Bacillary Angiomatosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
If Needed You Can Use Two Lines
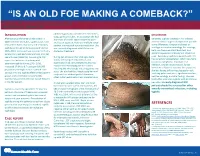
“IS AN OLD FOE MAKING A COMEBACK?” •Eyob Tadesse MD1; Samie Meskele MD1; Ankoor Biswas MD1 •Aurora Health Care, Milwaukee WI. NTRODUCTION abdomen gradually spread to her extremities, DISCUSSION I scalp, palms and soles. In association she had After being on the verge of elimination in shortness of breath, vague abdominal pain Generally, syphilis presents in HIV infected 2000 in the United States, syphilis cases have and loss of appetite, history of multiple sexual patients similar to general population yet with rebounded. Rates of primary and secondary partner, unprotected sex and prostitution. She some differences. Diagnosis is based on syphilis continued to increase overall during was recently diagnosed with HIV but not serologic test and microbiology. For serology, 2005–2013. Increases have occurred primarily started on treatment. both non treponemal antibody test, and among men, and particularly among men has specific treponemal antibody test should be used. Secondary syphilis in patients with HIV sex with men (MSM)(1). According to CDC During her admission her vital signs were has varied skin presentation, which can mimic report the incidence of primary and stable, she had pale conjunctivae, skin cutaneous lymphoma, mycobacterial secondary syphilis during 2015–2016, examination had demonstrated widespread macular and maculopapular skin lesions infection, bacillary angiomatosis, fungal increased 17.6% to 8.7 cases per 100,000 infections or Kaposi’s sarcoma. In our patient, population, the highest rate reported since involving the whole body including palms and soles. She also had thin, fragile scalp hair and she was having diffuse maculopapular rash, 1993(2). HIV and syphilis affect similar patient scalp hair loss without genital ulceration; involving palms and soles, significant hair loss, groups and co-infection is common(3). -

HIV and the SKIN • Sudden Acute Exacerbations • Treatment Failure DR
2018/08/13 KEY FEATURES • Atypical presentation of common disorders • Severe or exaggerated presentations HIV AND THE SKIN • Sudden acute exacerbations • Treatment failure DR. FREDAH MALEKA DERMATOLOGY UNIVERSITY OF PRETORIA:KALAFONG VIRAL INFECTIONS EXANTHEM OF PRIMARY HIV INFECTION • Exanthem of primary HIV infection • Acute retroviral syndrome • Herpes simplex virus (HSV) • Morbilliform rash (exanthem) : 2-4 weeks after HIV exposure • Varicella Zoster virus (VZV) • Typically generalised • Molluscum contagiosum (Poxvirus) • Pronounced on face and trunk, sparing distal extremities • Human papillomavirus (HPV) • Associated : fever, lymphadenopathy, pharyngitis • Epstein Barr virus (EBV) • DDX: drug reaction • Cytomegalovirus (CMV) • other viral infections – EBV, Enteroviruses, Hepatitis B virus 1 2018/08/13 HERPES SIMPLEX VIRUS(HSV) • Vesicular eruption due to HSV 1&2 • Primary lesion: painful, grouped vesicles on an erythematous base • HIV: attacks are more frequent and severe • : chronic, non-healing, deep ulcers, with scarring and tissue destruction • CLUE: severe pain and recurrences • DDX: syphilis, chancroid, lymphogranuloma venereum • Tzanck smear, Histology, Viral culture HSV • Treatment: Acyclovir 400mg tds 7-10 days • Alternatives: Valacyclovir and Famciclovir • In setting of treatment failure, viral isolates tested for resistance against acyclovir • Alternative drugs: Foscarnet, Cidofovir • Chronic suppressive therapy ( >8 attacks per year) 2 2018/08/13 VARICELLA • Chickenpox • Presents with erythematous papules and umbilicated -

