David Mccarty [email protected] Ph.D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Galeterone for the Treatment of Castration- Resistant Prostate Cancer Bruce Montgomery1, Mario A
Published OnlineFirst November 2, 2015; DOI: 10.1158/1078-0432.CCR-15-1432 Cancer Therapy: Clinical Clinical Cancer Research Androgen Receptor Modulation Optimized for Response (ARMOR) Phase I and II Studies: Galeterone for the Treatment of Castration- Resistant Prostate Cancer Bruce Montgomery1, Mario A. Eisenberger2, Matthew B. Rettig3, Franklin Chu4, Roberto Pili5, Joseph J. Stephenson6, Nicholas J. Vogelzang7, Alan J. Koletsky8, Luke T. Nordquist9, William J. Edenfield10, Khalid Mamlouk11, Karen J. Ferrante11, and Mary-Ellen Taplin12 Abstract Purpose: Galeterone is a selective, multitargeted agent that Results: In ARMOR1, across all doses, 49.0% (24/49) achieved a inhibits CYP17, antagonizes the androgen receptor (AR), and 30% decline in prostate-specific antigen (PSA; PSA30) and reduces AR expression in prostate cancer cells by causing an 22.4% (11/49) demonstrated a 50% PSA decline (PSA50). In increase in AR protein degradation. These open-label phase I ARMOR2 part 1, across all doses, PSA30 was 64.0% (16/25) and and II studies [Androgen Receptor Modulation Optimized PSA50 was 48.0% (12/25). In the 2,550-mg dose cohort, PSA30 for Response-1 (ARMOR1) and ARMOR2 part 1] evaluated was 72.7% (8/11) and PSA50 was 54.5% (6/11). Galeterone was the efficacy and safety of galeterone in patients with treat- well tolerated; the most common adverse events were fatigue, ment-naive nonmetastatic or metastatic castration-resistant increased liver enzymes, gastrointestinal events, and pruritus. Most prostate cancer (CRPC) and established a dose for further were mild or moderate in severity and required no action and there study. were no apparent mineralocorticoid excess (AME) events. -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -
Download Product Insert (PDF)
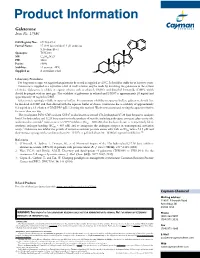
Product Information Galeterone Item No. 17586 N CAS Registry No.: 851983-85-2 Formal Name: 17-(1H-benzimidazol-1-yl)-androsta- 5,16-dien-3β-ol N Synonym: TOK-001 MF: C26H32N2O FW: 388.6 H Purity: ≥98% H H Stability: ≥2 years at -20°C Supplied as: A crystalline solid HO Laboratory Procedures For long term storage, we suggest that galeterone be stored as supplied at -20°C. It should be stable for at least two years. Galeterone is supplied as a crystalline solid. A stock solution may be made by dissolving the galeterone in the solvent of choice. Galeterone is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF), which should be purged with an inert gas. The solubility of galeterone in ethanol and DMSO is approximately 20 mg/ml and approximately 30 mg/ml in DMF. Galeterone is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, galeterone should first be dissolved in DMF and then diluted with the aqueous buffer of choice. Galeterone has a solubility of approximately 0.2 mg/ml in a 1:3 solution of DMF:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. The cytochrome P450 (CYP) isoform CYP17 is also known as steroid 17α-hydroxylase/17,20 lyase because it catalyzes both 17α-hydroxylase and 17,20 lyase reactions in the synthesis of steroids, including androgens, estrogens, glucocorticoids, 1 and mineralocorticoids. Galeterone is a CYP17 inhibitor (IC50 = 300 nM) that has been shown to competitively block synthetic androgen binding (EC50 = 845 nM) and to antagonize the androgen receptor in transcriptional activation 2 assays. -

