Case Report Long-Lasting Fever and Lymphadenitis: Think About F. Tularensis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Blood Smear Analysis in Babesiosis, Ehrlichiosis, Relapsing Fever, Malaria, and Chagas Disease
REVIEW STEVE M. BLEVINS, MD RONALD A. GREENFIELD, MD* MICHAEL S. BRONZE, MD CME Assistant Professor of Medicine, Section Professor of Medicine, Section of Infectious Professor of Medicine, Section of Infectious CREDIT of General Internal Medicine, Department Diseases, Department of Medicine, University Diseases, Chair of Department of Medicine, of Medicine, University of Oklahoma of Oklahoma Health Sciences Center and the University of Oklahoma Health Sciences Center Health Sciences Center, Oklahoma City Oklahoma City Veterans Administration and the Oklahoma City Veterans Administration Medical Center Medical Center Blood smear analysis in babesiosis, ehrlichiosis, relapsing fever, malaria, and Chagas disease ■ ABSTRACT LOOD SMEAR ANALYSIS, while commonly B used to evaluate hematologic condi- Blood smear analysis is especially useful for diagnosing tions, is infrequently used to diagnose infec- five infectious diseases: babesiosis, ehrlichiosis, relapsing tious diseases. This is because of the rarity of fever due to Borrelia infection, malaria, and American diseases for which blood smear analysis is indi- trypanosomiasis (Chagas disease). It should be performed cated. Consequently, such testing is often in patients with persistent or recurring fever or in those overlooked when it is diagnostically impor- who have traveled to the developing world or who have tant. a history of tick exposure, especially if accompanied by Nonspecific changes may include mor- hemolytic anemia, thrombocytopenia, or phologic changes in leukocytes and erythro- 1 hepatosplenomegaly. cytes (eg, toxic granulations, macrocytosis). And with certain pathogens, identifying ■ KEY POINTS organisms in a peripheral blood smear allows for a rapid diagnosis. In the United States, malaria and American This paper discusses the epidemiology, trypanosomiasis principally affect travelers from the clinical manifestations, laboratory findings, developing world. -

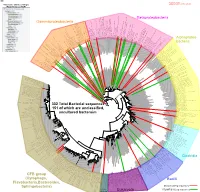
Genetic Diversity of Bartonella Species in Small Mammals in the Qaidam
www.nature.com/scientificreports OPEN Genetic diversity of Bartonella species in small mammals in the Qaidam Basin, western China Huaxiang Rao1, Shoujiang Li3, Liang Lu4, Rong Wang3, Xiuping Song4, Kai Sun5, Yan Shi3, Dongmei Li4* & Juan Yu2* Investigation of the prevalence and diversity of Bartonella infections in small mammals in the Qaidam Basin, western China, could provide a scientifc basis for the control and prevention of Bartonella infections in humans. Accordingly, in this study, small mammals were captured using snap traps in Wulan County and Ge’ermu City, Qaidam Basin, China. Spleen and brain tissues were collected and cultured to isolate Bartonella strains. The suspected positive colonies were detected with polymerase chain reaction amplifcation and sequencing of gltA, ftsZ, RNA polymerase beta subunit (rpoB) and ribC genes. Among 101 small mammals, 39 were positive for Bartonella, with the infection rate of 38.61%. The infection rate in diferent tissues (spleens and brains) (χ2 = 0.112, P = 0.738) and gender (χ2 = 1.927, P = 0.165) of small mammals did not have statistical diference, but that in diferent habitats had statistical diference (χ2 = 10.361, P = 0.016). Through genetic evolution analysis, 40 Bartonella strains were identifed (two diferent Bartonella species were detected in one small mammal), including B. grahamii (30), B. jaculi (3), B. krasnovii (3) and Candidatus B. gerbillinarum (4), which showed rodent-specifc characteristics. B. grahamii was the dominant epidemic strain (accounted for 75.0%). Furthermore, phylogenetic analysis showed that B. grahamii in the Qaidam Basin, might be close to the strains isolated from Japan and China. -

