Alcohol Dependence in Rats Is Associated with Global Changes in Gene Expression in the Central Amygdala
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nuclear Matrix Metalloproteinases: Functions Resemble the Evolution from the Intracellular to the Extracellular Compartment
OPEN Citation: Cell Death Discovery (2017) 3, 17036; doi:10.1038/cddiscovery.2017.36 Official journal of the Cell Death Differentiation Association www.nature.com/cddiscovery REVIEW Nuclear matrix metalloproteinases: functions resemble the evolution from the intracellular to the extracellular compartment Yingqiu Xie1,2,5, Aidana Mustafa1,5, Adina Yerzhan1,5, Dalmira Merzhakupova1, Perizat Yerlan1, Askarbek N Orakov1, Xiao Wang3, Yi Huang4 and Lixia Miao2 Matrix metalloproteinase (MMP) is defined as an endopeptidase in the extracellular matrix (ECM), which plays essential roles in physiological processes such as organogenesis, wound healing, angiogenesis, apoptosis and motility. MMPs are produced and assembled in the cytoplasm as proenzymes with a cytoplasmic domain and require extracellular activation. MMPs can degrade receptors, extracellular matrix proteins, PARPs and release apoptotic substances. MMPs have been found in the cytosol, organelles and extracellular compartments and recently many types of MMPs have been found in the nucleus. However, the mechanisms and roles of MMPs inside the cell nucleus are still poorly understood. Here we summarized the nuclear localization mechanisms of MMPs and their functions in the nucleus such as apoptosis, tissue remodeling upon injury and cancer progression. Most importantly, we found that nuclear MMPs have evolved to translocate to membrane and target ECM possibly through evolution of nuclear localization signal (NLS), natural selection and anti-apoptotic survival. Thus, the knowledge about the evolution and regulation of nuclear MMPs appears to be essential in understanding a variety of cellular processes along with the development of MMP-targeted therapeutic drugs against the progression of certain diseases. Cell Death Discovery (2017) 3, 17036; doi:10.1038/cddiscovery.2017.36; published online 14 August 2017 KEY FACTS MMP-10, MMP-13 and MMP-14. -
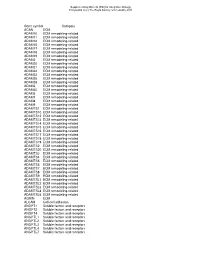
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Extracellular Matrix Alterations in Metastatic Processes
International Journal of Molecular Sciences Review Extracellular Matrix Alterations in Metastatic Processes Mayra Paolillo * and Sergio Schinelli Department of Drug Sciences, University of Pavia, 27100 Pavia, Italy; [email protected] * Correspondence: [email protected] Received: 17 September 2019; Accepted: 30 September 2019; Published: 7 October 2019 Abstract: The extracellular matrix (ECM) is a complex network of extracellular-secreted macromolecules, such as collagen, enzymes and glycoproteins, whose main functions deal with structural scaffolding and biochemical support of cells and tissues. ECM homeostasis is essential for organ development and functioning under physiological conditions, while its sustained modification or dysregulation can result in pathological conditions. During cancer progression, epithelial tumor cells may undergo epithelial-to-mesenchymal transition (EMT), a morphological and functional remodeling, that deeply alters tumor cell features, leading to loss of epithelial markers (i.e., E-cadherin), changes in cell polarity and intercellular junctions and increase of mesenchymal markers (i.e., N-cadherin, fibronectin and vimentin). This process enhances cancer cell detachment from the original tumor mass and invasiveness, which are necessary for metastasis onset, thus allowing cancer cells to enter the bloodstream or lymphatic flow and colonize distant sites. The mechanisms that lead to development of metastases in specific sites are still largely obscure but modifications occurring in target tissue ECM are being intensively studied. Matrix metalloproteases and several adhesion receptors, among which integrins play a key role, are involved in metastasis-linked ECM modifications. In addition, cells involved in the metastatic niche formation, like cancer associated fibroblasts (CAF) and tumor associated macrophages (TAM), have been found to play crucial roles in ECM alterations aimed at promoting cancer cells adhesion and growth. -
Ultra-Processed Food Targets Bone Quality Via Endochondral Ossification