Therapies Targeted to Androgen Receptor Signaling Axis in Prostate Cancer: Progress, Challenges, and Hope
cancers Review Therapies Targeted to Androgen Receptor Signaling Axis in Prostate Cancer: Progress, Challenges, and Hope Sirin Saranyutanon 1,2, Sanjeev Kumar Srivastava 1,2,*, Sachin Pai 3, Seema Singh 1,2,4 and Ajay Pratap Singh 1,2,4,* 1 Department of Pathology, College of Medicine, University of South Alabama, Mobile, AL 36617, USA; [email protected] (S.S.); [email protected] (S.S.) 2 Department of Oncologic Sciences, Mitchell Cancer Institute, University of South Alabama, Mobile, AL 36604, USA 3 Department of Medical Oncology, Mitchell Cancer Institute, University of South Alabama, Mobile, AL 36604, USA; [email protected] 4 Department of Biochemistry and Molecular Biology, College of Medicine, University of South Alabama, Mobile, AL 36688, USA * Correspondence: [email protected] (S.K.S.); [email protected] (A.P.S.); Tel.: +1-251-445-9874 (S.K.S.); +1-251-445-9843 (A.P.S.) Received: 4 November 2019; Accepted: 18 December 2019; Published: 23 December 2019 Abstract: Prostate cancer is the mostly commonly diagnosed non-cutaneous malignancy and the second leading cause of cancer-related death affecting men in the United States. Moreover, it disproportionately affects the men of African origin, who exhibit significantly greater incidence and mortality as compared to the men of European origin. Since androgens play an important role in the growth of normal prostate and prostate tumors, targeting of androgen signaling has remained a mainstay for the treatment of aggressive prostate cancer. Over the years, multiple approaches have been evaluated to effectively target the androgen signaling pathway that include direct targeting of the androgens, androgen receptor (AR), AR co-regulators or other alternate mechanisms that impact the outcome of androgen signaling. -

Development of Combination Therapy for Prostate Cancer
DEVELOPMENT OF COMBINATION THERAPY FOR PROSTATE CANCER A Dissertation Presented to the Faculty of the Weill Cornell Graduate School of Medical Sciences in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy by Alexander R. Root July 2017 © 2017 Weill Cornell Graduate School of Medical Sciences ALL RIGHTS RESERVED DEVELOPMENT OF COMBINATION THERAPY FOR PROSTATE CANCER Alexander R. Root, Ph.D. Cornell University 2017 There is an unmet need in prostate cancer for effective therapies to prevent the emergence of resistance. Combinations of small molecules targeting key pathways are a promising strategy. I investigated how populations of the early metastatic prostate cancer cell line LNCaP respond at the proteomic and pheno- typic levels to six clinically-relevant, one-drug treatments and their 15 pairs of two-drug combinations, administered simultaneously to treatment-naive cells. After 24 hours of drug addition for all 21 drug treatments I measured 52 total- proteins by selected-reaction monitoring mass-spectrometry based proteomics (SRM), 20 phospho-proteins, and 50 total-proteins by reverse-phase protein ar- rays (RPPA). I measured phenotypic effects on cell proliferation and apoptosis in all conditions using phase-contrast and fluorescence microscopy. Network analysis identified (phospho)-proteins with large responses to drug treatments that are druggable with FDA-approved drugs or have nearest-neighbors that are druggable. A total of ten drugs targeting these nearest responder (phospho)-proteins were tested in single, double, and triple combinations. I found that 7 out of 10 triple combinations co-targeting androgen receptor and PI3K pathways were no more effective than the two-drug combination at the doses tested: PRKC (en- zastaurin), MAPK (losmapimod), STAT3 (napabucasin), HDAC (panobinostat), SRC (saracatinib), casein kinase (silmitasertib), MAPK (ulixertinib). -

( 12 ) United States Patent
US010314797B2 (12 ) United States Patent ( 10 ) Patent No. : US 10 , 314 ,797 B2 Narayanan et al. ( 45 ) Date of Patent : * Jun . 11, 2019 ( 54 ) SELECTIVE ANDROGEN RECEPTOR ( 56 ) References Cited DEGRADER (SARD ) LIGANDS AND METHODS OF USE THEREOF U . S . PATENT DOCUMENTS 5 ,480 ,656 A 1 / 1996 Okada et al . (71 ) Applicant: University of Tennessee Research 5 ,575 , 987 A 11/ 1996 Kamei et al . Foundation , Knoxville , TN (US ) 5 ,631 , 020 A 5 / 1997 Okada et al. 5 , 643 ,607 A 7 / 1997 Okada et al. 5 ,716 ,640 A 2 / 1998 Kamei et al. ( 72 ) Inventors : Ramesh Narayanan , Cordova , TN 5 , 814 ,342 A 9 / 1998 Okada et al . (US ) ; Duane D . Miller , Collierville , 6 ,036 , 976 A 3 / 2000 Takechi et al . TN (US ) ; Thamarai Ponnusamy , 7 , 118 , 552 B2 10 / 2006 Shaw et al . Memphis , TN (US ); Dong - Jin Hwang, 7 , 220 , 247 B25 / 2007 Shaw et al . 7 ,500 , 964 B23 / 2009 Shaw et al . Arlington , TN (US ) ; Yali He, 9 ,815 , 776 B2 * 11 / 2017 Narayanan . .. .. C07C 255 /60 Germantown , TN (US ) 9 , 834 , 507 B2 * 12 / 2017 Narayanan . .. .. .. C07C 255 /60 2005 /0101657 A1 5 /2005 Furuya et al . (73 ) Assignee : University of Tennessee Research 2007 /0265290 A1 11/ 2007 Dalton et al . 2010 /0227846 AL 9 /2010 Ito et al. Foundation , Knoxville , TN ( US ) 2014 / 0018433 A11 / 2014 Dalton et al . ( * ) Notice : Subject to any disclaimer , the term of this 2018 /0118663 A1 * 5 / 2018 Narayanan . C07C 237/ 20 patent is extended or adjusted under 35 FOREIGN PATENT DOCUMENTS U . S . -