Tick-Borne Relapsing Fever CLAY ROSCOE, M.D., and TED EPPERLY, M.D., Family Medicine Residency of Idaho, Boise, Idaho
Tick-Borne Relapsing Fever CLAY ROSCOE, M.D., and TED EPPERLY, M.D., Family Medicine Residency of Idaho, Boise, Idaho Tick-borne relapsing fever is characterized by recurring fevers separated by afebrile periods and is accompanied by nonspecific constitutional symptoms. It occurs after a patient has been bitten by a tick infected with a Borrelia spirochete. The diagnosis of tick-borne relapsing fever requires an accurate characterization of the fever and a thorough medical, social, and travel history of the patient. Findings on physical examination are variable; abdominal pain, vomiting, and altered sensorium are the most common symptoms. Laboratory confirmation of tick-borne relapsing fever is made by detection of spirochetes in thin or thick blood smears obtained during a febrile episode. Treatment with a tetracycline or macrolide antibiotic is effective, and antibiotic resistance is rare. Patients treated for tick-borne relapsing fever should be monitored closely for Jarisch- Herxheimer reactions. Fatalities from tick-borne relapsing fever are rare in treated patients, as are subsequent Jarisch-Herxheimer reactions. Persons in endemic regions should avoid rodent- and tick-infested areas and use insect repellents and protective clothing to prevent tick bites. (Am Fam Physician 2005;72:2039-44, 2046. Copyright © 2005 American Academy of Family Physicians.) S Patient information: ick-borne relapsing fever (TBRF) develop with TBRF, with long-term sequelae A handout on tick-borne is transmitted by Ornithodoros that may be permanent. Reviewing a broad relapsing fever, written by 1,3-6 the authors of this article, ticks infected with one of sev- differential diagnosis (Table 1 ) for fever is provided on page 2046. -
Lyme Disease and Tick-Borne Infections User Manual
SCOTTISH MICROBIOLOGY REFERENCE LABORATORY, INVERNESS: LYME DISEASE AND TICK-BORNE INFECTIONS USER MANUAL 1 Amended 23 September 2020 CONTENTS Section Page 1 Introduction 3 2 Contact details and key personnel 3 3 Opening hours 4 4 Service provided 4 4.1 Samples and turnaround times 4 4.2 Laboratory tests 5 4.3 Specialist advice 5 5 Clinical Information 6 6 Referral criteria 6 7 Specimen and request form labelling 7 8 Specimen transportation 8 9 Charges 8 10 Results 8 11 Treatment 8 12 Prevention 8 13 SLDTRL request form 8 (Form MF023) 14 SLDTRL developments 9 15 References 9 16 Laboratory diagnosis of Lyme borreliosis algorithm Appendix 2 Amended 23 September 2020 1.0 Introduction The newly established Scottish Lyme Disease and Tick-borne Infections Reference Laboratory (SLDTRL) is provided by NHS Highland at Raigmore Hospital, Inverness. The aim of SLDTRL is to provide more comprehensive and standardised testing for Lyme disease and other tick-borne infections and to improve the epidemiological data provided to Health Protection Scotland (HPS). Lyme disease is caused by bacteria from the Borrelia burgdorferi sensu lato complex. In the UK the bacteria is transmitted to humans through the bite of infected, hard bodied, Ixodes ricinus ticks. Borrelia miyamotoi disease, which presents as a relapsing fever, can also be transmitted by Ixodes ricinus ticks. It is an emerging disease caused by B. miyamotoi bacteria, which are from the relapsing fever group of borrelia, genetically distinct from those that cause Lyme disease. Human granulocytic anaplasmosis (HGA), also an acute febrile illness transmitted by Ixodid ticks, is an infection caused by the bacterium Anaplasma phagocytophilum. -