Bone Research www.nature.com/boneres ARTICLE OPEN Ultra-processed food targets bone quality via endochondral ossification Janna Zaretsky1, Shelley Griess-Fishheimer1, Adi Carmi1, Tamara Travinsky Shmul1, Lior Ofer2, Tali Sinai1, Svetlana Penn1, Ron Shahar2 and Efrat Monsonego-Ornan 1 Ultra-processed foods have known negative implications for health; however, their effect on skeletal development has never been explored. Here, we show that young rats fed ultra-processed food rich in fat and sugar suffer from growth retardation due to lesions in their tibial growth plates. The bone mineral density decreases significantly, and the structural parameters of the bone deteriorate, presenting a sieve-like appearance in the cortices and poor trabecular parameters in long bones and vertebrae. This results in inferior mechanical performance of the entire bone with a high fracture risk. RNA sequence analysis of the growth plates demonstrated an imbalance in extracellular matrix formation and degradation and impairment of proliferation, differentiation and mineralization processes. Our findings highlight, for the first time, the severe impact of consuming ultra-processed foods on the growing skeleton. This pathology extends far beyond that explained by the known metabolic effects, highlighting bone as a new target for studies of modern diets. Bone Research (2021) ;9:14 https://doi.org/10.1038/s41413-020-00127-9 1234567890();,: INTRODUCTION penetration of blood vessels and bone tissue formation by The vertebrate skeleton has evolved as a dynamic system that osteoblasts.1,2,4,6 The EO process is tightly orchestrated by various serves numerous functions, such as protecting internal organs, signaling molecules and transcription factors, including transform- creating attachment sites for muscles to produce locomotion, ing growth factor β/bone morphogenetic protein (BMP), fibroblast providing a reservoir for minerals, and serving as a hematopoietic growth factor (FGF), Wnt, hedgehog, and the transcription factor niche. -

Mapping Transmembrane Binding Partners for E-Cadherin Ectodomains
Mapping transmembrane binding partners for E-cadherin ectodomains Omer Shafraza, Bin Xieb, Soichiro Yamadaa, and Sanjeevi Sivasankara,b,1 aDepartment of Biomedical Engineering, University of California, Davis, CA 95616; and bBiophysics Graduate Group, University of California, Davis, CA 95616 Edited by Barry Honig, Howard Hughes Medical Institute, Columbia University, New York, NY, and approved October 28, 2020 (received for review May 22, 2020) We combine proximity labeling and single molecule binding assays proteins that directly interact with a transmembrane bait would to discover transmembrane protein interactions in cells. We first be positioned in close proximity to both the bait’s ectodomain screen for candidate binding partners by tagging the extracellular and cytoplasmic regions. Consequently, if the proximity-based and cytoplasmic regions of a “bait” protein with BioID biotin ligase labeling enzyme was fused to both the bait’s extracellular and and identify proximal proteins that are biotin tagged on both their cytoplasmic regions, identifying transmembrane proteins that extracellular and intracellular regions. We then test direct binding are biotinylated in both regions would enable us to narrow interactions between proximal proteins and the bait, using single down the list of possible binding partners for subsequent AFM molecule atomic force microscope binding assays. Using this ap- binding measurements. Furthermore, an integrated extracellu- proach, we identify binding partners for the extracellular region lar and cytoplasmic BioID measurement would significantly of E-cadherin, an essential cell–cell adhesion protein. We show that increase the precision of the screen by dramatically reducing the desmosomal proteins desmoglein-2 and desmocollin-3, the focal the number of false positive hits. -

Functional Roles of MMP14 and MMP15 in Early Postnatal Mammary Gland Development Tamar Y