Metabolic Enzyme/Protease
Inhibitors, Agonists, Screening Libraries www.MedChemExpress.com Metabolic Enzyme/Protease Metabolic pathways are enzyme-mediated biochemical reactions that lead to biosynthesis (anabolism) or breakdown (catabolism) of natural product small molecules within a cell or tissue. In each pathway, enzymes catalyze the conversion of substrates into structurally similar products. Metabolic processes typically transform small molecules, but also include macromolecular processes such as DNA repair and replication, and protein synthesis and degradation. Metabolism maintains the living state of the cells and the organism. Proteases are used throughout an organism for various metabolic processes. Proteases control a great variety of physiological processes that are critical for life, including the immune response, cell cycle, cell death, wound healing, food digestion, and protein and organelle recycling. On the basis of the type of the key amino acid in the active site of the protease and the mechanism of peptide bond cleavage, proteases can be classified into six groups: cysteine, serine, threonine, glutamic acid, aspartate proteases, as well as matrix metalloproteases. Proteases can not only activate proteins such as cytokines, or inactivate them such as numerous repair proteins during apoptosis, but also expose cryptic sites, such as occurs with β-secretase during amyloid precursor protein processing, shed various transmembrane proteins such as occurs with metalloproteases and cysteine proteases, or convert receptor agonists into antagonists and vice versa such as chemokine conversions carried out by metalloproteases, dipeptidyl peptidase IV and some cathepsins. In addition to the catalytic domains, a great number of proteases contain numerous additional domains or modules that substantially increase the complexity of their functions. -

DHEA, the Most Abundant Steroid Hormone in the Body
CHAPTER 50 DHEA, the most abundant steroid hormone in the body: inhibits glucose-6-phosphate dehydrogenase, inhibits the generation of NADPH, activates the pyruvate dehydrogenase complex and increases oxidative phosphorylation, increases oxidative stress, polarizes the immune system to M1/Th1, inhibits the pathway PI3K/Akt and decreases proliferation and increases apoptosis in cancer José de Felippe Junior DHEA: substance synthesized in the body with multiple actions – Plasma DHEA-sulphate declines from a peak at age maintain health, prevent diseases and help to heal them. JFJ 20, in both men and women. In men, DHEA-s ranges Warning: your adrenal gland is prohibited from making DHEA from 11 to 2.5 microM and in women from 6 to 1 mi- if you live in Brazil. Nonconformist medical doctors croM, from 20 to 80 years respectively (Labrie-1997). The DHEA biological actions involve multiple re- ceptors. DHEA binds to steroid/nuclear receptors (e.g. DHEA in United States of America is considered as a pregnane X receptor/steroid and xenobiotic receptor or food supplement, in Europe as a hormone that requires PXR/SXR), estrogen receptors alpha, beta (ER-alpha medical prescription (Samaras-2013) and in Brazil, for and ER-beta), androgen (AR), cellular membrane re- reasons unknown, it is prohibited the commercializa- ceptors and endothelial cells receptors (activating tion and prescription. G-receptor-coupled proteins – GPCR) (Webb-2006, in Dehydroepiandrosterone – DHEA – is produced in Teng-2015). cortical adrenal gland and activated by sulfation in the It was found in Japanese with over 100 years in- liver and target organs. DHEA is the steroid hormone crease in telomere length in leukocytes, increased adi- or steroid pre-hormone in the highest amount in the ponectin concentration along with normal levels of body: 72% of the total (Ebeling-1994, Traish-2011). -