Bartonella Henselae Detected in Malignant Melanoma, a Preliminary Study
pathogens Article Bartonella henselae Detected in Malignant Melanoma, a Preliminary Study Marna E. Ericson 1, Edward B. Breitschwerdt 2 , Paul Reicherter 3, Cole Maxwell 4, Ricardo G. Maggi 2, Richard G. Melvin 5 , Azar H. Maluki 4,6 , Julie M. Bradley 2, Jennifer C. Miller 7, Glenn E. Simmons, Jr. 5 , Jamie Dencklau 4, Keaton Joppru 5, Jack Peterson 4, Will Bae 4, Janet Scanlon 4 and Lynne T. Bemis 5,* 1 T Lab Inc., 910 Clopper Road, Suite 220S, Gaithersburg, MD 20878, USA; [email protected] 2 Intracellular Pathogens Research Laboratory, Comparative Medicine Institute, College of Veterinary Medicine, North Carolina State University, Raleigh, NC 27607, USA; [email protected] (E.B.B.); [email protected] (R.G.M.); [email protected] (J.M.B.) 3 Dermatology Clinic, Truman Medical Center, University of Missouri, Kansas City, MO 64108, USA; [email protected] 4 Department of Dermatology, University of Minnesota, Minneapolis, MN 55455, USA; [email protected] (C.M.); [email protected] (A.H.M.); [email protected] (J.D.); [email protected] (J.P.); [email protected] (W.B.); [email protected] (J.S.) 5 Department of Biomedical Sciences, Duluth Campus, Medical School, University of Minnesota, Duluth, MN 55812, USA; [email protected] (R.G.M.); [email protected] (G.E.S.J.); [email protected] (K.J.) 6 Department of Dermatology, College of Medicine, University of Kufa, Kufa 54003, Iraq 7 Galaxy Diagnostics Inc., Research Triangle Park, NC 27709, USA; [email protected] Citation: Ericson, M.E.; * Correspondence: [email protected]; Tel.: +1-720-560-0278; Fax: +1-218-726-7906 Breitschwerdt, E.B.; Reicherter, P.; Maxwell, C.; Maggi, R.G.; Melvin, Abstract: Bartonella bacilliformis (B. -

IS IT LYME DISEASE, Or TICK-BORNE RELAPSING FEVER?
IS IT LYME DISEASE, or TICK-BORNE RELAPSING FEVER? Webinar Presented by Joseph J. Burrascano Jr. M.D. Joined by Jyotsna Shah PhD for the Q&A January 2020 Presenters Joseph J. Burrascano Jr. M.D. • Well-known pioneer in the field of tick-borne diseases, active since 1985 • Founding member of ILADS and ILADEF • Active in physician education on all aspects of tick-borne diseases Jyotsna Shah, PhD • President & Laboratory Director of IGeneX Clinical Laboratory • Over 40 Years of Research Experience in Immunology, Molecular Biology & Microbiology • Author of Multiple Publications & Holds More Than 20 Patents • Member of ILRAD as a Post-Doctoral Scientist • Started the First DNA Sequencing Laboratory in E. Africa 2 Poll Question Before we begin, we’d like to ask a poll question. Which one of these Borrelia causes Tick-Borne Relapsing Fever (TBRF)? a) B. mayonii b) B. turicatae c) B. burgdorferi d) B. andersonii e) B. garinii 3 Poll Question Before we begin, we’d like to ask a poll question. Which one of these Borrelia causes Tick-Borne Relapsing Fever (TBRF)? a) B. mayonii - Lyme b) B. turicatae - TBRF c) B. burgdorferi - Lyme d) B. andersonii - Lyme e) B. garinii – Lyme strain in Europe 4 What is TBRF? • Has been defined by clinical presentation • Has been defined by tick vector • Has been defined by genetics • Has been defined by serotype BUT • Each of these has exceptions and limitations! 5 Clinical Presentation of Classic TBRF • “Recurring febrile episodes that last ~3 days and are separated by afebrile periods of ~7 days duration.” • “Each febrile episode involves a “crisis.” During the “chill phase” of the crisis, patients develop very high fever (up to 106.7°F) and may become delirious, agitated, tachycardic and tachypneic. -

