The Case of Mr. Powers' Prostate Cancer Recurrence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Quality of Life Outcomes After Brachytherapy for Early Prostate Cancer
Prostate Cancer and Prostatic Diseases (1999) 2 Suppl 3, S19±S20 ß 1999 Stockton Press All rights reserved 1365±7852/99 $15.00 http://www.stockton-press.co.uk/pcan Quality of life outcomes after brachytherapy for early prostate cancer MS Litwin1, JM Brandeis1, CM Burnison1 and E Reiter1 1UCLA Departments of Urology, Health Services, and Radiation Oncology, UCLA, California, USA Despite the absence of empirical evidence, there is a XRT. Sildena®l appeared to have little effect in the radical popular perception that brachytherapy results in less prostatectomy patients. However, brachytherapy patients impairment of health-related quality of life. This study not receiving hormonal ablation or XRT who took silde- compared general and disease-speci®c health-related na®l had better sexual function and bother scores than quality of life in men who had undergone either brachy- those patients who did not. therapy (with and without pre-treatment XRT) or radical prostatectomy, and in healthy age-matched controls. Method Conclusion We surveyed all patients with clinical T2 or less prostate General health-related quality of life did not differ greatly cancer who had undergone interstitial seed brachyther- between the three groups, but there were variations in apy at UCLA during the previous 3±17 months. Each was disease-speci®c (urinary, bowel and sexual) health-related paired with two randomly selected, temporally matched quality of life. Radical prostatectomy patients had the radical prostatectomy patients. Healthy, age-matched worst urinary function (leakage), but brachytherapy controls were drawn from the literature. Surgery and patients were also signi®cantly worse than the controls. -

Prostate Biopsy in the Staging of Prostate Cancer
Prostate Cancer and Prostatic Diseases (1997) 1, 54±58 ß 1997 Stockton Press All rights reserved 1365±7852/97 $12.00 Review Prostate Biopsy in the staging of prostate cancer L Salomon, M Colombel, J-J Patard, D Gasman, D Chopin & C-C Abbou Service d'Urologie, CHU, Henri Mondor, CreÂteil, France The use of prostate biopsies was developed in parallel with progress in our knowledge of prostate cancer and the use of prostate-speci®c antigen (PSA). Prostate biopsies were initially indicated for the diagnosis of cancer, by the perineal approach under general anesthesia. Nowadays prostate biopsies are not only for diagnostic purposes but also to determine the prognosis, particularly before radical prostatectomy. They are performed in patients with elevated PSA levels, by the endorectal approach, sometimes under local anesthesia.(1±3) The gold standard is the sextant biopsy technique described by Hodge4,5, which is best to diagnose prostate cancer, particularly in case of T1c disease (patients with serum PSA elevation).6±13 Patients with a strong suspicion of prostate cancer from a negative series of biopsies can undergo a second series14;15 with transition zone biopsy16,17 or lateral biopsy.18,19 Karakiewicz et al 20 and Uzzo et al 21 proposed that the number of prostate biopsies should depend on prostate volume to improve the positivity rate. After the diagnosis of prostate cancer, initial therapy will depend on several prognostic factors. In the case of radical prostatectomy, the results of sextant biopsy provide a wealth of information.22,23 The aim of this report is to present the information given by prostate biopsy in the staging of prostate cancer. -