© 2016. Published by The Company of Biologists Ltd | Development (2016) 143, 3956-3968 doi:10.1242/dev.136259 RESEARCH ARTICLE Functional roles of MMP14 and MMP15 in early postnatal mammary gland development Tamar Y. Feinberg1,2,3, R. Grant Rowe1,*, Thomas L. Saunders1,4 and Stephen J. Weiss1,2,3,‡ ABSTRACT with epithelial development, the surrounding adipose-rich tissue, During late embryogenesis, mammary epithelial cells initiate migration termed the mammary fat pad, likewise undergoes morphogenesis programs that drive ductal invasion into the surrounding adipose-rich (Hovey and Aimo, 2010; Inman et al., 2015). Beginning during late mesenchyme. Currently, branching morphogenesis is thought to gestation (E14 to E18) and continuing through early postnatal depend on the mobilization of the membrane-anchored matrix development, the fat pad is eventually dominated by committed metalloproteinases MMP14 (MT1-MMP) and MMP15 (MT2-MMP), adipocytes that support epithelial morphogenesis and tissue which drive epithelial cell invasion by remodeling the extracellular homeostasis (Wang et al., 2015). At birth, the mammary gland matrix and triggering associated signaling cascades. However, the rudiment is a small, simply branched structure that is believed to lie ∼ roles that these proteinases play during mammary gland development dormant until the onset of puberty ( 3 weeks of age) (Ewald et al., in vivo remain undefined. Here, we characterize the impact of global 2008, 2012; Hogg et al., 1983; Watson and Khaled, 2008). Mmp14 and Mmp15 targeting on early postnatal mammary gland Recent studies emphasize crucial roles for proteolytic enzymes development in mice. Unexpectedly, both Mmp14−/− and Mmp15−/− belonging to the matrix metalloproteinase (MMP) family in the tissue mammary glands retain the ability to generate intact ductal networks. -

Supplement Data Supplemental Table 1. Stem-Loop Structure
Supplement Data Supplemental Table 1. Stem-loop structure oligonucleotide sequences. tgctgttgacagtgagcgaccagatacctgcaccaccttatagtgaagccacagatgtataaggt MMP2 ggtgcaggtatctgggtgcctactgcctcgga tgctgttgacagtgagcgccgatgctgccatttctaataatagtgaagccacagatgtattatta MMP3 gaaatggcagcatcgatgcctactgcctcgga tgctgttgacagtgagcgcgcaaggttatcccaaggatattagtgaagccacagatgtaatatcc MMP8 ttgggataaccttgcatgcctactgcctcgga tgctgttgacagtgagcgccgacatagacggcatccagtatagtgaagccacagatgtatactgg MMP9 atgccgtctatgtcgttgcctactgcctcgga tgctgttgacagtgagcgacgagcctgaatttcatttgattagtgaagccacagatgtaatcaaa MMP10 tgaaattcaggctcggtgcctactgcctcgga tgctgttgacagtgagcgagcaatatttcagctaccaatatagtgaagccacagatgtatattgg MMP11 tagctgaaatattgcctgcctactgcctcgga tgctgttgacagtgagcgccgcgggaatcctgaaggagaatagtgaagccacagatgtattctcc MMP13 ttcaggattcccgcgatgcctactgcctcgga tgctgttgacagtgagcgcggctgacatcatgatcttatttagtgaagccacagatgtaaataag MMP14 atcatgatgtcagccttgcctactgcctcgga tgctgttgacagtgagcgcggccacaccttcttcttccaatagtgaagccacagatgtattggaa MMP15 gaagaaggtgtggccttgcctactgcctcgga tgctgttgacagtgagcgaggcaaacgtgatgtggatatatagtgaagccacagatgtatatatc MMP16 cacatcacgtttgccgtgcctactgcctcgga tgctgttgacagtgagcgcaggaaggatattacacctatttagtgaagccacagatgtaaatagg MMP24 tgtaatatccttcctttgcctactgcctcgga tgctgttgacagtgagcgaccgactcctgctatacctttatagtgaagccacagatgtataaagg ADAM8 tatagcaggagtcggctgcctactgcctcgg tgctgttgacagtgagcgcgccatttcactctgtcatttatagtgaagccacagatgtataaatg ADAM10 acagagtgaaatggcatgcctactgcctcgga tgctgttgacagtgagcgccgacatcctctccttagctaatagtgaagccacagatgtattagct ADAM17 aaggagaggatgtcgttgcctactgcctcgga MOCK tgctgttgacagtgagcgcggcttcagactcattattatatagtgaagccacagatgtatataat -

A Human Breast Cell Model of Preinvasive to Invasive Transition
Research Article A Human Breast Cell Model of Preinvasive to Invasive Transition Aylin Rizki,1 Valerie M. Weaver,2 Sun-Young Lee,1 Gabriela I. Rozenberg,2 Koei Chin,3 Connie A. Myers,1 Jamie L. Bascom,1 Joni D. Mott,1 Jeremy R. Semeiks,1 Leslie R. Grate,1 I. Saira Mian,1 Alexander D. Borowsky,4 Roy A. Jensen,5 Michael O. Idowu,6 Fanqing Chen,1 David J. Chen,1,7 Ole W. Petersen,8 Joe W. Gray,1,4 and Mina J. Bissell1 1Life Sciences Division, Ernest Orlando Lawrence Berkeley National Laboratory, Berkeley, California; 2Department of Pathology and Institute for Medicine and Engineering, University of Pennsylvania, Philadelphia, Pennsylvania; 3Department of Laboratory Medicine and Comprehensive Cancer Center, University of California, San Francisco, San Francisco, California; 4Department of Pathology and Laboratory Medicine and Center for Comparative Medicine, University of California, Davis, Davis, California; 5Kansas Masonic Cancer Research Institute, Kansas City, Kansas; 6Department of Pathology, Virginia Commonwealth University, Richmond, Virginia; 7Department of Radiation Oncology, UT Southwestern Medical Center at Dallas, Dallas, Texas; and 8Department of Cellular and Molecular Medicine, Faculty of Health Sciences, University of Copenhagen, Copenhagen, Denmark Abstract Introduction A crucial step in human breast cancer progression is the Breast carcinomas are phenotypically and behaviorally hetero- acquisition of invasiveness. There is a distinct lack of human geneous (1). Subtypes of breast cancer with distinct behavioral cell culture -