Tick-Borne Disease Working Group 2020 Report to Congress
2nd Report Supported by the U.S. Department of Health and Human Services • Office of the Assistant Secretary for Health Tick-Borne Disease Working Group 2020 Report to Congress Information and opinions in this report do not necessarily reflect the opinions of each member of the Working Group, the U.S. Department of Health and Human Services, or any other component of the Federal government. Table of Contents Executive Summary . .1 Chapter 4: Clinical Manifestations, Appendices . 114 Diagnosis, and Diagnostics . 28 Chapter 1: Background . 4 Appendix A. Tick-Borne Disease Congressional Action ................. 8 Chapter 5: Causes, Pathogenesis, Working Group .....................114 and Pathophysiology . 44 The Tick-Borne Disease Working Group . 8 Appendix B. Tick-Borne Disease Working Chapter 6: Treatment . 51 Group Subcommittees ...............117 Second Report: Focus and Structure . 8 Chapter 7: Clinician and Public Appendix C. Acronyms and Abbreviations 126 Chapter 2: Methods of the Education, Patient Access Working Group . .10 to Care . 59 Appendix D. 21st Century Cures Act ...128 Topic Development Briefs ............ 10 Chapter 8: Epidemiology and Appendix E. Working Group Charter. .131 Surveillance . 84 Subcommittees ..................... 10 Chapter 9: Federal Inventory . 93 Appendix F. Federal Inventory Survey . 136 Federal Inventory ....................11 Chapter 10: Public Input . 98 Appendix G. References .............149 Minority Responses ................. 13 Chapter 11: Looking Forward . .103 Chapter 3: Tick Biology, Conclusion . 112 Ecology, and Control . .14 Contributions U.S. Department of Health and Human Services James J. Berger, MS, MT(ASCP), SBB B. Kaye Hayes, MPA Working Group Members David Hughes Walker, MD (Co-Chair) Adalbeto Pérez de León, DVM, MS, PhD Leigh Ann Soltysiak, MS (Co-Chair) Kevin R. -
Bacteria Clostridia Bacilli Eukaryota CFB Group
AM935842.1.1361 uncultured Burkholderiales bacterium Class Betaproteobacteria AY283260.1.1552 Alcaligenes sp. PCNB−2 Class Betaproteobacteria AM934953.1.1374 uncultured Burkholderiales bacterium Class Betaproteobacteria AJ581593.1.1460 uncultured betaAM936569.1.1351 proteobacterium uncultured Class Betaproteobacteria Derxia sp. Class Betaproteobacteria AJ581621.1.1418 uncultured beta proteobacterium Class Betaproteobacteria DQ248272.1.1498 uncultured soil bacterium soil uncultured DQ248272.1.1498 DQ248235.1.1498 uncultured soil bacterium RS49 DQ248270.1.1496 uncultured soil bacterium DQ256489.1.1211 Variovorax paradoxus Class Betaproteobacteria Class paradoxus Variovorax DQ256489.1.1211 AF523053.1.1486 uncultured Comamonadaceae bacterium Class Betaproteobacteria AY706442.1.1396 uncultured bacterium uncultured AY706442.1.1396 AJ536763.1.1422 uncultured bacterium CS000359.1.1530 Variovorax paradoxus Class Betaproteobacteria Class paradoxus Variovorax CS000359.1.1530 AY168733.1.1411 uncultured bacterium AJ009470.1.1526 uncultured bacterium SJA−62 Class Betaproteobacteria Class SJA−62 bacterium uncultured AJ009470.1.1526 AY212561.1.1433 uncultured bacterium D16212.1.1457 Rhodoferax fermentans Class Betaproteobacteria Class fermentans Rhodoferax D16212.1.1457 AY957894.1.1546 uncultured bacterium AJ581620.1.1452 uncultured beta proteobacterium Class Betaproteobacteria RS76 AY625146.1.1498 uncultured bacterium RS65 DQ316832.1.1269 uncultured beta proteobacterium Class Betaproteobacteria DQ404909.1.1513 uncultured bacterium uncultured DQ404909.1.1513 AB021341.1.1466 bacterium rM6 AJ487020.1.1500 uncultured bacterium uncultured AJ487020.1.1500 RS7 RS86RC AF364862.1.1425 bacterium BA128 Class Betaproteobacteria AY957931.1.1529 uncultured bacterium uncultured AY957931.1.1529 CP000884.723807.725332 Delftia acidovorans SPH−1 Class Betaproteobacteria AY957923.1.1520 uncultured bacterium uncultured AY957923.1.1520 RS18 AY957918.1.1527 uncultured bacterium uncultured AY957918.1.1527 AY945883.1.1500 uncultured bacterium AF526940.1.1489 uncultured Ralstonia sp. -

