Department of Urology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Part 2-Organ-Sparing Procedures in Testicular and Penile Tumors
International Urology and Nephrology (2019) 51:1699–1708 https://doi.org/10.1007/s11255-019-02182-6 UROLOGY - REVIEW Organ‑sparing procedures in GU cancer: part 2‑organ‑sparing procedures in testicular and penile tumors Mohamed H. Kamel1,3 · Mahmoud I. Khalil1,3 · Ehab Eltahawy1,3 · Rodney Davis1 · Nabil K. Bissada2 Received: 1 May 2019 / Accepted: 23 May 2019 / Published online: 2 July 2019 © Springer Nature B.V. 2019 Abstract Purpose Organ-sparing surgery (OSS) is recommended in selected patients with testicular tumors and penile cancer (PC). The functional and psychological impacts of organ excision for these genital tumors are profound. In this review, we sum- marize the indications, techniques and outcomes of OSS for these two tumors. Methods PubMed® was searched for relevant articles up to December 2018. For Testicular sparing surgery (TSS) search, keywords used were; testicular tumors alone and in combination with “testicular sparing surgery”, “partial orchiectomy” and outcomes. For penile conserving surgery (PCS), keywords used were: penile cancer alone and in combination with “penile conserving surgery”, “partial penectomy” and outcomes. Because of the low quality of available evidence, a narrative rather that systematic review has been performed. Results Indications of TSS are tumors ≤ 2 cm in solitary testis or bilateral tumors and no rete testis invasion. Prerequisites include normal testosterone and luteinizing hormone levels and patient compliance with follow-up. Indications for PCS are distal penile lesions with clinical stage ≤ T1. Adequate penile stump (3 cm) is required after surgery to maintain forward urine stream. Frozen section helps to reduce the risk of recurrence. Local recurrence after PCS is not associated with reduced survival and can be managed with another PCS in selected patients. -

Bris Or Brit Milah (Ritual Circumcision) According to Jewish Law, a Healthy Baby Boy Is Circumcised on the Eighth Day After His Birth
Bris or Brit milah (ritual circumcision) According to Jewish law, a healthy baby boy is circumcised on the eighth day after his birth. The brit milah, the ritual ceremony of removing the foreskin which covers the glans of the penis, is a simple surgical procedure that can take place in the home or synagogue and marks the identification of a baby boy as a Jew. The ceremony is traditionally conducted by a mohel, a highly trained and skilled individual, although a rabbi in conjunction with a physician may perform the brit milah. The brit milah is a joyous occasion for the parents, relatives and friends who celebrate in this momentous event. At the brit milah, it is customary to appoint a kvater (a man) and a kvaterin (a woman), the equivalent of Jewish godparents, whose ritual role is to bring the child into the room for the circumcision. Another honor bestowed on a family member is the sandak, who is most often the baby’s paternal grandfather or great-grandfather. This individual traditionally holds the baby during the circumcision ceremony. The service involves a kiddush (prayer over wine), the circumcision, blessings, a dvar torah (a small teaching of the Torah) and the presentation of the Jewish name selected for the baby. During the brit milah, a chair is set aside for Elijah the prophet. Following the ceremony, a seudat mitzvah (celebratory meal) is available for the guests. Please take note: Formal invitations for a bris are not sent out. Typically, guests are notified by phone or email. The baby’s name is not given before the bris. -

EAU Guidelines on Penile Cancer 2001