Needle Biopsy and Radical Prostatectomy Specimens David J Grignon
Modern Pathology (2018) 31, S96–S109 S96 © 2018 USCAP, Inc All rights reserved 0893-3952/18 $32.00 Prostate cancer reporting and staging: needle biopsy and radical prostatectomy specimens David J Grignon Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, IUH Pathology Laboratory, Indianapolis, IN, USA Prostatic adenocarcinoma remains the most common cancer affecting men. A substantial majority of patients have the diagnosis made on thin needle biopsies, most often in the absence of a palpable abnormality. Treatment choices ranging from surveillance to radical prostatectomy or radiation therapy are largely driven by the pathologic findings in the biopsy specimen. The first part of this review focuses on important morphologic parameters in needle biopsy specimens that are not covered in the accompanying articles. This includes tumor quantification as well as other parameters such a extraprostatic extension, seminal vesicle invasion, perineural invasion, and lymphovascular invasion. For those men who undergo radical prostatectomy, pathologic stage and other parameters are critical in prognostication and in determining the appropriateness of adjuvant therapy. Staging parameters, including extraprostatic extension, seminal vesicle invasion, and lymph node status are discussed here. Surgical margin status is also an important parameter and definitions and reporting of this feature are detailed. Throughout the article the current reporting guidelines published by the College of American Pathologists and the International Collaboration on Cancer Reporting are highlighted. Modern Pathology (2018) 31, S96–S109; doi:10.1038/modpathol.2017.167 The morphologic aspects of prostatic adenocarcinoma hormonal therapy.4,5 For needle biopsy specimens the have a critical role in the management and prognos- data described below are largely based on standard tication of patients with prostatic adenocarcinoma. -

Robot-Assisted Radical Prostatectomy in a Patient with a Preexisting Three-Piece Inflatable Penile Prosthesis
www.kjurology.org DOI:10.4111/kju.2010.51.1.70 Case Report Robot-Assisted Radical Prostatectomy in a Patient with a Preexisting Three-Piece Inflatable Penile Prosthesis Kyung Hwa Choi, Seung Hwan Lee, Won Sug Jung1, Byung Ha Chung Department of Urology, Urological Science Institute, Yonsei University College of Medicine, Seoul, 1National Health Insurance Corporation Ilsan Hospital, Goyang, Korea We report a rare case of robot-assisted laparoscopic radical prostatectomy (RARP) in Article History: a patient with a preexisting penile prosthesis. In this case, we completed RARP without received 27 August, 2009 14 October, 2009 removing the reservoir by using a deflation-inflation technique, and there were no com- accepted plications related to the prosthesis. The patient had a negative surgical margin. The Corresponding Author: preserved three-piece inflatable penile prosthesis continued to function properly in 1 Byung Ha Chung month. Reservoir-preserving RARP is technically feasible and safe. However, it is im- Department of Urology, Yonsei portant to be aware of device-related complications. Long-term studies on the mechan- University Health System, Gangnam Severance Hospital, 712, Eonju-ro, ical survival rate and patient satisfaction should be also performed. Dogok-dong, Gangnam-gu, Seoul Key Words: Robotics, Prostatectomy, Penile prosthesis, Prostatic neoplasms 135-720, Korea TEL: +82-2-2019-3474 FAX: +82-2-3462-8887 E-mail: [email protected] Prostate cancer has been reported to occur most frequently CASE REPORT in men over 40 years of age. In organ-confined cases, radical prostatectomy is the treatment of choice. After the in- 1. Patient troduction of the da VinciⓇ surgical system (Intuitive The patient was a 64-year-old male diagnosed with aci- Surgical, Sunnyvale, USA), robot-assisted laparoscopic nar-type prostate adenocarcinoma with a Gleason score of radical prostatectomy (RARP) has become a mainstay of 6 (3+3) by prostate biopsy. -

