and choosing an appropriate treatment. Novel therapies targeting molecular aberrations offer promise in achieving better first remission with the Citation: Lato, M.W.; Przysucha, A.; hope of preventing relapse. -

Cancer Drug Pharmacology Table
CANCER DRUG PHARMACOLOGY TABLE Cytotoxic Chemotherapy Drugs are classified according to the BC Cancer Drug Manual Monographs, unless otherwise specified (see asterisks). Subclassifications are in brackets where applicable. Alkylating Agents have reactive groups (usually alkyl) that attach to Antimetabolites are structural analogues of naturally occurring molecules DNA or RNA, leading to interruption in synthesis of DNA, RNA, or required for DNA and RNA synthesis. When substituted for the natural body proteins. substances, they disrupt DNA and RNA synthesis. bendamustine (nitrogen mustard) azacitidine (pyrimidine analogue) busulfan (alkyl sulfonate) capecitabine (pyrimidine analogue) carboplatin (platinum) cladribine (adenosine analogue) carmustine (nitrosurea) cytarabine (pyrimidine analogue) chlorambucil (nitrogen mustard) fludarabine (purine analogue) cisplatin (platinum) fluorouracil (pyrimidine analogue) cyclophosphamide (nitrogen mustard) gemcitabine (pyrimidine analogue) dacarbazine (triazine) mercaptopurine (purine analogue) estramustine (nitrogen mustard with 17-beta-estradiol) methotrexate (folate analogue) hydroxyurea pralatrexate (folate analogue) ifosfamide (nitrogen mustard) pemetrexed (folate analogue) lomustine (nitrosurea) pentostatin (purine analogue) mechlorethamine (nitrogen mustard) raltitrexed (folate analogue) melphalan (nitrogen mustard) thioguanine (purine analogue) oxaliplatin (platinum) trifluridine-tipiracil (pyrimidine analogue/thymidine phosphorylase procarbazine (triazine) inhibitor) -
Draft Matrix Post Referral PDF 189 KB
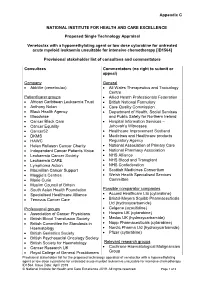
Appendix C NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Proposed Single Technology Appraisal Venetoclax with a hypomethylating agent or low dose cytarabine for untreated acute myeloid leukaemia unsuitable for intensive chemotherapy [ID1564] Provisional stakeholder list of consultees and commentators Consultees Commentators (no right to submit or appeal) Company General • AbbVie (venetoclax) • All Wales Therapeutics and Toxicology Centre Patient/carer groups • Allied Health Professionals Federation • African Caribbean Leukaemia Trust • British National Formulary • Anthony Nolan • Care Quality Commission • Black Health Agency • Department of Health, Social Services • Bloodwise and Public Safety for Northern Ireland • Cancer Black Care • Hospital Information Services – • Cancer Equality Jehovah’s Witnesses • Cancer52 • Healthcare Improvement Scotland • DKMS • Medicines and Healthcare products • HAWC Regulatory Agency • Helen Rollason Cancer Charity • National Association of Primary Care • Independent Cancer Patients Voice • National Pharmacy Association • Leukaemia Cancer Society • NHS Alliance • Leukaemia CARE • NHS Blood and Transplant • Lymphoma Action • NHS Confederation • Macmillan Cancer Support • Scottish Medicines Consortium • Maggie’s Centres • Welsh Health Specialised Services • Marie Curie Committee • Muslim Council of Britain • South Asian Health Foundation Possible comparator companies • Specialised Healthcare Alliance • Accord Healthcare Ltd (cytarabine) • Tenovus Cancer Care • Bristol-Meyers Squibb Pharmaceuticals Ltd -