Original Article ITGA8 Accelerates Migration and Invasion of Myeloma Cells in Multiple Myelomas
Int J Clin Exp Med 2021;14(2):1126-1132 www.ijcem.com /ISSN:1940-5901/IJCEM0122176 Original Article ITGA8 accelerates migration and invasion of myeloma cells in multiple myelomas Mengmeng Cui1, Jiangfang Feng1, Xuezhong Gu2, Zhuowei Zhang3, Junxia Zhao1, Hongmei Chai1, Jing Li4, Zheng Xu5 1Department of Hematology, Jincheng General Hospital, Jincheng, Shanxi Province, China; 2Department of He- matology, The First People’s Hospital of Yunnan Province, Kunming, Yunnan Province, China; 3Personnel Depart- ment of Shanxi Medical University, Taiyuan, Shanxi Province, China; 4Department of Oncology, Jincheng General Hospital, Jincheng, Shanxi Province, China; 5Department of Orthopaedics, Jincheng General Hospital, Jincheng, Shanxi Province, China Received September 11, 2020; Accepted October 14, 2020; Epub February 15, 2021; Published February 28, 2021 Abstract: Multiple myeloma is cancer of the plasma cells and is the second most common cancer of the blood system, which is characterized by increased calcium levels, renal insufficiency, anemia, bone disease, and suscep- tibility to infection due to suppression of immunoglobulin production. Early diagnosis of multiple myeloma is difficult as it has no symptoms until it reaches an advanced stage. Therefore, key genes involved in the pathogenesis of multiple myeloma might be significant markers for early diagnosis and treatment of the disease. We analyzed the differentially expressed genes in patients with multiple myeloma using sequencing microarrays from the GEO da- tabase. Combined with GO and KEGG analysis, we identified ITGA8 as a key target in the pathogenesis of multiple myeloma, and further verified the differential expression of ITGA8 in myeloma cell lines by rtPCR experiments. Our study contributes to a better understanding of the development of multiple myeloma and advances the application of bioinformatics in clinical diagnosis. -

Matrix Metalloproteinase-12 Expression Correlates with Local Recurrence and Metastatic Disease in Non–Small Cell Lung Cancer Patients
1086 Vol. 11, 1086–1092, February 1, 2005 Clinical Cancer Research Matrix Metalloproteinase-12 Expression Correlates with Local Recurrence and Metastatic Disease in Non–Small Cell Lung Cancer Patients Hans-Stefan Hofmann,1 Gesine Hansen,2 the 169,000 new cases identified in the United States in 2002 Gu¨nther Richter,4 Christiane Taege,3 will lead to more deaths than breast, colon, prostate, and cervical Andreas Simm,1 Rolf-Edgar Silber,1 cancers combined (1). The pathogenesis of lung cancer remains highly elusive due to its aggressive nature and considerably and Stefan Burdach4 heterogeneity as compared with other cancers. Many lung cancer 1 2 3 Departments of Cardio-Thoracic Surgery and Paediatrics; Institute patients have distant metastases or occult hematogenous and of Pathology, Martin-Luther-University Halle-Wittenberg, Halle; and 4Cancer Center and Division of Pediatric Hematology/Oncology, lymphatic spread of tumor cells at diagnosis, thus accounting for Munich University of Technology, Munich, Germany poor prognosis of this disease (2). Metastasis is the final stage in tumor progression from a normal cell to a fully malignant cell. One of the initial steps in ABSTRACT the metastatic process involves degradation of different Purpose: Non–small cell lung cancer (NSCLC) is a very components of the extracellular matrix and requires the action common and aggressive malignancy. Survival after resection of proteolytic enzymes such as serine-, cysteinyl- and aspartyl- of tumor is especially determined by the occurrence of distant proteinases as well as matrix metalloproteinases (MMP). metastasis. Matrix metalloproteinases (MMP) support this MMPs are a family of more than 20 secreted or transmembrane metastatic process by degradation of the extracellular matrix.