Coexistence of Antibodies to Tick-Borne
Mem Inst Oswaldo Cruz, Rio de Janeiro, Vol. 98(3): 311-318, April 2003 311 Coexistence of Antibodies to Tick-borne Agents of Babesiosis and Lyme Borreliosis in Patients from Cotia County, State of São Paulo, Brazil Natalino Hajime Yoshinari/+, Milena Garcia Abrão, Virginia Lúcia Nazário Bonoldi, Cleber Oliveira Soares*, Claudio Roberto Madruga*, Alessandra Scofield**, Carlos Luis Massard**, Adivaldo Henrique da Fonseca** Laboratório de Investigação em Reumatologia (LIM-17), Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, Av. Dr. Arnaldo 455, 3º andar, 01246-903 São Paulo, SP, Brasil *Embrapa Gado de Corte, Campo Grande, MS, Brasil **Universidade Federal Rural do Rio de Janeiro, Seropédica, RJ, Brasil This paper reports a case of coinfection caused by pathogens of Lyme disease and babesiosis in brothers. This was the first case of borreliosis in Brazil, acquired in Cotia County, State of São Paulo, Brazil. Both children had tick bite history, presented erythema migrans, fever, arthralgia, mialgia, and developed positive serology (ELISA and Western-blotting) directed to Borrelia burgdorferi G 39/40 and Babesia bovis antigens, mainly of IgM class antibodies, suggestive of acute disease. Also, high frequencies of antibodies to B. bovis was observed in a group of 59 Brazilian patients with Lyme borreliosis (25.4%), when compared with that obtained in a normal control group (10.2%) (chi-square = 5.6; p < 0.05). Interestingly, both children presented the highest titers for IgM antibodies directed to both infective diseases, among all patients with Lyme borreliosis. Key words: lyme borreliosis - lyme disease - spirochetosis - borreliosis - babesiosis - coinfection - tick-borne disease - Brazil Babesiosis is a tick-borne disease distributed world- The first case of babesiosis in a healthy person, with wide, caused by hemoprotozoans of the genus Babesia, intact spleen, was reported in 1969 in a woman from Nan- which infects wild and domestic animals, promoting eco- tucket Island (Massachusetts, USA)(Wester et al. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Bacterial Infections Diseases Picture Cause Basic Lesion
page: 117 Chapter 6: alphabetical Bacterial infections diseases picture cause basic lesion search contents print last screen viewed back next Bacterial infections diseases Impetigo page: 118 6.1 Impetigo alphabetical Bullous impetigo Bullae with cloudy contents, often surrounded by an erythematous halo. These bullae rupture easily picture and are rapidly replaced by extensive crusty patches. Bullous impetigo is classically caused by Staphylococcus aureus. cause basic lesion Basic Lesions: Bullae; Crusts Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Impetigo page: 119 alphabetical Non-bullous impetigo Erythematous patches covered by a yellowish crust. Lesions are most frequently around the mouth. picture Lesions around the nose are very characteristic and require prolonged treatment. ß-Haemolytic streptococcus is cause most frequently found in this type of impetigo. basic lesion Basic Lesions: Erythematous Macule; Crusts Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Ecthyma page: 120 6.2 Ecthyma alphabetical Slow and gradually deepening ulceration surmounted by a thick crust. The usual site of ecthyma are the legs. After healing there is a permanent scar. The pathogen is picture often a streptococcus. Ecthyma is very common in tropical countries. cause basic lesion Basic Lesions: Crusts; Ulcers Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Folliculitis page: 121 6.3 Folliculitis -

Rheumatic Manifestations of Bartonella Infection in 2 Children MOHAMMAD J
Case Report Rheumatic Manifestations of Bartonella Infection in 2 Children MOHAMMAD J. AL-MATAR, ROSS E. PETTY, DAVID A. CABRAL, LORI B. TUCKER, BANAFSHI PEYVANDI, JULIE PRENDIVILLE, JACK FORBES, ROBYN CAIRNS, and RALPH ROTHSTEIN ABSTRACT. We describe 2 patients with very unusual rheumatological presentations presumably caused by Bartonella infection: one had myositis of proximal thigh muscles bilaterally, and the other had arthritis and skin nodules. Both patients had very high levels of antibody to Bartonella that decreased in asso- ciation with clinical improvement. Bartonella infection should be considered in the differential diag- nosis of unusual myositis or arthritis in children. (J Rheumatol 2002;29:184–6) Key Indexing Terms: MYOSITIS ARTHRITIS BARTONELLA Infection with Bartonella species has a wide range of mani- was slightly increased at 9.86 IU/l (normal 4.51–9.16), and IgA was 2.1 IU/l festations in children including cat scratch disease (regional (normal 0.2–1.0). C3 was 0.11 g/l (normal 0.77–1.43) and C4 was 0.28 (nor- mal 0.07–0.40). Antinuclear antibodies were present at a titer of 1:40, the anti- granulomatous lymphadenitis), bacillary angiomatosis, streptolysin O titer was 35 (normal < 200), and the anti-DNAase B titer was encephalitis, Parinaud’s oculoglandular syndrome, Trench 1:85 (normal). Urinalysis showed 50–100 erythrocytes and 5–10 leukocytes fever (Vincent’s angina), osteomyelitis, granulomatous per high power field. Routine cultures of urine, blood, and throat were nega- hepatitis, splenitis, pneumonitis, endocarditis, and fever of tive. Liver enzymes, electrolytes, HIV serology, cerebrospinal fluid analysis, unknown origin1-3. -