A Novel CDK9 Inhibitor Increases the Efficacy of Venetoclax (ABT-199) in Multiple Models of Hematologic Malignancies
Leukemia (2020) 34:1646–1657 https://doi.org/10.1038/s41375-019-0652-0 ARTICLE Molecular targets for therapy A novel CDK9 inhibitor increases the efficacy of venetoclax (ABT-199) in multiple models of hematologic malignancies 1 1 2,3 4 1 5 6 Darren C. Phillips ● Sha Jin ● Gareth P. Gregory ● Qi Zhang ● John Xue ● Xiaoxian Zhao ● Jun Chen ● 1 1 1 1 1 1 Yunsong Tong ● Haichao Zhang ● Morey Smith ● Stephen K. Tahir ● Rick F. Clark ● Thomas D. Penning ● 2,7 3 5 1 4 2,7 Jennifer R. Devlin ● Jake Shortt ● Eric D. Hsi ● Daniel H. Albert ● Marina Konopleva ● Ricky W. Johnstone ● 8 1 Joel D. Leverson ● Andrew J. Souers Received: 27 November 2018 / Revised: 18 October 2019 / Accepted: 13 November 2019 / Published online: 11 December 2019 © The Author(s) 2019 Abstract MCL-1 is one of the most frequently amplified genes in cancer, facilitating tumor initiation and maintenance and enabling resistance to anti-tumorigenic agents including the BCL-2 selective inhibitor venetoclax. The expression of MCL-1 is maintained via P-TEFb-mediated transcription, where the kinase CDK9 is a critical component. Consequently, we developed a series of potent small-molecule inhibitors of CDK9, exemplified by the orally active A-1592668, with CDK selectivity profiles 1234567890();,: 1234567890();,: that are distinct from related molecules that have been extensively studied clinically. Short-term treatment with A-1592668 rapidly downregulates RNA pol-II (Ser 2) phosphorylation resulting in the loss of MCL-1 protein and apoptosis in MCL-1- dependent hematologic tumor cell lines. This cell death could be attenuated by either inhibiting caspases or overexpressing BCL-2 protein. -

New Drug Update: the Next Step in Personalized Medicine
New Drug Update: The Next Step in Personalized Medicine Jordan Hill, PharmD, BCOP Clinical Pharmacy Specialist WVU Medicine Mary Babb Randolph Cancer Center Objectives • Review indications for new FDA approved anti- neoplastic medications in 2017 • Outline place in therapy of new medications • Become familiar with mechanisms of action of new medications • Describe adverse effects associated with new medications • Summarize dosing schemes and appropriate dose reductions for new medications First-in-Class Approvals • FLT3 inhibitor – midostaurin • IDH2 inhibitor – enasidenib • Anti-CD22 antibody drug conjugate – inotuzumab ozogamicin • CAR T-cell therapy - tisagenlecleucel “Me-too” Approvals • CDK 4/6 inhibitor – ribociclib and abemaciclib • PD-L1 inhibitors • Avelumab • Durvalumab • PARP inhibitor – niraparib • ALK inhibitor – brigatinib • Pan-HER inhibitor – neratinib • Liposome-encapsulated combination of daunorubicin and cytarabine • PI3K inhibitor – copanlisib Drugs by Malignancy AML Breast Bladder ALL FL Lung Ovarian 0 1 2 3 Oral versus IV 46% 54% Oral IV FIRST-IN CLASS FLT3 Inhibitor - midostaurin Journal of Hematology & Oncology 2017;10:93 Midostaurin (Rydapt®) • 717 newly diagnosed FLT3+ AML Patients • Induction and consolidation chemotherapy and placebo maintenance versus chemotherapy + midostaurin and Treatment maintenance midostaurin • OS: 74.7 mo versus 25.6 mo (P=0.009) Efficacy • EFS: 8.2 mo versus 3.0 mo (P=0.002) • Higher grade > 3 anemia, rash, and nausea Safety N Engl J Med 2017;377:454-64 Midostaurin (Rydapt®) • Approved indications: FLT3+ AML, mast cell leukemia, systemic mastocytosis • AML dose: 50 mg twice daily with food on days 8-21 • Of each induction cycle (+ daunorubicin and cytarabine) • Of each consolidation cycle (+ high dose cytarabine) • ADEs: nausea, myelosuppression, mucositis, increases in LFTs, amylase/lipase, and electrolyte abnormalities • Pharmacokinetics: hepatic metabolism, substrate of CYP 3A4; < 5% excretion in urine RYDAPT (midostaurin) [package insert]. -