Delayed Multiple Port Sites Metastases After Laparoscopic Radical Prostatectomy
CASE REPORT Delayed Multiple Port Sites Metastases After Laparoscopic Radical Prostatectomy Brusabhanu Nayak, MS, MCH, Prem Nath Dogra, MS, MCH, Vaibhav Saxena, MS, MCH, Ashis Saini, MS, MCH Department of Urology, All India Institute of Medical Sciences, New Delhi, India (all authors). ABSTRACT Introduction: Laparoscopic port site metastases are recurrent nodular lesions developing locally in the abdominal wall within the scar tissue of one or more trocar sites. We are reporting an extremely rare case of delayed multiple port site metastases 3 years after laparoscopic radical prostatectomy. In this case, 3 port site metastases appeared 3 years after laparoscopic radical prostatectomy. Case Description: A 65-year-old man was evaluated for lower urinary tract symptoms and found to have raised serum prostate-specific antigen of 9.06 ng/mL. Transrectal ultrasonography-guided biopsy of the prostate revealed an adeno- carcinoma of the prostate (Gleason score 3 ϩ 4 ϭ 7), with 5 of 12 cores positive for tumor. Contrast-enhanced computed tomography showed localized disease with no involvement of seminal vesicle or lymph nodes. The bone scan was normal. He underwent laparoscopic radical prostatectomy for localized carcinoma of the prostate. He developed 3 port site metastases 3 years after surgery. In view of multiple port site metastatic disease, bilateral orchiectomy was done. The patient is doing well after 1 year of follow-up. Conclusion: We report an occurrence of delayed multiple port site metastases after laparoscopic radical prostatectomy. The 3 sites of metastases in our case included the extraction site, the most active instrument site, and the drain placement site. -

Gender Dysphoria Treatment – Commercial Medical Policy
UnitedHealthcare® Commercial Medical Policy Gender Dysphoria Treatment Policy Number: 2021T0580J Effective Date: April 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ....................................................................... 1 • Blepharoplasty, Blepharoptosis and Brow Ptosis Documentation Requirements ...................................................... 3 Repair Definitions ...................................................................................... 4 • Botulinum Toxins A and B Applicable Codes .......................................................................... 5 • Cosmetic and Reconstructive Procedures Description of Services ................................................................. 9 • Gonadotropin Releasing Hormone Analogs Benefit Considerations .................................................................. 9 Clinical Evidence ......................................................................... 10 • Habilitative Services and Outpatient Rehabilitation U.S. Food and Drug Administration ........................................... 15 Therapy References ................................................................................... 15 • Panniculectomy and Body Contouring Procedures Policy History/Revision Information ........................................... 16 • Rhinoplasty and Other Nasal Surgeries Instructions for Use ..................................................................... 17 Community Plan Policy • Gender Dysphoria -

Gender Dysphoria Treatment – Community Plan Medical Policy
UnitedHealthcare® Community Plan Medical Policy Gender Dysphoria Treatment Policy Number: CS145.I Effective Date: March 1, 2021 Instructions for Use Table of Contents Page Related Community Plan Policies Application ..................................................................................... 1 • Blepharoplasty, Blepharoptosis, and Brow Ptosis Coverage Rationale ....................................................................... 1 Repair Definitions ...................................................................................... 3 • Botulinum Toxins A and B Applicable Codes .......................................................................... 4 • Cosmetic and Reconstructive Procedures Description of Services ................................................................. 8 • Gonadotropin Releasing Hormone Analogs Benefit Considerations .................................................................. 9 Clinical Evidence ........................................................................... 9 • Panniculectomy and Body Contouring Procedures U.S. Food and Drug Administration ........................................... 14 • Rhinoplasty and Other Nasal Surgeries References ................................................................................... 14 • Speech Language Pathology Services Policy History/Revision Information ........................................... 16 Commercial Policy Instructions for Use ..................................................................... 16 • Gender Dysphoria Treatment -
Quality of Life After Open Or Robotic Prostatectomy, Cryoablation Or
Quality of Life After Open or Robotic Prostatectomy, Cryoablation or Brachytherapy for Localized Prostate Cancer Malcolm JB, Fabrizio MD, Barone BB, Given RW, Lance RS, Lynch DF, Davis JW, Shaves ME, Schellhammer PF Departments of Urology (JBM, MDF, BBB, RWG, RSL, DFL, JWD, PFS) and Interventional Radiology (MES), The Virginia Prostate Center at Eastern Virginia Medical School, Norfolk, VA J Urol 2010, 183: 1822 – 1829 HIGHLIGHTS • Highest urinary function and bother scores were reported with cryotherapy • Cryoablation post treatment scores exceeded 100% of baseline, presuming reduction in outlet obstruction with subsequent improvement in obstructive and irritative symptoms • Largest prospective, single center study evaluating HRQOL profiles for cryotherapy, ORP, RAP, BT BACKGROUND • Operative treatments for prostate cancer may produce comparable oncological outcomes • Patient reported quality of life outcomes – important measures – vary among options OBJECTIVE • To prospectively compare the health related QOL impact and recovery profiles for four common prostate treatment modalities METHODS • Prospective, longitudinal cohort study of HRQOL outcomes • Evaluated cryoablation, open radical prostatectomy (ORP), robotic assisted laparoscopic radical prostatectomy (RAP) or brachytherapy (BT) • Participants completed a self-administered UCLA-PCI questionnaire - Questionnaires pre treatment and 3, 6, 12, 18, 24, 30 and 36 months post treatment - HRQOL urinary, sexual and bowel function and bother scored using a 100-point scale • Baseline and -