European Association of Urology GUIDELINES ON PENILE CANCER* F. Algaba, S. Horenblas, G. Pizzocaro, E. Solsona, T. Windahl TABLE OF CONTENTS PAGE 1. Background 3 2. Classification 3 2.1 Pathology 3 2.2 References 4 3. Risk factors 5 3.1 References 5 4. Diagnosis 6 4.1 Primary lesion 6 4.2 Regional nodes 6 4.3 Distant metastases 7 4.4 Guidelines on the diagnosis of penile cancer 8 4.5 References 8 5. Treatment 9 5.1 Primary lesion 9 5.2 Regional nodes 9 5.3 Guidelines on the treatment of penile carcinoma 11 5.4 Integrated therapy 11 5.5 Distant metastases 11 5.6 Quality life 11 5.7 Technical aspects 12 5.8 Chemotherapy 12 5.9 References 14 6. Follow-up 15 6.1 Why follow-up? 15 6.2 How to follow-up 16 6.3 When to follow-up 16 6.4 Guidelines for follow-up in penile cancer 17 6.5 References 18 7. Abbreviations used in the text 19 2 1. BACKGROUND Penile carcinoma is an uncommon malignant disease with an incidence ranging from 0.1 to 7.9 per 100,000 males. In Europe, the incidence is 0.1–0.9 and in the US, 0.7–0.9 per 100,000 (1). In some areas, such as Asia, Africa and South America, penile carcinoma accounts for as many as 10–20% of male cancers. Phimosis and chronic irritation processes related to poor hygiene are commonly associated with this tumour, whereas neonatal circumcision gives protection against the disease. -

Guidelines on Paediatric Urology S
Guidelines on Paediatric Urology S. Tekgül (Chair), H.S. Dogan, E. Erdem (Guidelines Associate), P. Hoebeke, R. Ko˘cvara, J.M. Nijman (Vice-chair), C. Radmayr, M.S. Silay (Guidelines Associate), R. Stein, S. Undre (Guidelines Associate) European Society for Paediatric Urology © European Association of Urology 2015 TABLE OF CONTENTS PAGE 1. INTRODUCTION 7 1.1 Aim 7 1.2 Publication history 7 2. METHODS 8 3. THE GUIDELINE 8 3A PHIMOSIS 8 3A.1 Epidemiology, aetiology and pathophysiology 8 3A.2 Classification systems 8 3A.3 Diagnostic evaluation 8 3A.4 Disease management 8 3A.5 Follow-up 9 3A.6 Conclusions and recommendations on phimosis 9 3B CRYPTORCHIDISM 9 3B.1 Epidemiology, aetiology and pathophysiology 9 3B.2 Classification systems 9 3B.3 Diagnostic evaluation 10 3B.4 Disease management 10 3B.4.1 Medical therapy 10 3B.4.2 Surgery 10 3B.5 Follow-up 11 3B.6 Recommendations for cryptorchidism 11 3C HYDROCELE 12 3C.1 Epidemiology, aetiology and pathophysiology 12 3C.2 Diagnostic evaluation 12 3C.3 Disease management 12 3C.4 Recommendations for the management of hydrocele 12 3D ACUTE SCROTUM IN CHILDREN 13 3D.1 Epidemiology, aetiology and pathophysiology 13 3D.2 Diagnostic evaluation 13 3D.3 Disease management 14 3D.3.1 Epididymitis 14 3D.3.2 Testicular torsion 14 3D.3.3 Surgical treatment 14 3D.4 Follow-up 14 3D.4.1 Fertility 14 3D.4.2 Subfertility 14 3D.4.3 Androgen levels 15 3D.4.4 Testicular cancer 15 3D.5 Recommendations for the treatment of acute scrotum in children 15 3E HYPOSPADIAS 15 3E.1 Epidemiology, aetiology and pathophysiology -

IS CIRCUMCISION a FRAUD? FRAUD? a IS CIRCUMCISION Peter W
cjp_30-1_42664 Sheet No. 27 Side A 11/12/2020 09:05:36 \\jciprod01\productn\C\CJP\30-1\CJP102.txt unknown Seq: 1 11-NOV-20 14:50 IS CIRCUMCISION A FRAUD? Peter W. Adler, Robert Van Howe, Travis Wisdom & Felix Daase* This Article suggests that non-therapeutic male circumcision or male genital cutting (MGC), the irreversible removal of the foreskin from the penises of healthy boys, is not only unlawful in the United States but also fraudulent. As a German court held in 2012 before its ruling was effectively overturned by a special statute under political pressure, cir- cumcision for religious or non-medical reasons is harmful, violates the child’s rights to bodily integrity and self-determination (which super- sedes competing parental rights), and constitutes criminal assault. MGC also violates the child’s rights under U.S. law, and it constitutes a bat- tery, a tort and a crime, and statutory child abuse. Building upon a 2016 case in the United Kingdom, we