Olaparib and Temozolomide in SCLC
Olaparib and temozolomide in SCLC Anna Farago, MD, PhD and Benjamin Drapkin, MD, PhD March 16, 2018 Disclosures Farago: • Consulting fees from: PharmaMar, AbbVie, Takeda, Merrimack, Loxo Oncology • Honorarium from: Foundation Medicine • Research funding (to institution) from: AstraZeneca, AbbVie, Novartis, PharmaMar, Loxo Oncology, Ignyta, Merck, Bristol-Myers Squibb Drapkin: • Research funding (to institution) from: AstraZeneca, AbbVie, Novartis Bedside to Bench… and Back PARP inhibition in SCLC • PARP1 regulates base excision repair, homologous recombination, and non-homologous end joining. Inhibition of PARP enzymatic activity blocks PARP-mediated DNA repair.1 • PARP1 is highly expressed in SCLC compared to other cancers.2, 3 • SCLC cell lines are sensitive to PARP inhibitors. PARP sensitivity is not associated with BRCA1/2 mutations or HR defects.4,5 • “Trapping” of PARP complexes to sites of DNA single stranded breaks by PARP inhibitors can cause failure of repair and induction of double strand breaks.6 1. Sonnenblick et al., 2015 • PARP inhibitors synergize with agents that increase prevalence of 2. Byers et al., 2012 3. Cardnell et al., 2013 7,8 single stranded breaks in tumor models, including SCLC models. 4. Stewart et al., 2017 5. George et al., 2015 6. Hopkins et al., 2015 7. Murai et al., 2014 8. Lok et al., 2016 Farago et al., Presented at AACR annual meeting 2017 Rationale for olaparib + temozolomide in relapsed SCLC • Catalytic inhibitor of PARP1 and • Alkylating agent that induces Olaparib PARP2 Temozolomide single strand DNA breaks • Moderate PARP-trapping activity1 • FDA-approved in newly • FDA-approved as monotherapy for diagnosed glioblastoma patients with BRCA-mutated multiforme and refractory advanced ovarian cancer and for anaplastic astrocytoma patients with germline BRCA-mutated • Single agent activity in SCLC2 breast cancer • STOMP UK trial: Maintenance olaparib vs placebo following first-line chemotherapy. -

Targeting NAD+ Biosynthesis Overcomes Panobinostat and Bortezomib-Induced Malignant
Author Manuscript Published OnlineFirst on April 1, 2020; DOI: 10.1158/1541-7786.MCR-19-0669 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Targeting NAD+ biosynthesis overcomes panobinostat and bortezomib-induced malignant glioma resistance Esther P. Jane, 1, 2 Daniel R. Premkumar, 1, 2, 3 Swetha Thambireddy, 1 Brian Golbourn, 1 Sameer Agnihotri, 1, 2, 3 Kelsey C. Bertrand, 4 Stephen C. Mack, 4 Max I. Myers, 1 Ansuman Chattopadhyay, 5 D. Lansing Taylor, 6, 7, 8 Mark E. Schurdak, 6, 7, 8 Andrew M. Stern, 7, 8 and Ian F. Pollack 1, 2, 3 Department of Neurosurgery 1, University of Pittsburgh School of Medicine 2, University of Pittsburgh Cancer Institute Brain Tumor Center 3, Texas Children's Hospital, Baylor College of Medicine 4, University of Pittsburgh Molecular Biology Information Service 5, University of Pittsburgh Cancer Institute 6, University of Pittsburgh Drug Discovery Institute 7, Department of Computational and Systems Biology, University of Pittsburgh School of Medicine 8, Pittsburgh, Pennsylvania, U.S.A. Disclosure of Potential Conflict of Interest The authors have declared that no conflict of interest exists. 1 Downloaded from mcr.aacrjournals.org on October 2, 2021. © 2020 American Association for Cancer Research. Author Manuscript Published OnlineFirst on April 1, 2020; DOI: 10.1158/1541-7786.MCR-19-0669 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Keywords: Panobinostat, bortezomib, synergy, resistance, glioma, -

Phenotype-Based Drug Screening Reveals Association Between Venetoclax Response and Differentiation Stage in Acute Myeloid Leukemia
Acute Myeloid Leukemia SUPPLEMENTARY APPENDIX Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia Heikki Kuusanmäki, 1,2 Aino-Maija Leppä, 1 Petri Pölönen, 3 Mika Kontro, 2 Olli Dufva, 2 Debashish Deb, 1 Bhagwan Yadav, 2 Oscar Brück, 2 Ashwini Kumar, 1 Hele Everaus, 4 Bjørn T. Gjertsen, 5 Merja Heinäniemi, 3 Kimmo Porkka, 2 Satu Mustjoki 2,6 and Caroline A. Heckman 1 1Institute for Molecular Medicine Finland, Helsinki Institute of Life Science, University of Helsinki, Helsinki; 2Hematology Research Unit, Helsinki University Hospital Comprehensive Cancer Center, Helsinki; 3Institute of Biomedicine, School of Medicine, University of Eastern Finland, Kuopio, Finland; 4Department of Hematology and Oncology, University of Tartu, Tartu, Estonia; 5Centre for Cancer Biomarkers, De - partment of Clinical Science, University of Bergen, Bergen, Norway and 6Translational Immunology Research Program and Department of Clinical Chemistry and Hematology, University of Helsinki, Helsinki, Finland ©2020 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2018.214882 Received: December 17, 2018. Accepted: July 8, 2019. Pre-published: July 11, 2019. Correspondence: CAROLINE A. HECKMAN - [email protected] HEIKKI KUUSANMÄKI - [email protected] Supplemental Material Phenotype-based drug screening reveals an association between venetoclax response and differentiation stage in acute myeloid leukemia Authors: Heikki Kuusanmäki1, 2, Aino-Maija -

Sorafenib and Omacetaxine Mepesuccinate As a Safe and Effective Treatment for Acute Myeloid Leukemia Carrying Internal Tandem Du
Original Article Sorafenib and Omacetaxine Mepesuccinate as a Safe and Effective Treatment for Acute Myeloid Leukemia Carrying Internal Tandem Duplication of Fms-Like Tyrosine Kinase 3 Chunxiao Zhang, MSc1; Stephen S. Y. Lam, MBBS, PhD1; Garret M. K. Leung, MBBS1; Sze-Pui Tsui, MSc2; Ning Yang, PhD1; Nelson K. L. Ng, PhD1; Ho-Wan Ip, MBBS2; Chun-Hang Au, PhD3; Tsun-Leung Chan, PhD3; Edmond S. K. Ma, MBBS3; Sze-Fai Yip, MBBS4; Harold K. K. Lee, MBChB5; June S. M. Lau, MBChB6; Tsan-Hei Luk, MBChB6; Wa Li, MBChB7; Yok-Lam Kwong, MD 1; and Anskar Y. H. Leung, MD, PhD 1 BACKGROUND: Omacetaxine mepesuccinate (OME) has antileukemic effects against acute myeloid leukemia (AML) carrying an internal tandem duplication of Fms-like tyrosine kinase 3 (FLT3-ITD). A phase 2 clinical trial was conducted to evaluate a combina- tion treatment of sorafenib and omacetaxine mepesuccinate (SOME). METHODS: Relapsed or refractory (R/R) or newly diagnosed patients were treated with sorafenib (200-400 mg twice daily) and OME (2 mg daily) for 7 (first course) or 5 days (second course on- ward) every 21 days until disease progression or allogeneic hematopoietic stem cell transplantation (HSCT). The primary endpoint was composite complete remission, which was defined as complete remission (CR) plus complete remission with incomplete hematologic recovery (CRi). Secondary endpoints were leukemia-free survival (LFS) and overall survival (OS). RESULTS: Thirty-nine R/R patients and 5 newly diagnosed patients were recruited. Among the R/R patients, 28 achieved CR or CRi. Two patients showed partial remission, and 9 patients did not respond.