Rheumatic Manifestations of Bartonella Infection in 2 Children MOHAMMAD J
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melioidosis: an Emerging Infectious Disease
Review Article www.jpgmonline.com Melioidosis: An emerging infectious disease Raja NS, Ahmed MZ,* Singh NN** Department of Medical ABSTRACT Microbiology, University of Malaya Medical Center, Kuala Lumpur, Infectious diseases account for a third of all the deaths in the developing world. Achievements in understanding Malaysia, *St. the basic microbiology, pathogenesis, host defenses and expanded epidemiology of infectious diseases have Bartholomew’s Hospital, resulted in better management and reduced mortality. However, an emerging infectious disease, melioidosis, West Smithfield, London, is becoming endemic in the tropical regions of the world and is spreading to non-endemic areas. This article UK and **School of highlights the current understanding of melioidosis including advances in diagnosis, treatment and prevention. Biosciences, Cardiff Better understanding of melioidosis is essential, as it is life-threatening and if untreated, patients can succumb University, Cardiff, UK to it. Our sources include a literature review, information from international consensus meetings on melioidosis Correspondence: and ongoing discussions within the medical and scientific community. N. S. Raja, E-mail: [email protected] Received : 21-2-2005 Review completed : 20-3-2005 Accepted : 30-5-2005 PubMed ID : 16006713 KEY WORDS: Melioidosis, Burkholderia pseudomallei, Infection J Postgrad Med 2005;51:140-5 he name melioidosis [also known as Whitmore dis- in returning travellers to Europe from endemic areas.[14] The T ease] is taken from the Greek word ‘melis’ meaning geographic area of the prevalence of the organism is bound to distemper of asses and ‘eidos’ meaning resembles glanders. increase as the awareness increases. Melioidosis is a zoonotic disease caused by Pseudomonas pseudomallei [now known as Burkholderia pseudomallei], a B. -
If Needed You Can Use Two Lines
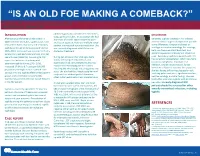
“IS AN OLD FOE MAKING A COMEBACK?” •Eyob Tadesse MD1; Samie Meskele MD1; Ankoor Biswas MD1 •Aurora Health Care, Milwaukee WI. NTRODUCTION abdomen gradually spread to her extremities, DISCUSSION I scalp, palms and soles. In association she had After being on the verge of elimination in shortness of breath, vague abdominal pain Generally, syphilis presents in HIV infected 2000 in the United States, syphilis cases have and loss of appetite, history of multiple sexual patients similar to general population yet with rebounded. Rates of primary and secondary partner, unprotected sex and prostitution. She some differences. Diagnosis is based on syphilis continued to increase overall during was recently diagnosed with HIV but not serologic test and microbiology. For serology, 2005–2013. Increases have occurred primarily started on treatment. both non treponemal antibody test, and among men, and particularly among men has specific treponemal antibody test should be used. Secondary syphilis in patients with HIV sex with men (MSM)(1). According to CDC During her admission her vital signs were has varied skin presentation, which can mimic report the incidence of primary and stable, she had pale conjunctivae, skin cutaneous lymphoma, mycobacterial secondary syphilis during 2015–2016, examination had demonstrated widespread macular and maculopapular skin lesions infection, bacillary angiomatosis, fungal increased 17.6% to 8.7 cases per 100,000 infections or Kaposi’s sarcoma. In our patient, population, the highest rate reported since involving the whole body including palms and soles. She also had thin, fragile scalp hair and she was having diffuse maculopapular rash, 1993(2). HIV and syphilis affect similar patient scalp hair loss without genital ulceration; involving palms and soles, significant hair loss, groups and co-infection is common(3). -

Cutaneous Manifestations of HIV Infection Carrie L
Chapter Title Cutaneous Manifestations of HIV Infection Carrie L. Kovarik, MD Addy Kekitiinwa, MB, ChB Heidi Schwarzwald, MD, MPH Objectives Table 1. Cutaneous manifestations of HIV 1. Review the most common cutaneous Cause Manifestations manifestations of human immunodeficiency Neoplasia Kaposi sarcoma virus (HIV) infection. Lymphoma 2. Describe the methods of diagnosis and treatment Squamous cell carcinoma for each cutaneous disease. Infectious Herpes zoster Herpes simplex virus infections Superficial fungal infections Key Points Angular cheilitis 1. Cutaneous lesions are often the first Chancroid manifestation of HIV noted by patients and Cryptococcus Histoplasmosis health professionals. Human papillomavirus (verruca vulgaris, 2. Cutaneous lesions occur frequently in both adults verruca plana, condyloma) and children infected with HIV. Impetigo 3. Diagnosis of several mucocutaneous diseases Lymphogranuloma venereum in the setting of HIV will allow appropriate Molluscum contagiosum treatment and prevention of complications. Syphilis Furunculosis 4. Prompt diagnosis and treatment of cutaneous Folliculitis manifestations can prevent complications and Pyomyositis improve quality of life for HIV-infected persons. Other Pruritic papular eruption Seborrheic dermatitis Overview Drug eruption Vasculitis Many people with human immunodeficiency virus Psoriasis (HIV) infection develop cutaneous lesions. The risk of Hyperpigmentation developing cutaneous manifestations increases with Photodermatitis disease progression. As immunosuppression increases, Atopic Dermatitis patients may develop multiple skin diseases at once, Hair changes atypical-appearing skin lesions, or diseases that are refractory to standard treatment. Skin conditions that have been associated with HIV infection are listed in Clinical staging is useful in the initial assessment of a Table 1. patient, at the time the patient enters into long-term HIV care, and for monitoring a patient’s disease progression. -

HIV and the SKIN • Sudden Acute Exacerbations • Treatment Failure DR
2018/08/13 KEY FEATURES • Atypical presentation of common disorders • Severe or exaggerated presentations HIV AND THE SKIN • Sudden acute exacerbations • Treatment failure DR. FREDAH MALEKA DERMATOLOGY UNIVERSITY OF PRETORIA:KALAFONG VIRAL INFECTIONS EXANTHEM OF PRIMARY HIV INFECTION • Exanthem of primary HIV infection • Acute retroviral syndrome • Herpes simplex virus (HSV) • Morbilliform rash (exanthem) : 2-4 weeks after HIV exposure • Varicella Zoster virus (VZV) • Typically generalised • Molluscum contagiosum (Poxvirus) • Pronounced on face and trunk, sparing distal extremities • Human papillomavirus (HPV) • Associated : fever, lymphadenopathy, pharyngitis • Epstein Barr virus (EBV) • DDX: drug reaction • Cytomegalovirus (CMV) • other viral infections – EBV, Enteroviruses, Hepatitis B virus 1 2018/08/13 HERPES SIMPLEX VIRUS(HSV) • Vesicular eruption due to HSV 1&2 • Primary lesion: painful, grouped vesicles on an erythematous base • HIV: attacks are more frequent and severe • : chronic, non-healing, deep ulcers, with scarring and tissue destruction • CLUE: severe pain and recurrences • DDX: syphilis, chancroid, lymphogranuloma venereum • Tzanck smear, Histology, Viral culture HSV • Treatment: Acyclovir 400mg tds 7-10 days • Alternatives: Valacyclovir and Famciclovir • In setting of treatment failure, viral isolates tested for resistance against acyclovir • Alternative drugs: Foscarnet, Cidofovir • Chronic suppressive therapy ( >8 attacks per year) 2 2018/08/13 VARICELLA • Chickenpox • Presents with erythematous papules and umbilicated -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

An Important One Health Opportunity
veterinary sciences Review Ehrlichioses: An Important One Health Opportunity Tais B. Saito * and David H. Walker Department of Pathology, University of Texas Medical Branch at Galveston, Galveston, TX 77555, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-1409-772-4813 Academic Editor: Ulrike Munderloh Received: 15 July 2016; Accepted: 25 August 2016; Published: 31 August 2016 Abstract: Ehrlichioses are caused by obligately intracellular bacteria that are maintained subclinically in a persistently infected vertebrate host and a tick vector. The most severe life-threatening illnesses, such as human monocytotropic ehrlichiosis and heartwater, occur in incidental hosts. Ehrlichia have a developmental cycle involving an infectious, nonreplicating, dense core cell and a noninfectious, replicating reticulate cell. Ehrlichiae secrete proteins that bind to host cytoplasmic proteins and nuclear chromatin, manipulating the host cell environment to their advantage. Severe disease in immunocompetent hosts is mediated in large part by immunologic and inflammatory mechanisms, including overproduction of tumor necrosis factor α (TNF-α), which is produced by CD8 T lymphocytes, and interleukin-10 (IL-10). Immune components that contribute to control of ehrlichial infection include CD4 and CD8 T cells, natural killer (NK) cells, interferon-γ (IFN-γ), IL-12, and antibodies. Some immune components, such as TNF-α, perforin, and CD8 T cells, play both pathogenic and protective roles. In contrast with the immunocompetent host, which may die with few detectable organisms owing to the overly strong immune response, immunodeficient hosts die with overwhelming infection and large quantities of organisms in the tissues. Vaccine development is challenging because of antigenic diversity of E. -

Gonococcal Prosthetic Joint Infection Ian Gassiep1, 2, Bradley Gilpin2, 3, Joel Douglas1, David Siebert1, 2
J. Bone Joint Infect. 2017, Vol. 2 160 Ivyspring International Publisher Journal of Bone and Joint Infection 2017; 2(3): 160-162. doi: 10.7150/jbji.20791 Short Research Communication Gonococcal Prosthetic Joint Infection Ian Gassiep1, 2, Bradley Gilpin2, 3, Joel Douglas1, David Siebert1, 2 1. Department of Infectious Diseases, Princess Alexandra Hospital, Queensland Health, Woolloongabba, Queensland, Australia; 2. School of Medicine, University of Queensland, Brisbane, Queensland, Australia; 3. Department of Orthopaedic Surgery, Princess Alexandra Hospital, Queensland Health, Woolloongabba, Queensland, Australia. Corresponding author: Ian Gassiep, Department of Infectious Diseases, Princess Alexandra Hospital, 199 Ipswich Rd, Woolloongabba, QLD 4102, Australia Tel: +61430662244 Facsimile: +6173176 5920 Email: [email protected] © Ivyspring International Publisher. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY-NC) license (https://creativecommons.org/licenses/by-nc/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2017.04.28; Accepted: 2017.07.27; Published: 2017.08.18 Abstract Neisseria gonorrhoea is a common sexually transmitted infection worldwide. Disseminated gonococcal infection is an infrequent presentation and rarely can be associated with septic arthritis. Incidence of this infection is rising, both internationally and in older age groups. We present the first documented case of N. gonorrhoea prosthetic joint infection which was successfully treated with laparoscopic debridement and antimicrobial therapy. Key words: Gonorrhoea; prosthetic joint infection; gonococcal arthritis; DGI. Introduction Neisseria gonorrhoea is an aerobic facultative poorly diet controlled type 2 diabetes mellitus, intracellular gram negative bacteria typically HbA1C: 8.3% (4.3-6.0). appearing as diplococci [1]. -

Urinogenital Infections in the Tropics
8.1 CHAPTER 8 Urinogenital infections in the tropics Ahmed S. Latif The range of urinary tract infections and sexually transmitted infections varies from place to place and though the aetiology and clinical presentation of infections is similar in industrialised and developing countries it is evident that persons with these infections resource-constrained tropical areas of the world often present for care with more severe illness and often only after complications have developed. For clinicians working in resource-constrained settings it is important to be aware of symptoms and signs of UTI and STIs so that early effective care may be provided before complications develop. Clinicians should also be aware that laboratory services are not widely available in rural and remote countries throughout the world and hence persons suspected of having infection should be treated according to clinical symptoms and signs as results of tests may not become available till much later. In managing persons with STIs the syndromic approach is particularly useful as reliance is not placed on the results of laboratory tests. *** PART A URINARY TRACT INFECTIONS 8.1 Introduction The term urinary tract infection covers a number of infections affecting the urinary tract, including asymptomatic bacteriuria, pyelonephritis, cystitis, prostatitis and urethritis. In this section the non-sexually transmitted infections of the urinary tract are described. The commonest causes of community acquired infection world-wide are Escherichia coli and Staphylococcus saprophyticus; other pathogens including Klebsiella, Proteus and Enterobacter species cause infections more frequently in hospitalised patients, and in patients who have had urinary tract instrumentation and in those that have urinary catheters. -

Circulatory and Lymphatic System Infections 1105
Chapter 25 | Circulatory and Lymphatic System Infections 1105 Chapter 25 Circulatory and Lymphatic System Infections Figure 25.1 Yellow fever is a viral hemorrhagic disease that can cause liver damage, resulting in jaundice (left) as well as serious and sometimes fatal complications. The virus that causes yellow fever is transmitted through the bite of a biological vector, the Aedes aegypti mosquito (right). (credit left: modification of work by Centers for Disease Control and Prevention; credit right: modification of work by James Gathany, Centers for Disease Control and Prevention) Chapter Outline 25.1 Anatomy of the Circulatory and Lymphatic Systems 25.2 Bacterial Infections of the Circulatory and Lymphatic Systems 25.3 Viral Infections of the Circulatory and Lymphatic Systems 25.4 Parasitic Infections of the Circulatory and Lymphatic Systems Introduction Yellow fever was once common in the southeastern US, with annual outbreaks of more than 25,000 infections in New Orleans in the mid-1800s.[1] In the early 20th century, efforts to eradicate the virus that causes yellow fever were successful thanks to vaccination programs and effective control (mainly through the insecticide dichlorodiphenyltrichloroethane [DDT]) of Aedes aegypti, the mosquito that serves as a vector. Today, the virus has been largely eradicated in North America. Elsewhere, efforts to contain yellow fever have been less successful. Despite mass vaccination campaigns in some regions, the risk for yellow fever epidemics is rising in dense urban cities in Africa and South America.[2] In an increasingly globalized society, yellow fever could easily make a comeback in North America, where A. aegypti is still present. -

Tularemia (CFSPH)
Tularemia Importance Tularemia is a zoonotic bacterial disease with a wide host range. Infections are most prevalent among wild mammals and marsupials, with periodic epizootics in Rabbit Fever, lagomorphs and rodents, but clinical cases also occur in sheep, cats and other Deerfly Fever, domesticated species. A variety of syndromes can be seen, but fatal septicemia is Meat-Cutter’s Disease common in some species. In humans, tularemia varies from a localized infection to Ohara Disease, fulminant, life-threatening pneumonia or septicemia. Francis Disease Tularemia is mainly seen in the Northern Hemisphere, where it has recently emerged or re-emerged in some areas, including parts of Europe and the Middle East. A few endemic clinical cases have also been recognized in regions where this disease Last Updated: June 2017 was not thought to exist, such as Australia, South Korea and southern Sudan. In some cases, emergence may be due to increased awareness, surveillance and/or reporting requirements; in others, it has been associated with population explosions of animal reservoir hosts, or with social upheavals such as wars, where sanitation is difficult and infected rodents may contaminate food and water supplies. Occasionally, this disease may even be imported into a country in animals. In 2002, tularemia entered the Czech Republic in a shipment of sick pet prairie dogs from the U.S. Etiology Tularemia is caused by Francisella tularensis (formerly known as Pasteurella tularensis), a Gram negative coccobacillus in the family Francisellaceae and class γ- Proteobacteria. Depending on the author, either three or four subspecies are currently recognized. F. tularensis subsp. tularensis (also known as type A) and F. -

Gonococcal Subcutaneous Abscess and Pyomyositis: a Case Report
Hindawi Publishing Corporation Case Reports in Infectious Diseases Volume 2012, Article ID 790478, 4 pages doi:10.1155/2012/790478 Case Report Gonococcal Subcutaneous Abscess and Pyomyositis: ACaseReport Anupop Jitmuang,1 Adhiratha Boonyasiri,1 Nukool Keurueangkul,2 Amornrut Leelaporn,3 and Amorn Leelarasamee1 1 Division of Infectious Disease and Tropical Medicine, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand 2 Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand 3 Department of Microbiology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand Correspondence should be addressed to Anupop Jitmuang, [email protected] Received 31 March 2012; Accepted 10 July 2012 Academic Editors: W. Chierakul, L. Falk, A. Marangoni, and G. Walder Copyright © 2012 Anupop Jitmuang et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Disseminated gonococcal infection (DGI) is an uncommon complication of Neisseria gonorrhoeae infection, its manifestation varies from a classic arthritis-dermatitis syndrome to uncommon pyogenic infections of several organs. Herein, we reported atypical presentation of DGI with subcutaneous abscess of right knee, pyomyositis of right lower extremity, and subsequently complicated by Escherichia coli pyomyositis. This infection responded to appropriate antimicrobial therapy and prompt surgical management with good clinical outcome. 1. Introduction of perianal pain during this illness. At Siriraj Hospital, body temperature was 38.2◦C, pulse rate 102/minute, blood Neisseria gonorrhoeae is a fastidious gram-negative diplo- pressure and respiratory rate were normal. -

Extraintestinal Salmonellosis in the Immunocompromised: an Unusual Case of Pyomyositis
Hindawi Case Reports in Medicine Volume 2017, Article ID 5030961, 5 pages https://doi.org/10.1155/2017/5030961 Case Report Extraintestinal Salmonellosis in the Immunocompromised: An Unusual Case of Pyomyositis Veeraraghavan Meyyur Aravamudan,1 Phang Kee Fong,1 Pavel Singh,2 Jong Sze Chin,1 Yang Shiyao Sam,1 and P. A. Tambyah1,3 1 Department of Medicine, National University Hospital, 5 Lower Kent Ridge Road, Singapore 119074 2Department of Diagnostic Imaging, National University Hospital, 5 Lower Kent Ridge Road, Singapore 119074 3Division of Infectious Diseases, National University Hospital, Singapore Correspondence should be addressed to Veeraraghavan Meyyur Aravamudan; veera meyyur [email protected] Received 12 June 2017; Accepted 23 August 2017; Published 11 September 2017 Academic Editor: Ting Fan Leung Copyright © 2017 Veeraraghavan Meyyur Aravamudan et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Salmonella infection can cause a wide range of presentations, predominantly gastrointestinal but occasionally with cardiovascular or other extraintestinal manifestations. The diagnosis of extraintestinal salmonellosis requires a high degree of clinical suspicion and should be considered in patients with deep-seated abscesses especially if they are immunocompromised. We present a case of salmonella causing gastroenteritis complicated by an intramuscular abscess of the left leg. With prompt recognition and multidisciplinary management, the patient recovered with no serious sequela. 1. Introduction Physical examination revealed pyrexia (temperature: 38.9 degrees Celsius), blood pressure of 140/60 mmHg, and pulse Salmonella infection can cause a wide range of presentations rate of 80/min.