make the novel suggestion that when performed by a physician, MGC is a breach of trust or fiduciary duty, and hence constructive fraud, where courts impute fraud even if intent to defraud is absent. We reprise and build upon the argument that it is unlawful and Medicaid fraud for physicians and hospitals to bill Medi- caid for unnecessary genital surgery. Finally, we suggest that MGC con- stitutes intentional fraud by the American Academy of Pediatrics (AAP) and most physicians who perform circumcisions in the United States. They have long portrayed MGC as medicine when it is violence, and as a parental right when males have the right to keep their penile foreskin, and physicians are not allowed to take orders from parents to perform cjp_30-1_42664 Sheet No. -

The Human Foreskin the Foreskin Is Not an Optional Extra for a Man’S Body, Or an Accident
The Human Foreskin The foreskin is not an optional extra for a man’s body, or an accident. It is an integral, functioning, important component of a man’s penis. An eye does not function properly without an eyelid – and nor does a penis without its foreskin. Among other things, the foreskin provides: Protection The foreskin fully covers the glans (head) of the flaccid penis, thereby protecting it from damage and harsh rubbing against abrasive agents (underwear, etc.) and maintaining its sensitivity Sexual Sensitivity The foreskin provides direct sexual pleasure in its own right, as it contains the highest concentration of nerve endings on the penis Lubrication The foreskin, with its unique mucous membrane, permanently lubricates the glans, thus improving sensitivity and aiding smoother intercourse Skin-Gliding During Erection The foreskin facilitates the gliding movement of the skin of the penis up and down the penile shaft and over the glans during erection and sexual activity Varied Sexual Sensation The foreskin facilitates direct stimulation of the glans during sexual activity by its interactive contact with the sensitive glans Immunological Defense The foreskin helps clean and protect the glans via the secretion of anti-bacterial agents What circumcision takes away The foreskin is at the heart of male sexuality. Circumcision almost always results in a diminution of sexual sensitivity; largely because removing the foreskin cuts away the most nerve-rich part of the penis (up to 80% of the penis’s nerve endings reside in the foreskin) [1]. The following anatomy is amputated with circumcision: The Taylor “ridged band” (sometimes called the “frenar band”), the primary erogenous zone of the male body. -
Thromboprophylaxis in Urological Surgery
EAU Guidelines on Thromboprophylaxis in Urological Surgery K.A.O. Tikkinen (Chair), R. Cartwright, M.K. Gould, R. Naspro, G. Novara, P.M. Sandset, P. D . Violette, G.H. Guyatt © European Association of Urology 2018 TABLE OF CONTENTS PAGE 1. INTRODUCTION 3 1.1 Aims and objectives 3 1.2 Panel composition 3 1.3 Available publications 3 1.4 Publication history 3 2. METHODS 3 2.1 Guideline methodology 3 3. GUIDELINE 4 3.1 Thromboprophylaxis post-surgery 4 3.1.1 Introduction 4 3.1.2 Outcomes and definitions 4 3.1.3 Timing and duration of thromboprophylaxis 4 3.1.4 Basic principles for recommending (or not recommending) post-surgery thromboprophylaxis 5 3.1.4.1 Effect of prophylaxis on key outcomes 5 3.1.4.2 Baseline risk of key outcomes 5 3.1.4.3 Patient-related risk (and protective) factors 5 3.1.4.4 From evidence to recommendations 6 3.1.5 General statements for all procedure-specific recommendations 7 3.1.6 Recommendations 7 3.2 Peri-operative management of antithrombotic agents in urology 14 3.2.1 Introduction 14 3.2.2 Evidence summary 14 3.2.3 Recommendations 14 4. RESEARCH RECOMMENDATIONS 16 5. REFERENCES 16 6. CONFLICT OF INTEREST 18 7. ACKNOWLEDGEMENTS 18 8. CITATION INFORMATION 18 2 THROMBOPROPHYLAXIS - MARCH 2017 1. INTRODUCTION 1.1 Aims and objectives Due to the hypercoagulable state induced by surgery, serious complications of urological surgery include deep vein thrombosis (DVT) and pulmonary embolism (PE) - together referred to as venous thromboembolism (VTE) - and major bleeding [1-4]. -

Gender Affirming Surgery and Related Procedures State(S): LOB(S): Idaho Montana Oregon Washington Other: Commercial Medicare Medicaid
Gender Affirming Surgery and Related Procedures State(s): LOB(s): Idaho Montana Oregon Washington Other: Commercial Medicare Medicaid Enterprise Policy BACKGROUND The American Psychiatric Association’s Diagnostic and Statistical Manual, 5th Edition (DSM 5) defines criterion A of Gender Dysphoria as “a marked incongruence between one’s experience/expressed gender and assigned gender.” These individuals must meet additional criteria which include persistence over time and clinically significant distress or impairment in social, occupational or other important areas of functioning. Benefits must be verified by reviewing the plan’s contract or plan document (PD). Some PacificSource benefit plans do not include coverage of gender affirming surgery, procedures or other related treatment. Groups may elect to customize these benefits; therefore, benefit determinations are based on specific contract language. CRITERIA The member should be placed into case management by Health Services as a way to help the member understand their benefits and required criteria related to gender affirming surgery and treatment, and to assist her/him to navigate the system and promote an optimal outcome. Covered Services and Exclusions – Commercial, Medicaid 1. The following are considered medically necessary gender affirming surgeries. a. Core surgical procedures considered medically necessary for females transitioning to males include: hysterectomy, vaginectomy, salpingo-oophorectomy, metoidioplasty, phalloplasty, urethroplasty, scrotoplasty, perineal electrolysis, and placement of testicular implant and mastectomy including nipple reconstruction. b. Core surgical procedures considered medically necessary for males transitioning to females include: penectomy, orchiectomy, vaginoplasty, clitoroplasty, perineal electrolysis, labiaplasty, and mammoplasty when 12 continuous months of hormonal (estrogen) therapy has failed to result in breast tissue growth of Tanner Stage 5 on the puberty scale or there is any contraindication to, or intolerance of, or patient refusal of hormone therapy. -
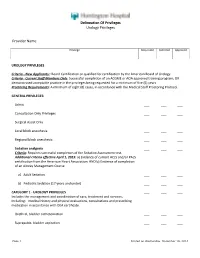
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

A Comprehensive Review of a Rare Subclass of Mucosal Melanoma with Emphasis on Differential Diagnosis and Therapeutic Approaches
cancers Review Urological Melanoma: A Comprehensive Review of a Rare Subclass of Mucosal Melanoma with Emphasis on Differential Diagnosis and Therapeutic Approaches Gerardo Cazzato 1,*,† , Anna Colagrande 1,†, Antonietta Cimmino 1, Concetta Caporusso 1, Pragnell Mary Victoria Candance 1, Senia Maria Rosaria Trabucco 1, Marcello Zingarelli 2, Alfonso Lorusso 2, Maricla Marrone 3 , Alessandra Stellacci 3 , Francesca Arezzo 4, Andrea Marzullo 1, Gabriella Serio 1, Angela Filoni 5, Domenico Bonamonte 5, Paolo Romita 5, Caterina Foti 5, Teresa Lettini 1 , Vera Loizzi 4, Gennaro Cormio 4 , Leonardo Resta 1 , Roberta Rossi 1,‡ and Giuseppe Ingravallo 1,‡ 1 Section of Pathology, Department of Emergency and Organ Transplantation (DETO), University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] (A.C.); [email protected] (A.C.); [email protected] (C.C.); [email protected] (P.M.V.C.); [email protected] (S.M.R.T.); [email protected] (A.M.); [email protected] (G.S.); [email protected] (T.L.); [email protected] (L.R.); [email protected] (R.R.); [email protected] (G.I.) 