Robotic Surgery for Male Infertility
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reproductive MEDICINE Approximately One in Six Couples Will Experience Difficulty Conceiving
reproductive MEDICINE Approximately one in six couples will experience difficulty conceiving. Our team can help. Welcome to the CMC Center for Reproductive Medicine at CMC Women’s Institute. From the moment you enter our office, you will experience the warm and welcoming atmosphere, the expert medical care and the success that truly makes the CMC Center for Reproductive Medicine one of the best centers in the region. Our physicians have over 50 years combined experience and are the only all board-certified Reproductive Endocrinology and Infertility team near Charlotte. Whether your infertility issue is simple or complex, our caring team will do everything it can to help you achieve your dream of having a baby. “The nurses are your biggest cheerleaders, and the doctors are your rock which helps you through to the next steps. Whenever I see my girls smile and giggle, every shot, test and office visit suddenly becomes a part of the story of how our family was created. There are no words to express my gratitude for the doctors and staff at CMC Center for Reproductive Medicine.” -Melissa Harrison Highly Trained When “high tech” treatment is needed, our physicians provide comprehensive care, seeking out the most effective new technologies with the best trained andrology and embryology specialists in the region. Our services include: Fertility Services • Intrauterine sperm inseminations (IUI) We believe that open communication is one of the most important elements of fertility • In vitro fertilization (IVF) treatment. This is why our entire staff is committed to listening to your concerns and • Donor egg program keeping you fully informed throughout your entire treatment plan. -

Reproductive Endocrinology and Infertility the American Board of Obstetrics and Gynecology, Inc
1 2019 Bulletin for Subspecialty Certification in Reproductive Endocrinology and Infertility The American Board of Obstetrics and Gynecology, Inc. 2915 Vine St., Dallas, TX 75204 First in Women’s Health This Bulletin, issued in January 2018, represents the official statement of the 2019 requirements for subspecialty certification in Reproductive Endocrinology and Infertility 2 Important Information for all Candidates 1. Beginning in calendar year 2020, all physicians who have completed an ABOG or ACGME fellowship in Reproductive Endocrinology and Infertility must achieve ABOG subspecialty certification within 8 years of completion of their training. If certification is not achieved within 8 years, the physician no longer will be eligible to apply for either the qualifying or certifying subspecialty examination unless an additional 6 months of subspecialty training is completed. Physicians who have completed subspecialty training in calendar year 2012 or earlier must be subspecialty certified by 2020 or will be required to complete an additional 6 months of training before regaining eligibility to apply for certification. 2. The preparation of case lists for the Certifying Examination has changed. Candidates will no longer submit paper case lists. Rather, submission will be electronic. Candidates MUST use the electronic reproductive endocrinology and infertility case list forms that will be posted on their ABOG Personal Page in early 2018. 3. Fellows may take up to 8 weeks off each of the fellowship years. The total time off may not exceed 15 weeks over the three years. 4. All fees must be paid by credit card through the ABOG website (www.abog.org) and are payable in US Dollars only. -

Glickman Urological & Kidney Institute
Glickman Urological & Kidney Institute Graphic design and photography were provided by Cleveland Clinic’s Center for Medical Art and Photography. © The Cleveland Clinic Foundation 2017 9500 Euclid Avenue, Cleveland, OH 44195 clevelandclinic.org 2016 Outcomes 17-OUT-426 108374_CCFBCH_17OUT426_acg.indd 1-3 8/31/17 3:02 PM Measuring Outcomes Promotes Quality Improvement Clinical Trials Cleveland Clinic is running more than 2200 clinical trials at any given time for conditions including breast and liver cancer, coronary artery disease, heart failure, epilepsy, Parkinson disease, chronic obstructive pulmonary disease, asthma, high blood pressure, diabetes, depression, and eating disorders. Cancer Clinical Trials is a mobile app that provides information on the more than 200 active clinical trials available to cancer patients at Cleveland Clinic. clevelandclinic.org/cancertrialapp Healthcare Executive Education Cleveland Clinic has programs to share its expertise in operating a successful major medical center. The Executive Visitors’ Program is an intensive, 3-day behind-the-scenes view of the Cleveland Clinic organization for the busy executive. The Samson Global Leadership Academy is a 2-week immersion in challenges of leadership, management, and innovation taught by Cleveland Clinic leaders, administrators, and clinicians. Curriculum includes coaching and a personalized 3-year leadership development plan. clevelandclinic.org/executiveeducation Consult QD Physician Blog A website from Cleveland Clinic for physicians and healthcare professionals. Discover the latest research insights, innovations, treatment trends, and more for all specialties. consultqd.clevelandclinic.org Social Media Cleveland Clinic uses social media to help caregivers everywhere provide better patient care. Millions of people currently like, friend, or link to Cleveland Clinic social media — including leaders in medicine. -

Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) Revised Glossary on ART Terminology, 2009†
Human Reproduction, Vol.24, No.11 pp. 2683–2687, 2009 Advanced Access publication on October 4, 2009 doi:10.1093/humrep/dep343 SIMULTANEOUS PUBLICATION Infertility The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) Revised Glossary on ART Terminology, 2009† F. Zegers-Hochschild1,9, G.D. Adamson2, J. de Mouzon3, O. Ishihara4, R. Mansour5, K. Nygren6, E. Sullivan7, and S. van der Poel8 on behalf of ICMART and WHO 1Unit of Reproductive Medicine, Clinicas las Condes, Santiago, Chile 2Fertility Physicians of Northern California, Palo Alto and San Jose, California, USA 3INSERM U822, Hoˆpital de Biceˆtre, Le Kremlin Biceˆtre Cedex, Paris, France 4Saitama Medical University Hospital, Moroyama, Saitana 350-0495, JAPAN 53 Rd 161 Maadi, Cairo 11431, Egypt 6IVF Unit, Sophiahemmet Hospital, Stockholm, Sweden 7Perinatal and Reproductive Epidemiology and Research Unit, School Women’s and Children’s Health, University of New South Wales, Sydney, Australia 8Department of Reproductive Health and Research, and the Special Program of Research, Development and Research Training in Human Reproduction, World Health Organization, Geneva, Switzerland 9Correspondence address: Unit of Reproductive Medicine, Clinica las Condes, Lo Fontecilla, 441, Santiago, Chile. Fax: 56-2-6108167, E-mail: [email protected] background: Many definitions used in medically assisted reproduction (MAR) vary in different settings, making it difficult to standardize and compare procedures in different countries and regions. With the expansion of infertility interventions worldwide, including lower resource settings, the importance and value of a common nomenclature is critical. The objective is to develop an internationally accepted and continually updated set of definitions, which would be utilized to standardize and harmonize international data collection, and to assist in monitoring the availability, efficacy, and safety of assisted reproductive technology (ART) being practiced worldwide. -

The History of Microsurgery in Urological Practice
Chen-1 The History of Microsurgery in Urological Practice Mang L. Chen1, Gregory M. Buncke2 and Paul J. Turek3 1G.U. Recon, San Francisco, CA, 94114 2The Buncke Clinic, San Francisco, CA 94114 3The Turek Clinic, Beverly Hills, CA 90210 Correspondence to: Mang Chen, MD G.U. Recon 45 Castro St, Suite 111 San Francisco, CA 94114 Tel: 415-481-3980 Email: [email protected] Chen-2 Abstract Operative microscopy spans all surgical disciplines, allowing human dexterity to perform beyond direct visual limitations. Microsurgery started in otolaryngology, became popular in reconstructive microsurgery, and was then adopted in urology. Starting with reproductive tract reconstruction of the vas and epididymis, microsurgery in urology now extends to varicocele repair, sperm retrieval, penile transplantation and free flap phalloplasty. By examining the peer reviewed and lay literature this review discusses the history of microsurgery and its subsequent development as a subspecialty in urology. Keywords: urology, microsurgery, phalloplasty, vasovasostomy, varicocelectomy Chen-3 I. Introduction Microsurgery has been instrumental to surgical advances in many medical fields. Otolaryngology, ophthalmology, gynecology, hand and plastic surgery have all embraced the operating microscope to minimize surgical trauma and scar and to increase patency rates of vessels, nerves and tubes. Urologic adoption of microsurgery began with vasectomy reversals, testis transplants, varicocelectomies and sperm retrieval and has now progressed to free flap phalloplasties and penile transplantation. In this review, we describe the origins of microsurgery, highlight the careers of prominent microsurgeons, and discuss current use applications in urology. II. Birth of Microsurgery 1) Technology The birth of microsurgery followed from an interesting marriage of technology and clinical need. -