Syphilis Onset Seizures, a Head CT Reveals an Acute CVA • 85 Yo Woman C/O Shooting Pains Down Her Simon J
• 43 yo woman with RUQ pain is found to have a liver mass on U/S, biopsy of the mass reveals granulomas • 26 yo man presents to the ED with new- Syphilis onset seizures, a Head CT reveals an acute CVA • 85 yo woman c/o shooting pains down her Simon J. Tsiouris, MD, MPH Assistant Professor of Clinical Medicine and Clinical Epidemiology arms and in her face for 2 years duration Division of Infectious Diseases College of Physicians and Surgeons • 36 yo man presents to his PMD with an Columbia University enlarging lymph node in his neck 55 yo man presents to the ER with chest pain radiating to his back, 19 yo man is seen at an STD clinic shortness of breath and is found to have this on Chest CT for a painless ulcer on his penis Aortic aneurysm rupture. Axial postcontrast image through the aortic arch reveals an aortic aneurysm with contrast penetrating the thrombus within the aneurysm (open arrow). Note the high attenuation material within the mediastinal fat (arrowheads), representing blood and indicating the presence of aneurysm rupture. 26 yo man presents to an ophthalmologist with progressive loss of vision in his Left eye, his fundoscopic exam looks like the picture on the left: Mercutio: “… a pox on your houses!” Romeo and Juliet, 1st Quarto, 1597, William Shakespeare Normal MID 15 Famous people who (probably) had syphilis • Ivan the Terrible • Henry VIII •Cortes • Francis I • Charles Baudelaire • Meriwether Lewis • Friedrich Nietzche • Gaetano Donizetti • Toulouse Lautrec • Al Capone Old World disease which always existed and happened •… New NewWorld World agent disease which mutatedwhich was and transmitted created a newto the Old Old World World? disease? to flare up around the time of New World exploration? The Great Pox – Origins of syphilis Syphilis in the 1500s • Pre-Colombian New World skeletal remains have bony lesions consistent with syphilis • T. -

Tick-Borne Relapsing Fever Epidemiology
Tick-borne Relapsing Fever Epidemiology Tick-borne Relapsing Fever (TBRF) occurs in the western United States and is usually linked to sleeping in rustic, rodent-infested cabins in mountainous areas and high elevations1,2,3,4. TBRF is not very common in Arizona, and usually sporadic cases occur, with the exception of two small outbreaks in 2005 and 20141,2,3,4. A. Agent: Tick-borne relapsing fever (TBRF) is most commonly caused by Borrelia hermsii, but can be caused by at least 14 other Borrelia species. These bacteria are gram negative spirochetes (cork-screw shaped) and are visible with light microscopy1,2,3,4. B. Clinical Description: Relapsing fever is a systemic spirochetal disease in which periods of fever lasting 2-7 days alternate with afebrile periods of 4-14 days; the number of relapses varies from 1-10 without treatment1,2,3,4. Febrile periods are often associated with shaking chills, sweats, headache, muscle and joint pain, and can be associated with a rash. Photophobia, eye pain, dizziness, dry cough, nausea, vomiting, or lack of appetite can also occur. Symptoms can be more severe without treatment1,2,3,4. Optimal management of TBRF requires both prompt diagnosis and careful observation during the initial phases of treatment1,2,3,4. With appropriate treatment the mortality rate is very low. The mortality rate without treatment is estimated at 5-10%1,2,3,4. TBRF contracted during pregnancy can cause spontaneous abortion, premature birth, and neonatal death1,2,3,4. In general, pregnant women have higher spirochete loads and more severe symptoms than non- pregnant women. -