An Important One Health Opportunity
veterinary sciences Review Ehrlichioses: An Important One Health Opportunity Tais B. Saito * and David H. Walker Department of Pathology, University of Texas Medical Branch at Galveston, Galveston, TX 77555, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-1409-772-4813 Academic Editor: Ulrike Munderloh Received: 15 July 2016; Accepted: 25 August 2016; Published: 31 August 2016 Abstract: Ehrlichioses are caused by obligately intracellular bacteria that are maintained subclinically in a persistently infected vertebrate host and a tick vector. The most severe life-threatening illnesses, such as human monocytotropic ehrlichiosis and heartwater, occur in incidental hosts. Ehrlichia have a developmental cycle involving an infectious, nonreplicating, dense core cell and a noninfectious, replicating reticulate cell. Ehrlichiae secrete proteins that bind to host cytoplasmic proteins and nuclear chromatin, manipulating the host cell environment to their advantage. Severe disease in immunocompetent hosts is mediated in large part by immunologic and inflammatory mechanisms, including overproduction of tumor necrosis factor α (TNF-α), which is produced by CD8 T lymphocytes, and interleukin-10 (IL-10). Immune components that contribute to control of ehrlichial infection include CD4 and CD8 T cells, natural killer (NK) cells, interferon-γ (IFN-γ), IL-12, and antibodies. Some immune components, such as TNF-α, perforin, and CD8 T cells, play both pathogenic and protective roles. In contrast with the immunocompetent host, which may die with few detectable organisms owing to the overly strong immune response, immunodeficient hosts die with overwhelming infection and large quantities of organisms in the tissues. Vaccine development is challenging because of antigenic diversity of E. -

Skin Disease and Disorders
Sports Dermatology Robert Kiningham, MD, FACSM Department of Family Medicine University of Michigan Health System Disclosures/Conflicts of Interest ◼ None Goals and Objectives ◼ Review skin infections common in athletes ◼ Establish a logical treatment approach to skin infections ◼ Discuss ways to decrease the risk of athlete’s acquiring and spreading skin infections ◼ Discuss disqualification and return-to-play criteria for athletes with skin infections ◼ Recognize and treat non-infectious skin conditions in athletes Skin Infections in Athletes ◼ Bacterial ◼ Herpetic ◼ Fungal Skin Infections in Athletes ◼ Very common – most common cause of practice-loss time in wrestlers ◼ Athletes are susceptible because: – Prone to skin breakdown (abrasions, cuts) – Warm, moist environment – Close contacts Cases 1 -3 ◼ 21 year old male football player with 4 day h/o left axillary pain and tenderness. Two days ago he noticed a tender “bump” that is getting bigger and more tender. ◼ 16 year old football player with 3 day h/o mildly tender lesions on chin. Started as a single lesion, but now has “spread”. Over the past day the lesions have developed a dark yellowish crust. ◼ 19 year old wrestler with a 3 day h/o lesions on right side of face. Noticed “tingling” 4 days ago, small fluid filled lesions then appeared that have now started to crust over. Skin Infections Bacterial Skin Infections ◼ Cellulitis ◼ Erysipelas ◼ Impetigo ◼ Furunculosis ◼ Folliculitis ◼ Paronychea Cellulitis Cellulitis ◼ Diffuse infection of connective tissue with severe inflammation of dermal and subcutaneous layers of the skin – Triad of erythema, edema, and warmth in the absence of underlying foci ◼ S. aureus or S. pyogenes Erysipelas Erysipelas ◼ Superficial infection of the dermis ◼ Distinguished from cellulitis by the intracutaneous edema that produces palpable margins of the skin. -

Pediatric Cutaneous Bacterial Infections Dr
PEDIATRIC CUTANEOUS BACTERIAL INFECTIONS DR. PEARL C. KWONG MD PHD BOARD CERTIFIED PEDIATRIC DERMATOLOGIST JACKSONVILLE, FLORIDA DISCLOSURE • No relevant relationships PRETEST QUESTIONS • In Staph scalded skin syndrome: • A. The staph bacteria can be isolated from the nares , conjunctiva or the perianal area • B. The patients always have associated multiple system involvement including GI hepatic MSK renal and CNS • C. common in adults and adolescents • D. can also be caused by Pseudomonas aeruginosa • E. None of the above PRETEST QUESTIONS • Scarlet fever • A. should be treated with penicillins • B. should be treated with sulfa drugs • C. can lead to toxic shock syndrome • D. can be associated with pharyngitis or circumoral pallor • E. Both A and D are correct PRETEST QUESTIONS • Strep can be treated with the following antibiotics • A. Penicillin • B. First generation cephalosporin • C. clindamycin • D. Septra • E. A B or C • F. A and D only PRETEST QUESTIONS • MRSA • A. is only acquired via hospital • B. can be acquired in the community • C. is more aggressive than OSSA • D. needs treatment with first generation cephalosporin • E. A and C • F. B and C CUTANEOUS BACTERIAL PATHOGENS • Staphylococcus aureus: OSSA and MRSA • Gp A Streptococcus GABHS • Pseudomonas aeruginosa CUTANEOUS BACTERIAL INFECTIONS • Folliculitis • Non bullous Impetigo/Bullous Impetigo • Furuncle/Carbuncle/Abscess • Cellulitis • Acute Paronychia • Dactylitis • Erysipelas • Impetiginization of dermatoses BACTERIAL INFECTION • Important to diagnose early • Almost always -

Building Blocks of Clinical Practice Helping Athletic Trainers Build a Strong Foundation
Building Blocks of Clinical Practice Helping Athletic Trainers Build a Strong Foundation Issue #2: Bacterial Infections of the Skin Folliculitis Carbuncles Definition: Definition: • Inflammation of a hair follicle • A complication of folliculitis, a carbuncle is several • Can progress down hair follicle or into multiple furuncles that have merged.merged follicles and result in a furuncle or carbuncle • Carbuncles are readily transmitted by skin-to-skin contact. Often, the direct cause of a carbuncle cannot Causes: be determined.determined • Bacterial or viral infection, chemical irritation • Secondary to skin injury, which introduces bacteria to Causes: the area • Most carbuncles are caused by the bacteria • Shaving hairy areas may facilitate infection staphylococcus aureus. The infection is contagious and • Occlusion of hair-bearing areas may facilitate growth may spread to other areas of the body or other people.people of microbes • Friction Symptoms: • Hyperhidrosis • A carbuncle is a swollen lump or mass under the skin which may be the size of a pea or as larlargege as a golf ball.ball Symptoms: • The carbuncle may be red and irritated and might hurt • Areas are usually non-tender or slightly tender when you touch it.it • Area may itch • Pain gets worse as it fills with pus and dead tissue.tissue • Erythematous perifollicular papules or pustules may • Other signs and symptoms include itching at the site of develop infection, skin inflammation around the wound, general • Grouped lesions ill feeling, fever, or fatigue. Pain improves -

Circulatory and Lymphatic System Infections 1105
Chapter 25 | Circulatory and Lymphatic System Infections 1105 Chapter 25 Circulatory and Lymphatic System Infections Figure 25.1 Yellow fever is a viral hemorrhagic disease that can cause liver damage, resulting in jaundice (left) as well as serious and sometimes fatal complications. The virus that causes yellow fever is transmitted through the bite of a biological vector, the Aedes aegypti mosquito (right). (credit left: modification of work by Centers for Disease Control and Prevention; credit right: modification of work by James Gathany, Centers for Disease Control and Prevention) Chapter Outline 25.1 Anatomy of the Circulatory and Lymphatic Systems 25.2 Bacterial Infections of the Circulatory and Lymphatic Systems 25.3 Viral Infections of the Circulatory and Lymphatic Systems 25.4 Parasitic Infections of the Circulatory and Lymphatic Systems Introduction Yellow fever was once common in the southeastern US, with annual outbreaks of more than 25,000 infections in New Orleans in the mid-1800s.[1] In the early 20th century, efforts to eradicate the virus that causes yellow fever were successful thanks to vaccination programs and effective control (mainly through the insecticide dichlorodiphenyltrichloroethane [DDT]) of Aedes aegypti, the mosquito that serves as a vector. Today, the virus has been largely eradicated in North America. Elsewhere, efforts to contain yellow fever have been less successful. Despite mass vaccination campaigns in some regions, the risk for yellow fever epidemics is rising in dense urban cities in Africa and South America.[2] In an increasingly globalized society, yellow fever could easily make a comeback in North America, where A. aegypti is still present. -

Modern Surgery, 4Th Edition, by John Chalmers Da Costa Rare Medical Books
Thomas Jefferson University Jefferson Digital Commons Modern Surgery, 4th edition, by John Chalmers Da Costa Rare Medical Books 1903 Modern Surgery - Chapter 31. Diseases of the Skin and Nails John Chalmers Da Costa Jefferson Medical College Follow this and additional works at: https://jdc.jefferson.edu/dacosta_modernsurgery Part of the History of Science, Technology, and Medicine Commons Let us know how access to this document benefits ouy Recommended Citation Da Costa, John Chalmers, "Modern Surgery - Chapter 31. Diseases of the Skin and Nails" (1903). Modern Surgery, 4th edition, by John Chalmers Da Costa. Paper 14. https://jdc.jefferson.edu/dacosta_modernsurgery/14 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Modern Surgery, 4th edition, by John Chalmers Da Costa by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. 896 Diseases of the Skin and Nails XXXI. DISEASES OF THE SKIN AND NAILS. Dermatitis venenata results from irritants and from garments con- taining arsenic, but is generally due to rhus-poisoning. Rhus-poisoning arises from the poison-oak, the poison-ash, the poison-ivy, and other species of sumach.