1 Activity of Galeterone in Hepatocellular Carcinoma And
Activity of Galeterone in Hepatocellular Carcinoma and Description of Androgen Receptor Expression in Mouse Liver Undergraduate Research Thesis By Riley Mullins The Ohio State University May 2019 Project Advisor: Dr. Chris Coss, Department of Pharmaceutics and Pharmaceutical Chemistry 1 ABSTRACT Globally, liver cancer is the sixth most commonly diagnosed cancer, fourth leading cause of cancer deaths, and has increasing incidence and mortality rates [1]. Hepatocellular carcinoma (HCC) is the dominant form of liver cancer [1]. Although HCC treatments are improving, the 5-year survival rate in the United States remains low at 18% [2, 3]. A 3-fold higher prevalence of HCC in men than women suggests androgens, such as testosterone, promote the disease. Androgens bind and activate the androgen receptor (AR), a transcription factor that regulates a diverse set of genes. Despite evidence that AR contributes to HCC, traditional antiandrogen therapies, which are steroid-competitive at the ligand binding domain of AR, are ineffective in treating advanced HCC [4]. In primary HCC patient samples and HCC cell lines, we identified alternatively-spliced forms of AR (ARsvs) that lack the ligand binding domain, are constitutively active, and are unaffected by traditional antiandrogens (unpublished). We hypothesize that full-length AR and ARsvs contribute to liver disease progression, and novel selective AR degraders (SARDs) will have anti-HCC activity by inhibiting all forms of AR. The data support that pharmacologic activation or inhibition of full-length AR does not affect HCC cell line proliferation. However, a novel SARD, galeterone, decreases proliferation potentially by inhibiting full-length AR, ARsvs, and mTOR signaling. Future work aims to identify and investigate signaling through AR in immune and non-immune cells of the liver that is relevant to disease. -

Cphi & P-MEC China Exhibition List展商名单version版本20180308
CPhI & P-MEC China Exhibition List展商名单 Version版本 20180308 Booth/ Company Name/公司中英文名 Product/产品 展位号 Carbosynth Ltd E1A01 IPTG,EDAC HCl,2-脱氧-D-核糖IPTG,EDAC HCl,2-deoxy-D-ribose Analytical standards,Natural products,Amino acids and peptides,Steroids,API’s, impurities, and metabolites,Stable isotope labelled analogues,Building blocks,Chiral molecules,Carbohydrates and oligosaccharides,Nucleic acid derivatives,Enzyme Toronto Research Chemicals Inc E1A08 activators and inhibitors,Sulfhydryl active agents,Fluorescent reagents,Spin labels,Nicotine derivatives and metabolites,Neurochemicals,Environmental standards,mutagens, and metabolites,Phthalates,Retinoids,Vitamin D derivatives,Drugs of abuse for forensic testing,Phosphates SiliaMetS,SiliaCat,SiliaFlash,SiliaBond,Metal Scavenger,Catalyst,silica SiliCycle Inc. E1A10 gel,chromatographic phases SA TOURNAIRE E1A11 铝,包装,瓶,原料药Aluminum,Bottle,Packaging,API 紫杉醇,多西他赛,秋水仙碱,利血平,硫秋水仙碱苷,欧洲越橘,葡萄籽,银杏叶,姜黄,橄榄果,绿茶,水飞 蓟,乳香,锯叶棕,积雪草Paclitaxel,Docetaxel, Indena SpA E1A17 Colchicine,Reserpine,Thiocolchicoside,Bilberry,Grape Seed,Ginkgo Biloba,Curcumin,Olive,Green Tea, Silymarin, Boswellia,Saw Palmetto,Centella Asiatica Chempro Pharma PVT LTD E1A19 Trifarma E1A21 LLC Velpharma E1A25 Anuh Pharma E1A31 Moehs Iberica S.L E1A32 BROMOBENZENE,N PROPYL BROMIDE,SODIUM BROMIDE,ETHYL Chemclone Industries E1A51 BROMIDEBROMOBENZENE,NPROPYL BROMIDE,SODIUM BROMIDE,ETHYL BROMIDE Chemwerth Inc. E1B01 Hetero Labs Limited E1B09 Tacrolimus,Mycophenolate Mofetil,Mycophenolate Sodium,Cyclosporine,Sirolimus,Pimecrolimus,Temsirolimus,Everolimus,Romidepsin,Mitomyci -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic