Provider Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wildlife Ophthalmology
Wildlife Ophthalmology DR. HEATHER REID TORONTO WILDLIFE CENTRE TORONTO, ON CANADA Why understand eyes? Wildlife need to have excellent vision to survive in the wild Eye related problems are common in wildlife admitted to rehabilitation centers What we will cover Anatomy of the eye Differences between birds and mammals The eye exam Recognizing common problems Prognosis Treatment options When to see the vet Anatomy Around the Eye: Muscles & nerves Skin Eye lids Nictitating eyelid Conjunctiva & sclera Tear glands & ducts Ossicles (birds) Anatomy Front of the Eye: Cornea Iris Pupil Ciliary body Anterior Chamber Aqueous humor Anatomy Back of the Eye: Lens Retina Optic nerve Choroid Pecten (birds) Posterior Chamber Vitreous humor Fundus of the Eye Mammal Eye Bird Eye The Avian Eye - Differences Small eye size in most birds and small pupil size makes it hard to examine Can control the size of their pupil Lower eyelid more developed The nictitating membrane spreads the tears allowing birds to blink less Moves horizontally across eye The Avian Eye - Differences Eyes are not as protected by skull Less muscles around eye so less eye movement Boney ossicles support the eye Three main eye shapes; flat, globose & tubular The Avian Eye - Differences Four different color receptors compared to the three in mammals means better color detail Can see in the ultraviolet range Higher flicker rate – can detect lights that flicker at more than 100 flashes per second (humans detect at 50) The Avian Eye - Differences In some species the eye -

Part 2-Organ-Sparing Procedures in Testicular and Penile Tumors
International Urology and Nephrology (2019) 51:1699–1708 https://doi.org/10.1007/s11255-019-02182-6 UROLOGY - REVIEW Organ‑sparing procedures in GU cancer: part 2‑organ‑sparing procedures in testicular and penile tumors Mohamed H. Kamel1,3 · Mahmoud I. Khalil1,3 · Ehab Eltahawy1,3 · Rodney Davis1 · Nabil K. Bissada2 Received: 1 May 2019 / Accepted: 23 May 2019 / Published online: 2 July 2019 © Springer Nature B.V. 2019 Abstract Purpose Organ-sparing surgery (OSS) is recommended in selected patients with testicular tumors and penile cancer (PC). The functional and psychological impacts of organ excision for these genital tumors are profound. In this review, we sum- marize the indications, techniques and outcomes of OSS for these two tumors. Methods PubMed® was searched for relevant articles up to December 2018. For Testicular sparing surgery (TSS) search, keywords used were; testicular tumors alone and in combination with “testicular sparing surgery”, “partial orchiectomy” and outcomes. For penile conserving surgery (PCS), keywords used were: penile cancer alone and in combination with “penile conserving surgery”, “partial penectomy” and outcomes. Because of the low quality of available evidence, a narrative rather that systematic review has been performed. Results Indications of TSS are tumors ≤ 2 cm in solitary testis or bilateral tumors and no rete testis invasion. Prerequisites include normal testosterone and luteinizing hormone levels and patient compliance with follow-up. Indications for PCS are distal penile lesions with clinical stage ≤ T1. Adequate penile stump (3 cm) is required after surgery to maintain forward urine stream. Frozen section helps to reduce the risk of recurrence. Local recurrence after PCS is not associated with reduced survival and can be managed with another PCS in selected patients. -

Faculdade De Medicina Veterinária
UNIVERSIDADE DE LISBOA Faculdade de Medicina Veterinária OCULAR BRACHYCEPHALIC SYNDROME Joana Veiga Costa CONSTITUIÇÃO DO JÚRI ORIENTADORA Doutora Maria Luísa Mendes Jorge Doutora Esmeralda Sofia da Costa Doutora Esmeralda Sofia da Costa Delgado Delgado Doutora Lisa Alexandra Pereira Mestrinho CO-ORIENTADORA Doutora Andrea Steinmetz 2019 LISBOA ___________________________________________________________________ UNIVERSIDADE DE LISBOA Faculdade de Medicina Veterinária OCULAR BRACHYCEPHALIC SYNDROME Joana Veiga Costa DISSERTAÇÃO DE MESTRADO INTEGRADO EM MEDICINA VETERINÁRIA CONSTITUIÇÃO DO JÚRI ORIENTADORA Doutora Maria Luísa Mendes Jorge Doutora Esmeralda Sofia da Costa Doutora Esmeralda Sofia da Costa Delgado Delgado Doutora Lisa Alexandra Pereira Mestrinho CO-ORIENTADORA Doutora Andrea Steinmetz 2019 LISBOA ___________________________________________________________________ ACKNOWLEDGEMENT I express my sincere gratitude towards my amazing parents for always supporting me in the pursue of my dreams. I am also immensely thankful to my sister and grandparents, not only for sharing this road with me, but also my whole life. I gratefully acknowledge and offer a special thanks to Professor Esmeralda Delgado for the valuable contribution, guidance, support and kind words throughout the last year. A big thank you to Dr. Susana Azinheira and Dr. Diogo Azinheira for all that I’ve learned during my stayings in your incredible hospital, and the opportunity to put my knowledge at practice. My warmest thanks to my colleagues Maria, Mariana, Pedro, Francisco, Diogo, Catarina, Cláudia, Inês, Sara and Marta for being by my side all these years and for their friendship. May it last forever. I am grateful to Ivo and Rafael for their guidance during the course, specially in the first year, when everything was completely new to me. -

EAU Guidelines on Penile Cancer 2001
European Association of Urology GUIDELINES ON PENILE CANCER* F. Algaba, S. Horenblas, G. Pizzocaro, E. Solsona, T. Windahl TABLE OF CONTENTS PAGE 1. Background 3 2. Classification 3 2.1 Pathology 3 2.2 References 4 3. Risk factors 5 3.1 References 5 4. Diagnosis 6 4.1 Primary lesion 6 4.2 Regional nodes 6 4.3 Distant metastases 7 4.4 Guidelines on the diagnosis of penile cancer 8 4.5 References 8 5. Treatment 9 5.1 Primary lesion 9 5.2 Regional nodes 9 5.3 Guidelines on the treatment of penile carcinoma 11 5.4 Integrated therapy 11 5.5 Distant metastases 11 5.6 Quality life 11 5.7 Technical aspects 12 5.8 Chemotherapy 12 5.9 References 14 6. Follow-up 15 6.1 Why follow-up? 15 6.2 How to follow-up 16 6.3 When to follow-up 16 6.4 Guidelines for follow-up in penile cancer 17 6.5 References 18 7. Abbreviations used in the text 19 2 1. BACKGROUND Penile carcinoma is an uncommon malignant disease with an incidence ranging from 0.1 to 7.9 per 100,000 males. In Europe, the incidence is 0.1–0.9 and in the US, 0.7–0.9 per 100,000 (1). In some areas, such as Asia, Africa and South America, penile carcinoma accounts for as many as 10–20% of male cancers. Phimosis and chronic irritation processes related to poor hygiene are commonly associated with this tumour, whereas neonatal circumcision gives protection against the disease. -

Electroretinography 1 Electroretinography
Electroretinography 1 Electroretinography Electroretinography measures the electrical responses of various cell types in the retina, including the photoreceptors (rods and cones), inner retinal cells (bipolar and amacrine cells), and the ganglion cells. Electrodes are usually placed on the cornea and the skin near the eye, although it is possible to record the ERG from skin electrodes. During a recording, the patient's eyes are exposed to standardized stimuli and the resulting signal is displayed showing the time course of the signal's Maximal response ERG waveform from a dark adapted eye. amplitude (voltage). Signals are very small, and typically are measured in microvolts or nanovolts. The ERG is composed of electrical potentials contributed by different cell types within the retina, and the stimulus conditions (flash or pattern stimulus, whether a background light is present, and the colors of the stimulus and background) can elicit stronger response from certain components. If a flash ERG is performed on a dark-adapted eye, the response is primarily from the rod system and flash ERGs performed on a light adapted eye will reflect the activity of the cone system. To sufficiently bright flashes, the ERG will contain an A patient undergoing an electroretinogram a-wave (initial negative deflection) followed by a b-wave (positive deflection). The leading edge of the a-wave is produced by the photoreceptors, while the remainder of the wave is produced by a mixture of cells including photoreceptors, bipolar, amacrine, and Muller cells or Muller glia.[1] The pattern ERG, evoked by an alternating checkerboard stimulus, primarily reflects activity of retinal ganglion cells. -
Myopia: More Than a Refractive Error − Lasik and Retinal Dystrophies
MYOPIA: MORE THAN A REFRACTIVE ERROR − LASIK AND RETINAL DYSTROPHIES WALRAEDT S.1*, LEROY B.P.1,2*, KESTELYN P.H.1, DE LAEY J.J.1 SUMMARY SAMENVATTING Three patients who had undergone laser in situ Drie patiënten die een correctie van myopie hadden keratomileusis (LASIK) correction for myopia were ondergaan met laser in situ keratomileusis (LASIK) first seen because of suboptimal visual acuity (VA) werden onderzocht omwille van postoperatieve sub- and night blindness and/or photophobia. After a com- optimale visus en nachtblindheid en/of fotofobie. Na prehensive examination including psychophysical uitgebreid onderzoek met inbegrip van psychofysi- and electrophysiological tests, two of the three pa- sche en electrofysiologische testen werd een dia- tients were shown to suffer from a progressive cone- gnose van progressieve kegeltjes-staafjesdystrofie ge- rod dystrophy. The third patient had retinitis pig- steld bij twee patiënten. De derde patiënt leed aan mentosa. These cases illustrate the need for in depth retinitis pigmentosa. Deze gevallen illustreren de preoperative evaluation in myopic patients about to noodzaak van een doorgedreven preoperatief onder- undergo LASIK when signs or problems of night blind- zoek bij myope patiënten die LASIK zullen onder- ness and/or photophobia are present. gaan met klachten van nachtblindheid en fotofobie. KEY WORDS RÉSUMÉ Retinal dystrophy, cone-rod dystrophy, Trois patients sont présentés ayant été examinés pour retinitis pigmentosa, photophobia, night une acuité visuelle sous-optimale et une héméralo- blindness, laser in situ keratomileusis, pie et/ou photophobie, après correction d’une myo- preoperative evaluation pie suivant la technique du laser in situ keratomi- leusis (LASIK). Sur base d’une évaluation élaborée, MOTS-CLÉS y inclus des tests psychophysiques et éléctrophysio- logiques, un diagnostic de dystrophie des cônes et Dystrophie rétinienne, dystrophie de type bâtonnets a été établi chez deux patients. -

Gender Affirming Surgery and Related Procedures State(S): LOB(S): Idaho Montana Oregon Washington Other: Commercial Medicare Medicaid
Gender Affirming Surgery and Related Procedures State(s): LOB(s): Idaho Montana Oregon Washington Other: Commercial Medicare Medicaid Enterprise Policy BACKGROUND The American Psychiatric Association’s Diagnostic and Statistical Manual, 5th Edition (DSM 5) defines criterion A of Gender Dysphoria as “a marked incongruence between one’s experience/expressed gender and assigned gender.” These individuals must meet additional criteria which include persistence over time and clinically significant distress or impairment in social, occupational or other important areas of functioning. Benefits must be verified by reviewing the plan’s contract or plan document (PD). Some PacificSource benefit plans do not include coverage of gender affirming surgery, procedures or other related treatment. Groups may elect to customize these benefits; therefore, benefit determinations are based on specific contract language. CRITERIA The member should be placed into case management by Health Services as a way to help the member understand their benefits and required criteria related to gender affirming surgery and treatment, and to assist her/him to navigate the system and promote an optimal outcome. Covered Services and Exclusions – Commercial, Medicaid 1. The following are considered medically necessary gender affirming surgeries. a. Core surgical procedures considered medically necessary for females transitioning to males include: hysterectomy, vaginectomy, salpingo-oophorectomy, metoidioplasty, phalloplasty, urethroplasty, scrotoplasty, perineal electrolysis, and placement of testicular implant and mastectomy including nipple reconstruction. b. Core surgical procedures considered medically necessary for males transitioning to females include: penectomy, orchiectomy, vaginoplasty, clitoroplasty, perineal electrolysis, labiaplasty, and mammoplasty when 12 continuous months of hormonal (estrogen) therapy has failed to result in breast tissue growth of Tanner Stage 5 on the puberty scale or there is any contraindication to, or intolerance of, or patient refusal of hormone therapy. -
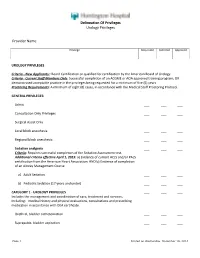
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

A Comprehensive Review of a Rare Subclass of Mucosal Melanoma with Emphasis on Differential Diagnosis and Therapeutic Approaches
cancers Review Urological Melanoma: A Comprehensive Review of a Rare Subclass of Mucosal Melanoma with Emphasis on Differential Diagnosis and Therapeutic Approaches Gerardo Cazzato 1,*,† , Anna Colagrande 1,†, Antonietta Cimmino 1, Concetta Caporusso 1, Pragnell Mary Victoria Candance 1, Senia Maria Rosaria Trabucco 1, Marcello Zingarelli 2, Alfonso Lorusso 2, Maricla Marrone 3 , Alessandra Stellacci 3 , Francesca Arezzo 4, Andrea Marzullo 1, Gabriella Serio 1, Angela Filoni 5, Domenico Bonamonte 5, Paolo Romita 5, Caterina Foti 5, Teresa Lettini 1 , Vera Loizzi 4, Gennaro Cormio 4 , Leonardo Resta 1 , Roberta Rossi 1,‡ and Giuseppe Ingravallo 1,‡ 1 Section of Pathology, Department of Emergency and Organ Transplantation (DETO), University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] (A.C.); [email protected] (A.C.); [email protected] (C.C.); [email protected] (P.M.V.C.); [email protected] (S.M.R.T.); [email protected] (A.M.); [email protected] (G.S.); [email protected] (T.L.); [email protected] (L.R.); [email protected] (R.R.); [email protected] (G.I.) 2 Section of Urology, Deparment of Emergency and Organ Transplantation (DETO), University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] (M.Z.); [email protected] (A.L.) 3 Section of Legal Medicine, Interdisciplinary Department of Medicine, Bari Policlinico Hospital, Citation: Cazzato, G.; Colagrande, University of Bari Aldo Moro, Piazza Giulio Cesare 11, 70124 Bari, Italy; [email protected] (M.M.); A.; Cimmino, A.; Caporusso, C.; [email protected] (A.S.) Candance, P.M.V.; Trabucco, S.M.R.; 4 Section of Ginecology and Obstetrics, Department of Biomedical Sciences and Human Oncology, Zingarelli, M.; Lorusso, A.; Marrone, University of Bari Aldo Moro, Piazza Giulio Cesare 11, 70124 Bari, Italy; [email protected] (F.A.); M.; Stellacci, A.; et al. -

Medical, Legal, Psychosocial, and Ethical Issues of Penile Transplants for Injured Veterans in the United States a Ochasi, N Sopko, G Mamo, V Pepe, a L Burnett, II
The Internet Journal of Law, Healthcare and Ethics ISPUB.COM Volume 11 Number 1 Penile Transplants: To Do or Not To Do: Medical, Legal, Psychosocial, and Ethical Issues of Penile Transplants for Injured Veterans in the United States A Ochasi, N Sopko, G Mamo, V Pepe, A L Burnett, II Citation A Ochasi, N Sopko, G Mamo, V Pepe, A L Burnett, II. Penile Transplants: To Do or Not To Do: Medical, Legal, Psychosocial, and Ethical Issues of Penile Transplants for Injured Veterans in the United States. The Internet Journal of Law, Healthcare and Ethics. 2016 Volume 11 Number 1. DOI: 10.5580/IJLHE.47425 Abstract The genitourinary injuries sustained by soldiers in Iraq and Afghanistan, which make urination, sexual intimacy and fathering a child, more difficult, can cause psychological distress for men, and may even lead to depression. To help ease the burden, Johns Hopkins University has approved a series of 60 experimental penile transplants on wounded veterans with such injuries following the first successful surgery in the US in May of 2016. This article addresses the permissibility of this procedure from the medical, legal, regulatory, sociocultural, religious and ethical perspectives. Medically, since penile transplant fits into the emerging new field of vascularized composite allograft (VCA) there are concerns about the risks for life-long immunosuppression, infection and malignancy. Other concerns include patient’s expectations, donor shortage and lack of public awareness. Legally, the procedure raises issues about the informed consent of donor and recipient, compliance and privacy, as well as need to require a different set of screening procedures and criteria for donation. -