Robotic Surgery for Male Infertility
Robotic Surgery for Male Infertility Annie Darves-Bornoz, MD, Evan Panken, BS, Robert E. Brannigan, MD, Joshua A. Halpern, MD, MS* KEYWORDS Robotic surgical procedures Infertility Male Vasovasostomy Varicocele KEY POINTS Robotic-assisted approaches to male infertility microsurgery have potential practical benefits including reduction of tremor, 3-dimensional visualization, and decreased need for skilled surgical assistance. Several small, retrospective studies have described robotic-assisted vasectomy reversal with com- parable clinical outcomes to the traditional microsurgical approach. Few studies have described application of the robot to varicocelectomy, testicular sperm extrac- tion, and spermatic cord denervation. The use of robotic-assistance for male infertility procedures is evolving, and adoption has been limited. Rigorous studies are needed to evaluate outcomes and cost-effectiveness. INTRODUCTION with intraperitoneal and pelvic surgery. On the other hand, many of the theoretic and practical ad- Up to 15% of couples have infertility, with approx- 1,2 vantages offered by the robotic approach are imately 50% of cases involving a male factor. A highly transferrable to surgery for male infertility: substantial proportion of men with subfertility have surgically treatable and even reversible etiologies, High quality, 3-dimensional visualization is such as a varicocele or vasal obstruction. The essential for any microsurgical procedure. introduction of the operating microscope revolu- Improved surgeon ergonomics are always desir- tionized the field of male infertility, dramatically able, particularly given the surgeon morbidity improving visualization of small, complex associated with microsurgery.3 anatomic structures. The technical precision Filtering of physiologic tremor can improve pre- afforded has improved operative outcomes across cision during technically demanding micro- the board. -
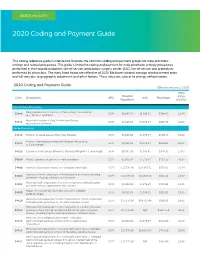
2020 Coding and Payment Guide
MEN’S HEALTH 2020 Coding and Payment Guide This coding reference guide is intended to illustrate the common coding and payment groups for male prosthetic urology and related procedures. This guide is limited to coding and payment for male prosthetic urology procedures performed in the hospital outpatient site-of-service, ambulatory surgery center (ASC) site-of-service and procedures performed by physicians. The rates listed below are reflective of 2020 Medicare national average reimbursement rates and will vary due to geographic adjustment and other factors. These rates are subject to change without notice. 2020 Coding and Payment Guide Effective January 1, 2020 Total Hospital Code Description APC ASC Physicians RVUs Outpatient (Facility) Urinary Sling Procedures Sling operation for correction of male urinary incontinence 53440 5376 $8,067.93 $6.546.11 $784.59 21.74 (e.g., fascia or synthetic) Removal or revision of sling for male incontinence 53442 5375 $4,231.62 $1,976.27 $816.35 22.62 (e.g., fascia or synthetic) Penile Procedures 54110 Excision of penile plaque (Peyronie’s Disease) 5374 $3,018.54 $1,376.97 $650.33 18.02 Excision of penile plaque (Peyronie’s Disease); with graft up 54111 5375 $4,231.62 $1,976.27 $834.03 23.11 to 5 cm in length 54112 Excision of penile plaque (Peyronie’s Disease); with graft > 5 cm in length 5376 $8,067.93 $3,995.65 $976.95 27.07 54360 Plastic operation on penis to correct angulation 5374 $3,018.54 $1,376.97 $751.39 20.82 54400 Insertion of penile prosthesis; non-inflatable (semi-rigid) 5377 $17,573.96 -

ARRO Case: HDR Prostate Brachytherapy
ARRO Case: HDR Prostate Brachytherapy Karna Sura, MD (PGY-5) Faculty Advisor: Sirisha Nandalur, MD Department of Radiation Oncology Beaumont Health Case Presentation • 67 year old male presented with an elevated PSA at 3.55 ng/mL • Found to have no evidence of abnormalities on DRE • Underwent prostate biopsy May 22, 2018 Case presentation continued • Discussed various treatment options including: – Active surveillance – Radical prostatectomy – External beam radiation – HDR prostate brachytherapy as a monotherapy – Other options include LDR brachytherapy and SBRT • Patient wanted to proceed with brachytherapy May 22, 2018 Brief History of Prostate Brachytherapy • 1917 – Barringer inserted radium needles transperineally in the prostate • 1952 – Flocks et al. injected radioactive gold solution into prostate cancer • 1972 – Willet Whitmore described an open implant technique using 125I • 1983 – H. Holm described technique of implanting the prostate with radioactive seeds May 22, 2018 Radiobiology behind prostate brachytherapy • Prostate tumors have small fraction of cycling cells and possibly a low α/β ratio • A meta-analysis of 20+ studies has estimated the α/β ratio between 1-4 Gy with a mean of 2.7 Gy • Thus, hypofractionation might be more effective for prostate cancer Patient history • Urologic history – Prior transurethral or open resection of the prostate or other surgery on the urethra – Prior procedure for BPH – Medication for urinary obstructive symptoms – Erectile function • Prior diagnosis of cancer, especially rectal or bladder -

Robotic-Assisted Laparoscopic Radical Prostatectomy After Aborted Retropubic Radical Prostatectomy
J Robotic Surg (2013) 7:301–304 DOI 10.1007/s11701-012-0377-9 CASE REPORT Robotic-assisted laparoscopic radical prostatectomy after aborted retropubic radical prostatectomy Keith J. Kowalczyk • Andy C. Huang • Stephen B. Williams • Hua-yin Yu • Jim C. Hu Received: 11 March 2012 / Accepted: 31 July 2012 / Published online: 19 August 2012 Ó Springer-Verlag London Ltd 2012 Abstract Robotic-assisted laparoscopic prostatectomy of the endopelvic fascia due to poor visualization, a (RALP) has surged in popularity since US Food and Drug prominent pubic tubercle, and a narrow pelvis. The Administration approval in 2000. Advantages include enhanced visualization and precision of the robotic plat- improved visualization and increased instrument dexterity form allowed adequate exposure of the prostate and within the pelvis. Obesity and narrow pelves have been allowed us to proceed with an uncomplicated prostatecto- associated with increased difficulty during open retropubic my, which was not possible to perform easily via an open radical prostatectomy (RRP), but the robotic platform approach. The bladder was densely adherent to the pubis theoretically allows one to perform a radical prostatectomy and the anterior prostatic contour and apex were difficult to despite these challenges. We present an example of a develop due to a dense fibrotic reaction from the previous RALP performed following an aborted RRP. A 49-year-old endopelvic fascia incision. However, we were able to male with intermediate risk prostate cancer and body mass successfully complete RALP with subtle technical modi- index of 38 kg/m2 presented for RALP after RRP was fications. Estimated blood loss was 160 mL and operating aborted by an experienced open surgeon following incision time was 145 min.