2 Section of Urology, Deparment of Emergency and Organ Transplantation (DETO), University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] (M.Z.); [email protected] (A.L.) 3 Section of Legal Medicine, Interdisciplinary Department of Medicine, Bari Policlinico Hospital, Citation: Cazzato, G.; Colagrande, University of Bari Aldo Moro, Piazza Giulio Cesare 11, 70124 Bari, Italy; [email protected] (M.M.); A.; Cimmino, A.; Caporusso, C.; [email protected] (A.S.) Candance, P.M.V.; Trabucco, S.M.R.; 4 Section of Ginecology and Obstetrics, Department of Biomedical Sciences and Human Oncology, Zingarelli, M.; Lorusso, A.; Marrone, University of Bari Aldo Moro, Piazza Giulio Cesare 11, 70124 Bari, Italy; [email protected] (F.A.); M.; Stellacci, A.; et al. -

The Circumcision Decision
The Circumcision Decision Circumcision is a surgical procedure in which the skin covering the end of the penis is removed. Scientific studies show a number of medical benefits to circumcision. Parents may also want their son circumcised for religious, social or cultural reasons. Because circumcision is not essential to a child’s health, parents should choose what is best for their child by looking at the benefits, the risks and discussing it with their pediatrician. The following are answers to common questions about circumcision. What Is Circumcision? What Should I Expect For My Son After Circumcision? At birth, boys have skin that covers the end of the penis, called the foreskin. After the circumcision, the tip of the penis Circumcision surgically removes the may seem raw or yellowish. The diaper foreskin, exposing the tip of the penis. should be applied loosely and changed Circumcision is usually performed by a frequently for the first few days. This doctor in the first few days of life. An will help prevent possible infection and infant must be stable and healthy to safely keep the penis from becoming irritated. be circumcised. Petroleum jelly may be used to keep the healing penis from sticking to the Because circumcision may be more risky diaper. Surgical gauze is often applied if done later in life, parents should decide after completion of the circumcision to before or soon after their son is born if prevent bleeding. The gauze will fall off they want it done. on its own in a few days. The penis should be fully healed in about 7-10 days after Is Circumcision Painful? circumcision. -
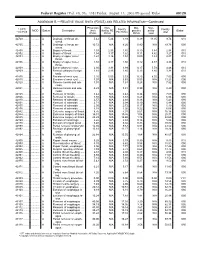
RELATIVE VALUE UNITS (RVUS) and RELATED INFORMATION—Continued
Federal Register / Vol. 68, No. 158 / Friday, August 15, 2003 / Proposed Rules 49129 ADDENDUM B.—RELATIVE VALUE UNITS (RVUS) AND RELATED INFORMATION—Continued Physician Non- Mal- Non- 1 CPT/ Facility Facility 2 MOD Status Description work facility PE practice acility Global HCPCS RVUs RVUs PE RVUs RVUs total total 42720 ....... ........... A Drainage of throat ab- 5.42 5.24 3.93 0.39 11.05 9.74 010 scess. 42725 ....... ........... A Drainage of throat ab- 10.72 N/A 8.26 0.80 N/A 19.78 090 scess. 42800 ....... ........... A Biopsy of throat ................ 1.39 2.35 1.45 0.10 3.84 2.94 010 42802 ....... ........... A Biopsy of throat ................ 1.54 3.17 1.62 0.11 4.82 3.27 010 42804 ....... ........... A Biopsy of upper nose/ 1.24 3.16 1.54 0.09 4.49 2.87 010 throat. 42806 ....... ........... A Biopsy of upper nose/ 1.58 3.17 1.66 0.12 4.87 3.36 010 throat. 42808 ....... ........... A Excise pharynx lesion ...... 2.30 3.31 1.99 0.17 5.78 4.46 010 42809 ....... ........... A Remove pharynx foreign 1.81 2.46 1.40 0.13 4.40 3.34 010 body. 42810 ....... ........... A Excision of neck cyst ........ 3.25 5.05 3.53 0.25 8.55 7.03 090 42815 ....... ........... A Excision of neck cyst ........ 7.07 N/A 5.63 0.53 N/A 13.23 090 42820 ....... ........... A Remove tonsils and ade- 3.91 N/A 3.63 0.28 N/A 7.82 090 noids.