Isolation of Francisella Tularensis from Skin Ulcer After a Tick Bite, Austria, 2020
microorganisms Case Report Isolation of Francisella tularensis from Skin Ulcer after a Tick Bite, Austria, 2020 Mateusz Markowicz 1,*, Anna-Margarita Schötta 1 , Freya Penatzer 2, Christoph Matscheko 2, Gerold Stanek 1, Hannes Stockinger 1 and Josef Riedler 2 1 Center for Pathophysiology, Infectiology and Immunology, Institute for Hygiene and Applied Immunology, Medical University of Vienna, Kinderspitalgasse 15, A-1090 Vienna, Austria; [email protected] (A.-M.S.); [email protected] (G.S.); [email protected] (H.S.) 2 Kardinal Schwarzenberg Klinikum, Kardinal Schwarzenbergplatz 1, A-5620 Schwarzach, Austria; [email protected] (F.P.); [email protected] (C.M.); [email protected] (J.R.) * Correspondence: [email protected]; Tel.: +43-1-40160-33023 Abstract: Ulceroglandular tularemia is caused by the transmission of Francisella tularensis by arthro- pods to a human host. We report a case of tick-borne tularemia in Austria which was followed by an abscess formation in a lymph node, making drainage necessary. F. tularensis subsp. holarctica was identified by PCR and multilocus sequence typing. Keywords: tularemia; Francisella tularensis; tick; multi locus sequence typing Depending on the transmission route of Francisella tularensis, tularemia can present Citation: Markowicz, M.; Schötta, as a local infection or a systemic disease [1]. Transmission of the pathogen takes place A.-M.; Penatzer, F.; Matscheko, C.; by contact with infected animals, by bites of arthropods or through contaminated water Stanek, G.; Stockinger, H.; Riedler, J. and soil. Hares and wild rabbits are the main reservoirs of the pathogen in Austria [2]. -

Emerging Bartonellosis Christoph Dehio & Anna Sander
Emerging bartonellosis Christoph Dehio & Anna Sander Bartonellae are arthropod-borne pathogens of they cause a long-lasting infection within the red blood Ggrowing medical importance. Until the early cells (intraerythrocytic bacteraemia). Blood-sucking 1990s, only two species of this bacterial genus, arthropod vectors transmit the bacteria from this reservoir B. bacilliformis and B. quintana, were recognized as caus- to new hosts. Incidental infection of non-reservoir hosts ing disease in humans. In addition to re-emergence of the (e.g. humans by the zoonotic species) may cause disease, human-specific B. quintana, a number of zoonotic but does not result in intraerythrocytic infection. Bartonella species have now been recognized as causative agents for a broadening spectrum of diseases that can be Natural history and epidemiology transmitted to humans from their animal hosts. Most Humans are the only known reservoir for two Bartonella prominently, B. henselae is an important zoonotic species, B. bacilliformis and B. quintana. pathogen that is frequently passed from its feline B. quintana was a leading cause of infectious morbidity reservoir to humans. among soldiers during World War I, and recurred on the Bacteria of the genus Bartonella are Gram-negative, East European front in World War II. The disease, pleomorphic, fastidious bacilli that belong to the α-2 Trench fever, is rarely fatal and is characterized by an subclass of Proteobacteria. All Bartonella species appear intraerythrocytic bacteraemia with recurrent, cycling to have a specific mammalian species as a host, in which fever. It is transmitted among humans by the human body louse Pediculus humanus. Although almost forgotten Table 1.