Tick‐Borne Encephalitis Virus in Cows and Unpasteurized Cow Milk from Norway
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fylkesmannens Kommunebilde Evje Og Hornnes Kommune 2013
Fylkesmannens kommunebilde Evje og Hornnes kommune 2013 Innhold 1 Innledning 3 2 Planlegging og styring av kommunen 4 2.1 Demografi 4 2.2 Likestilling 5 2.3 Økonomi og økonomistyring 8 2.4 Bosetting og kvalifisering av flyktninger 12 3 Tjenesteyting og velferdsproduksjon 14 3.1 Barnehage 14 3.2 Tidlig innsats 18 3.3 Utdanning 19 3.4 Vergemål 25 3.5 Byggesak 26 3.6 Folkehelse og levekår 27 3.7 Barneverntjenesten 29 3.8 Helsesøster- og jordmortjeneste 32 3.9 Helsetjenester 33 3.10 Tjenester i sykehjem 35 3.11 Velferdsprofil 37 3.12 Arealplanlegging 39 3.13 Forurensning 40 3.14 Landbruk 41 Side: 2 - Fylkesmannen i Aust-Agder, kommunebilde 2013 Evje og Hornnes 1 Innledning Kommunebilde, som Fylkesmannen utarbeider for alle 15 kommuner i Aust-Agder, er et viktig element i styringsdialogen mellom kommunene og Fylkesmannen. Det gir ikke et fullstendig utfyllende bilde av kommunens virksomhet, men gjelder de felt der Fylkesmannen har oppdrag og dialog mot kommunene. Det er et dokument som peker på utfordringer og handlingsrom. Fylkesmannen er opptatt av at kommunene kan løse sine oppgaver best mulig og ha politisk og administrativt handlingsrom. Det er viktig at kommunene har et best mulig beslutningsgrunnlag for de valg de tar. Blant annet derfor er kommunebilde et viktig dokument. Kommunebilde er inndelt i tre 1. Innledning 2. Planlegging og styring av kommunen 3. Tjenesteyting og velferdsproduksjon Under hvert punkt har vi oppsummert Fylkesmannens vurdering av utfordringspunkter for kommunen. Dette er punkter vi anbefaler kommunen å legge til grunn i videre kommunalplanlegging. Kommunebilde er et godt utgangspunkt for å få et makrobilde av kommunen og bør brukes aktivt i kommunen – ikke minst av de folkevalgte. -

Utdanningsplan for Leger I Spesialisering I Nyresykdommer Ved Sørlandet Sykehus
Utdanningsplan for leger i spesialisering i nyresykdommer ved Sørlandet Sykehus Om utdanningsvirksomheten Sørlandet sykehus er Agders største kompetansebedrift, med over 7000 ansatte fordelt på ulike lokasjoner. SSHF har ansvar for spesialisthelsetjenester innen fysisk og psykisk helse og avhengighetsbehandling. Sykehusene ligger i Arendal, Kristiansand og Flekkefjord. I tillegg har vi distriktspsykiatriske sentre og poliklinikker flere andre steder i Agder. I fjor var det over 550 000 pasientbehandlinger i Sørlandet sykehus. Om organisering av spesialiteten Nyremedisinsk virksomhet er organisert som seksjoner i medisinsk avdeling både i Arendal og Kristiansand. Ved begge avdelinger er det egen dialyseavdeling. Det behandles også mange nyrepasienter i Flekkefjord i den generelle indremedisinske avdelingen der som også har egen dialyseavdeling. Ved behov for nyremedisinsk kompetanse konsulteres nyrelegene i Kristiansand eller pasientene overflyttes dit. De nyremedisinske pasientene håndteres poliklinisk av nyremedisinerne i Kristiansand som også besøker dialysen i Flekkefjord 1 gang pr mnd. Generelle indremedisinske læringsmål i del 2 indremedisin dekkes alle tre steder, men de fleste læringsmålene i del 3 nyremedisin må dekkes i Arendal eller Kristiansand. LIS 3 i nyremedisin ved SSHF skal rotere i 6 mnd til Ullevål eller AHUS og 3 mnd til Rikshospitalet for å nå læringsmål i transplantasjonsmedisin. Om avdelingen/seksjonen i SSHF Medisinsk avdeling ligger under somatisk klinikk delt ved tre lokalisasjoner, Flekkefjord, Arendal og Kristiansand. Det er egne nyremedisinske seksjoner i Arendal og Kristiansand, mens i Flekkefjord ligger nyrepasientene i generell medisinsk avdeling ved innleggelse. Nyreseksjonen i Arendal har 6 senger som deles mellom hema/endo/nefro. Det er 3 overleger i nyremedisin som jobber ved avdelingen. Nyreseksjonen i Kristiansand har 4 senger. -

Årsrapport 2019 Årsberetning
Respekt, faglig dyktighet, tilgjengelighet og engasjement Flekkefjord Kristiansand Arendal Årsrapport 201 20149 Sørlandet sykehus HF - trygghet når du trenger det mest Innholdsfortegnelse Årsberetning 3 Resultatregnskap 13 Balanse 14 Kontantstrømoppstilling 15 Noter 16 Revisors beretning 32 2 Sørlandet sykehus HF Årsrapport 2019 Årsberetning Dette er Sørlandet sykehus gevinstrealisering i prosjektene. Bedre kvalitet i Sørlandet sykehus HF (SSHF) eies av det regionale pasientbehandlingen skal sikres gjennom arbeid med helseforetaket Helse Sør-Øst RHF. SSHF leverer helhetlige pasientforløp gjennom alle tjenesteledd. spesialisthelsetjenester til i overkant av 300 000 Arbeidet skal være kunnskapsbasert, og inkludere mennesker i sykehusområdet. Agder er primært forpliktende samhandling basert på avtaler med opptaksområde. I tillegg har SSHF regionale og kommunehelsetjenesten. nasjonale funksjoner. Programmet startet 01.03.2019 og det er satt i gang en SSHFs lovpålagte oppgaver er pasientbehandling, rekke prosjekter som følges opp fra programkontoret. forskning, utdanning av helsepersonell samt opplæring av pasienter og pårørende. Ansvarsområdene omfatter Hovedmål somatikk, psykisk helsevern, tverrfaglig spesialisert SSHF skal gi befolkningen i Agder tilgang til spesialist- rusbehandling, spesialisert rehabilitering, prehospitale helsetjenester slik dette er fastsatt i lover og forskrifter. tjenester og pasientreiser. SSHF skal innrette sin virksomhet med sikte på å nå følgende hovedmål gitt av Helse Sør-Øst RHF i Oppdrag SSHF har somatiske sykehus i Arendal, Kristiansand og bestilling 2019: og Flekkefjord. Psykiatrisk sykehusavdeling er lokalisert i Arendal og Kristiansand. Distrikts- 1. Redusere unødvendig venting og variasjon i psykiatriske og barne- og ungdomspsykiatriske enheter kapasitetsutnyttelsen ligger i kommunene Kristiansand, Mandal, Kvinesdal, 2. Prioritere psykisk helsevern og tverrfaglig Farsund, Flekkefjord, Arendal, Lillesand, Grimstad og spesialisert rusbehandling Tvedestrand. Det er polikliniske og døgnbaserte enheter innen rusbehandling i begge 3. -

01 Agder Kommunesammenslåing
Veien til færre og større Agder-kommuner Her er oversikt over status på prosessene SIRDAL: Ønsker primært å stå alene. Er også involvert i VEST-AGDER rundt kommunesammenslåing i alle mulighetsstudiet «Langfjella» (Sirdal, Valle, Bykle, Vinje, og Bygland), men har satt det på vent. 180 877 innbyggere AUST-AGDER kommunene i Agder-fylkene. ÅSERAL: Kommunestyret vedtok 25. juni med 9 mot 8 stemmer å stå alene. Alternativene er 114 767 innbyggere «Midtre Agder» og «Indre Agder» (Åseral, Bygland, Evje og Hornnes) Saken skal opp 1838 BYKLE 933 ÅMLI: SIRDAL Kommunestyret takket igjen 3. september, og det skal holdes BYKLE: rådgivende folkeavstemning 14. september. Kommunestyret vedtok 25. juni å 18. juni ja til videre UTSNITT utrede «nullalternativet». De vil sonderinger med også utrede sammenslåing med Froland. Takket også ja KVINESDAL: til sonderinger med ÅSERAL 925 Valle og Bygland i «Setesdal»- Foreløpig uklar situasjon, sak framlegges for alternativet, og ønsker drøftinger Nissedal i Telemark. formannskapet 1. september. Opprinnelig om aktuelle samarbeidsområder med i «Lister 5» som har strandet, «Lister 3» med Vinje og Sirdal. vil muligens bli vurdert. Men ønsker også VEGÅRSHEI: GJERSTAD: RISØR: 5948 Sirdal med på laget. KVINESDAL VALLE 1251 Kommunestyret vedtok Ønsker å gå videre med Bystyret oppfordret 28. mai de 16. juni at de er best «Østregionen» (Gjerstad, fire kommunene i «Østregionen» VALLE: tjent med å stå alene, Vegårdshei, Tvedestrand å utrede sammenslåing. HÆGEBOSTAD: Formannskapet vedtok 24. juni å Kommunestyret sa 18. juni ja til å forhandle både men vil også vurdere og Risør). Vurderer også Arbeidet med Østre Agder går utrede «nullaltenativet», altså å stå «Østre Agder» og om Åmli bør være med, parallelt, og kommunestyret om «Midtre Agder» (Marnardal, Audnedal, alene. -

Sluttrapport Fra Forvaltningskontroll Landbruk Evje Og Hornnes Og Iveland
Landbruksavdelingen Sluttrapport fra kontroll av forvaltningen av utvalgte tilskuddsordninger i landbruket – 2016 Kontrollert Evje og Hornnes og Iveland Kontrollpersoner fra Hans Bach- enhet kommuner Fylkesmannen i Evensen og Rolf Aust- og Vest-Agder Inge Pettersen Kontrollomfang Dato for sluttrapport 01.12.2016 -Avløsning ved sykdom og fødsel mv. - Tilskudd til spesielle miljøtiltak i landbruket (SMIL). Kommune Kontaktperson Evje og Hornnes og Iveland kommune Inge Eftevand Rapportens innhold Rapporten er utarbeidet etter gjennomført forvaltningskontroll i Iveland og Evje og Hornnes kommune innen ordningene med avløsning ved sykdom og fødsel mv. og tilskudd til spesielle miljøtiltak i landbruket (SMIL). Rapporten er utarbeidet som 1 rapport til begge kommunene siden det er felles forvaltning på de aktuelle landbrukstilskuddene. Den beskriver eventuelle avvik og merknader som ble avdekket innen de kontrollerte områdene. Avvik er mangel på oppfyllelse av krav fastsatt i lov, forskrift og/eller rundskriv. Merknad er forhold som ikke er i strid med krav, men der Fylkesmannen finner grunn til å påpeke behov for forbedring. Bakgrunn for kontrollen Fylkesmannen har det regionale ansvar for å sikre at statlige midler brukes og forvaltes i samsvar med forutsetningene. Forvaltningskontrollen har hjemmelsgrunnlag i Økonomireglementet i staten (§ 15) og bakgrunn i fullmaktsbrev fra Landbruksdirektoratet for 2016. Ved å avdekke eventuelle avvik og brudd på regelverk og rutiner vil dette kunne hjelpe kommunen fram mot en sikrere, bedre og mer effektiv forvaltning av tilskuddsordningene. Gjennomføring og omfang Kontrollen ble gjennomført som en dokumentkontroll. Fylkesmannen gjennomgikk forhåndsvalgte saker som kommunene hadde oversendt. Dette gjaldt 3 saker om tilskudd til avløsning til sykdom og fødsel mv. og 4 saker tilknyttet SMIL ordningen. -

Sparebanken Sør Boligkreditt AS
Sparebanken Sør Boligkreditt AS Investor Presentation March 2016 Executive summary . The fifth largest savings bank in Norway with a strong market position in Southern Norway . High capitalization; Capital ratio of 15.5 % - Core Tier 1 ratio of 12.7 % at December 31th 2015 Sparebanken Sør . Rated A1 (stable outlook) by Moody’s . Strong asset quality – 65 per cent of loan book to retail customers . New rights issue of NOK 600 million in progress will strengthen capital ratio even further . 100 % owned and dedicated covered bond subsidiary of Sparebanken Sør . Cover pool consisting of 100 % prime Norwegian residential mortgages Sparebanken Sør . High quality cover pool reflected by the weighted average LTV of 55.3 % Boligkreditt . Covered bonds rated Aaa by Moody’s with 5 notches of “leeway” . Strong legal framework for covered bonds in Norway with LTV limit of 75 % for residential mortgages . Low interest rates, weak NOK and fiscal stimulus are counterbalancing economic slowdown stemming from the lower oil investments . Unemployment is expected to increase gradually but from a very low level and the unemployment Norwegian rate remains well below the European levels economy . The Norwegian government has a strong financial position with large budget surplus. The government pension fund, which accounts over 200% of the GDP, provides the government with substantial economic leeway . The Southern region is clearly less exposed to oil production than Western Norway Southern region . Registered unemployment in the Southern region remains below -
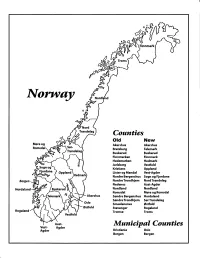
Norway Maps.Pdf
Finnmark lVorwny Trondelag Counties old New Akershus Akershus Bratsberg Telemark Buskerud Buskerud Finnmarken Finnmark Hedemarken Hedmark Jarlsberg Vestfold Kristians Oppland Oppland Lister og Mandal Vest-Agder Nordre Bergenshus Sogn og Fjordane NordreTrondhjem NordTrondelag Nedenes Aust-Agder Nordland Nordland Romsdal Mgre og Romsdal Akershus Sgndre Bergenshus Hordaland SsndreTrondhjem SorTrondelag Oslo Smaalenenes Ostfold Ostfold Stavanger Rogaland Rogaland Tromso Troms Vestfold Aust- Municipal Counties Vest- Agder Agder Kristiania Oslo Bergen Bergen A Feiring ((r Hurdal /\Langset /, \ Alc,ersltus Eidsvoll og Oslo Bjorke \ \\ r- -// Nannestad Heni ,Gi'erdrum Lilliestrom {", {udenes\ ,/\ Aurpkog )Y' ,\ I :' 'lv- '/t:ri \r*r/ t *) I ,I odfltisard l,t Enebakk Nordbv { Frog ) L-[--h il 6- As xrarctaa bak I { ':-\ I Vestby Hvitsten 'ca{a", 'l 4 ,- Holen :\saner Aust-Agder Valle 6rrl-1\ r--- Hylestad l- Austad 7/ Sandes - ,t'r ,'-' aa Gjovdal -.\. '\.-- ! Tovdal ,V-u-/ Vegarshei I *r""i'9^ _t Amli Risor -Ytre ,/ Ssndel Holt vtdestran \ -'ar^/Froland lveland ffi Bergen E- o;l'.t r 'aa*rrra- I t T ]***,,.\ I BYFJORDEN srl ffitt\ --- I 9r Mulen €'r A I t \ t Krohnengen Nordnest Fjellet \ XfC KORSKIRKEN t Nostet "r. I igvono i Leitet I Dokken DOMKIRKEN Dar;sird\ W \ - cyu8npris Lappen LAKSEVAG 'I Uran ,t' \ r-r -,4egry,*T-* \ ilJ]' *.,, Legdene ,rrf\t llruoAs \ o Kirstianborg ,'t? FYLLINGSDALEN {lil};h;h';ltft t)\l/ I t ,a o ff ui Mannasverkl , I t I t /_l-, Fjosanger I ,r-tJ 1r,7" N.fl.nd I r\a ,, , i, I, ,- Buslr,rrud I I N-(f i t\torbo \) l,/ Nes l-t' I J Viker -- l^ -- ---{a - tc')rt"- i Vtre Adal -o-r Uvdal ) Hgnefoss Y':TTS Tryistr-and Sigdal Veggli oJ Rollag ,y Lvnqdal J .--l/Tranbv *\, Frogn6r.tr Flesberg ; \. -

NIVI-Rapport 2012:3 Endret Fylkestilknytning for Evje Og
NIVI-rapport 2012:3 Endret fylkestilknytning for Evje og Hornnes, Birkenes, Iveland og Lillesand kommuner? En konsekvensvurdering Utarbeidet på oppdrag av Kommunal- og regionaldepartementet Jørund K Nilsen og Magne Langset April 2012 Innhold: SAMMENDRAG ..................................................................................................... 1 1. MÅL OG RAMMER FOR OPPDRAGET .................................................. 11 1.1 Historikk og bakgrunn ....................................................................... 11 1.2 Formål og problemstillinger .............................................................. 13 1.3 Metode ............................................................................................... 13 2. AGDER-FYLKENE OG SØKERKOMMUNENE ..................................... 14 2.1 Agder-fylkene .................................................................................... 14 2.2 Søkerkommunene .............................................................................. 15 2.3 Regionråd og formaliserte samarbeidsordninger ............................... 17 2.4 Kommunenes deltakelse i formaliserte samarbeidsordninger ........... 18 3. KONSEKVENSER FOR FYLKESKOMMUNENE ................................... 20 3.1 Inndelingslovens bestemmelser ved grensejustering ......................... 20 3.2 Videregående opplæring .................................................................... 20 3.3 Tannhelse ........................................................................................... 25 -

Arendal Prison
VISIT REPORT SUMMARY AND RECOMMENDATIONS Arendal Prison 7-8 February 2018 National Preventive Mechanism against Torture and Ill-Treatment Visit report Arendal Prison 7–8 February 2018 VISIT REPORT Arendal Prison 7-8 February 2018 1 Visit report Arendal Prison 7–8 February 2018 Table of content 1 The Parliamentary Ombudsman's prevention mandate ................................ 3 2 Summary ............................................................................................. 4 3 Recommendations ................................................................................. 6 2 Visit report Arendal Prison 7–8 February 2018 1 The Parliamentary Ombudsman's prevention mandate As a result of Norway's ratification of the Optional Protocol to the UN Convention against Torture in 2013, the Parliamentary Ombudsman was issued with a special mandate to prevent torture and other cruel, inhuman or degrading treatment or punishment.1 The Parliamentary Ombudsman has established its own National Preventive Mechanism (NPM) in order to fulfil this mandate. The NPM regularly visits locations where people are deprived of their liberty, such as prisons, police custody facilities, mental health care institutions and child welfare institutions. The visits can be both announced and unannounced. The Parliamentary Ombudsman has right of access to all places of detention and the right to speak in private with people who have been deprived of their liberty. The Parliamentary Ombudsman also has right of access to all necessary information that is relevant to the conditions for people deprived of their liberty. The risk of torture or ill-treatment occurring is influenced by factors such as legal and institutional frameworks, physical conditions, training, resources, management and institutional culture.2 Effective prevention work therefore requires a broad approach that does not exclusively focus on whether the situation complies with Norwegian law. -

GRID-Arendal Annual Report 2018
29 and counting GRID-Arendal Annual Report 2018 Established in 1989 as a non-profit foundation under Norwegian law, GRID-Arendal’s mission is to create environmental knowledge that encourages positive change. We do this by organising and transforming available environmental data into credible, science-based information products, delivered through innovative communication tools and capacity building services targeting relevant stakeholders. GRID-Arendal works closely with United Nations Environment, other UN agencies and partners around the world to connect science to policy. Our goal is to shorten the distance between the emergence of new science and policy actions. We seek to influence thinking and action at the level of the global community on issues that require collective efforts because many problems cannot be solved at the national level alone. Acknowledgements GRID-Arendal would like to acknowledge the support of the Government of Norway and its other funders, partners and supporters. Contents Foreword 3 From the desk of the Managing Director 5 Stories 6 Action to make mine waste dams safer 8 Participatory mapping in Vietnam 9 On the coast of West Africa 10 Helping Vanuatu and France hold historic meeting 11 Blue Carbon 12 Success in the Caspian Sea 13 And Caspian sturgeon better protected 14 Marine plastic pollution in the Arctic 15 © GRID-Arendal, 2018 Marine litter – research, not talking trash 16 Publication: GRID-Arendal 2018 Annual Report Sanitation and wastewater in Africa 17 ISBN: 978-82-7701-188-2 IW:LEARN 18 This publication may be reproduced in whole or in part and in any form Moving mountains (onto the agenda) 19 for educational or non-profit purposes without special permission from the copyright holder provided acknowledgement of the source is made. -

Topp 20 Turar I Åmli
Topp 20 turar i Åmli TOP 20 HIKING TRAILS IN ÅMLI TOP 20 WANDERROUTEN IN ÅMLI www.visitsorlandet.com Topp 20 i Åmli – 20 gode turforslag i Åmli Dette er moro for både store symbol med grad av kor vanskeleg SKOGBRANNFARE og små, og ein fin måte å ein antek at løypa er. Turløypene er Frå 15. april til 15. september er det kome seg ut på tur. Nokre av merka med blå merke i terrenget. forbode å gjere opp bål og bruke eld løypene er også egna for skigåing i eller i nærleiken av skogsmark. om vinteren. REGISTRERING OG PREMIERING Tlf. brannvesen: 110 På kvar topp er det ei kasse med Brosjyre med klippekort kan du få på gjestebok og klippetang. Ver snill BANDTVANG følgjande stader: og skriv deg inn i denne. Hugs å Hundar skal vere i band i perioden Rådhuset i Åmli registrere turen på klippekortet 1. april til 20. august. Laushundar kan Åmfoss kafeteria (baksida av denne brosjyra) med avlivast på staden dersom dei jagar Esso, Åmli sentrum klippetanga. vilt eller husdyr. Hillestad Galleri Vindilhytta Når du har registrert deg på alle top- ELGJAKT Elvarheim Museum pane, kan du få ei t-skjorte. Alle som Frå og med 25. september blir det Nelaug Daglegvare leverer inn fullt klippekort får til- jakta elg i store delar av turområda. sendt t-skjorte. Barn til og med 12 år Det oppmodast om å ta omsyn til Brosjyra kan du og finne i ein boks på må ha gått 15 valfrie løyper for å få dette og om mogleg legge turen til infotavla for kvar løype. -

FV 43 Listervegen - Brogata Farsund Kommune Reguleringsbestemmelser, Retningslinjer Og Planbeskrivelse
FV 43 Listervegen - Brogata Farsund kommune Reguleringsbestemmelser, retningslinjer og planbeskrivelse Region sør Arendal, R.vegktr Plan og prosjektering Agder Høringsutkast Revidert dato:27.11.2012 Reguleringsplan planbeskrivelse Fv 43 – Listervegen – Brogata i Farsund. 1 Reguleringsplan planbeskrivelse Statens vegvesen region sør Fv. 43 Listervegen – Brogata gjennom Farsund sentrum. Reguleringsplan Fv 43 – Listervegen – Brogata i Farsund. 2 Reguleringsplan planbeskrivelse Fv 43 – Listervegen – Brogata i Farsund. 3 Reguleringsplan planbeskrivelse Forord Reguleringsplanforslaget er utarbeidet av Statens vegvesen Region sør. Prosjektleder hos Statens vegvesen er Øystein Lien. Ansvarlig for prosjektgjennomføringer har vært Anlaug Konnestad Nordal og Øystein Bedford Pedersen. Formålet med planarbeidet for Fv. 43 Listervegen - Brogata gjennom Farsund sentrum er å bedre fremkommelighet og trafikksikkerheten for gående og syklende, utbedre kurver og stigninger, bedre sikt og stigningsforhold i avkjørsler, utforming av ny gate, utrede støy. Støytiltak vil bli foreslått i forbindelse med utarbeidelse av byggeplan og i samråd med grunneiere. Statens vegvesen har hatt ansvar for det praktiske planarbeidet. Statens vegvesen er forslagsstiller for reguleringsplanen. Planen består av følgende dokumenter: • Planbeskrivelse for reguleringsplan og reguleringsbestemmelser (dette dokument). • Reguleringsplankart i målestokk 1: 1000 (vedlegg til dette dokument). • Risikovurdering, 2010 (eget vedlegg). • Støyrapport, 2012 (eget vedlegg). • Barnetråkkundersøkelsen.