Penile Cancer
Guidelines on Penile Cancer O.W. Hakenberg (chair), E. Compérat, S. Minhas, A. Necchi, C. Protzel, N. Watkin © European Association of Urology 2014 TABLE OF CONTENTS PAGE 1. INTRODUCTION 4 1.1 Publication history 4 1.2 Potential conflict of interest statement 4 2. METHODOLOGY 4 2.1 References 5 3. DEFINITION OF PENILE CANCER 5 4. EPIDEMIOLOGY 5 4.1 References 6 5. RISK FACTORS AND PREVENTION 7 5.1 References 8 6. TNM CLASSIFICATION AND PATHOLOGY 9 6.1 TNM classification 9 6.2 Pathology 10 6.2.1 References 13 7. DIAGNOSIS AND STAGING 15 7.1 Primary lesion 15 7.2 Regional lymph nodes 15 7.2.1 Non-palpable inguinal nodes 15 7.2.2 Palpable inguinal nodes 16 7.3 Distant metastases 16 7.4 Recommendations for the diagnosis and staging of penile cancer 16 7.5 References 16 8. TREATMENT 17 8.1 Treatment of the primary tumour 17 8.1.1 Treatment of superficial non-invasive disease (CIS) 18 8.1.2 Treatment of invasive disease confined to the glans (category Ta/T1a) 18 8.1.2.1 Results of different surgical organ-preserving treatment modalities 18 8.1.2.2 Summary of results of surgical techniques 19 8.1.2.3 Results of radiotherapy for T1 and T2 disease 19 8.1.3 Treatment of invasive disease confined to the corpus spongiosum/glans (Category T2) 20 8.1.4 Treatment of disease invading the corpora cavernosa and/or urethra (category T2/T3) 20 8.1.5 Treatment of locally advanced disease invading adjacent structures (category T3/T4) 20 8.1.6 Local recurrence after organ-conserving surgery 20 8.1.7 Recommendations for stage-dependent local treatment of penile carcinoma. -

6269 Variation of the Response to the Optokinetic Drum Among Various Strain
[Frontiers in Bioscience 13, 6269-6275, May 1, 2008] Variation of the response to the optokinetic drum among various strains of mice Oliver Puk1, Claudia Dalke1, Martin Hrabé de Angelis2, Jochen Graw1 1 GSF-National Research Center for Environment and Health, Institute of Developmental Genetics, D-85764 Neuherberg, Germany, 2GSF-National Research Center for Environment and Health, Institute of Experimental Genetics, D-85764 Neuherberg, Germany TABLE OF CONTENTS 1. Abstract 2. Introduction 3. Materials and methods 3.1. Animals 3.2. Vision test protocol 3.3. Statistical analysis 3.4. Funduscopy 3.5. Electroretinography 3.6. Histology 4. Results 4.1. Head-tracking behavior 4.2. Electroretinography, funduscopy and histology of DBA/2 and BALB/c mice 4.3. Linkage analysis of BALB/c 5. Discussion 6. Acknowledgement 7. References 1. ABSTRACT 2. INTRODUCTION The mouse is currently an established The optokinetic drum has become an appropriate mammalian model for studying hereditary disorders, which tool to examine visual properties of mice. We performed have an effect on eye structure and function. In order to baseline measurements using mice of the inbred strains select and characterize mouse mutants suffering from C3H, C57BL/6, BALB/c, JF1, 129 and DBA/2 at the age of ocular defects, a variety of test systems are well 8-15 weeks. Each individual C57BL/6, 129 and JF1 mouse established, like slit lamp analysis for detecting lens was reliably identified as non-affected in vision by opacities, iris and corneal abnormalities (1-3), funduscopy determining head-tracking responses. C3H mice were used for abnormalities of the retinal fundus, reflecting retinal as negative control because of their inherited retinal degeneration, vascular problems and optic disc alterations degeneration; as expected, they did not respond to the (4), or electroretinography for functional disorders of the moving stripe pattern.