Parviz K. Kavoussi, M.D., F.A.C.S. Reproductive Urologist
PARVIZ K. KAVOUSSI, M.D., F.A.C.S. REPRODUCTIVE UROLOGIST www.AustinFertility.com www.AustinVasecomyCenter.com www.WestlakeIVF.com www.AustinMensHealth.com WESTLAKE LOCATION: 300 BEARDSLEY LANE Building B, SUITE 200 AUSTIN, TX 78746 SOUTH AUSTIN LOCATION: 4303 JAMES CASEY, SUITE B AUSTIN, TEXAS 78745 ROUND ROCK LOCATION: 7700 CAT HOLLOW DRIVE, SUITE 106 ROUND ROCK, TEXAS 78681 Phone: (512) 444-1414 EXT 2 Fax: (512) 441-1202 POSTDOCTORAL TRAINING THE UNIVERSITY OF VIRGINIA HEALTH SCIENCES CENTER. Charlottesville, Virginia. Fellowship- Reproductive Urology/Andrology – Male Infertility, Sexual Medicine, and Microsurgery (Vasectomy Reversals/Sperm Retrievals). National Institute of Health funded fellow. July 2008-June 2010. BAYLOR SCOTT & WHITE MEMORIAL HOSPITAL AND HEALTH SCIENCES CENTER. Temple, Texas. Residency- Urology- July 2004-June 2008. General Surgery July 2002-June 2004 EDUCATION THE UNIVERSITY OF TEXAS MEDICAL BRANCH AT GALVESTON. Galveston, Texas. Doctor of Medicine. August 1998-May 2002. BAYLOR UNIVERSITY. Waco, Texas. Bachelor of Arts, degree in Biology. August 1994-May 1998. BOARD CERTIFICATION The American Board of Urology ACADEMIC APPOINTMENTS • Adjunct Assistant Professor. Department of Urology. University of Texas Health Sciences Center at San Antonio. September 2015-present. • Adjunct Assistant Professor. Department of Psychology, Division of Neuroendocrinology and Motivation. University of Texas at Austin. March 2013- present. SPECIALTY CREDENTIALS RAMSES. Credentialed in Robot Assisted Microsurgery in Urology/Robot Assisted Vasectomy Reversals by RAMSES (Robot Assisted Microsurgical and Endoscopic Society). Winter Haven Hospital & University of Florida. April 2011. LABORATORY EXPERIENCE • Basic science laboratory research in the Department of Urology at University of Virginia funded via NIH training grant. July 2008-June 2010. • Non-human primate surgery at the Michael E. -

Minimally Invasive Reproductive Surgery
EPRODU R CT F I O V E Y S Society of T U E I R G C E O O S N Reproductive E S H T ASRM F O 84 UNDED 19 Surgeons FALL 2017 Note from the Editor Message from SRS President, Dr. Ceana Nezhat Dear SRS Members: Dear Colleagues: I am very excited to provide for you It has been an exciting five years serving the membership of the Society of the latest updates from SRS. Reproductive Surgeons. As the President of SRS, I had big shoes to fill and great expectations to match the standards of previous presidents. I could not be more pleased with the accomplishments of the SRS. A successful SRS Fellows Bootcamp was held earlier this year in Houston, My vision and focus as President has been the revitalization of reproductive surgery TX and was led by Dr. Samantha among the members of the American Society for Reproductive Medicine (ASRM), Pfeifer. This issue highlights this by means of furthering educational opportunities and increasing membership wonderful event which received activities. I am pleased to report we have taken great strides in both directions. The very positive feedback from both continuing education for the next generation of reproductive surgeons is of the upmost fellows and faculty. importance. We established an intensive didactic and hands-on surgical boot camp tailored to reproductive endocrinology fellows and junior faculty. Following the success Dr. Camran Nezhat’s team has of our first two SRS-SREI Boot Camps, we are working towards making the 2018 boot contributed a great article on camp even better with plans to increase available spots to meet high demand. -

Delayed Multiple Port Sites Metastases After Laparoscopic Radical Prostatectomy
CASE REPORT Delayed Multiple Port Sites Metastases After Laparoscopic Radical Prostatectomy Brusabhanu Nayak, MS, MCH, Prem Nath Dogra, MS, MCH, Vaibhav Saxena, MS, MCH, Ashis Saini, MS, MCH Department of Urology, All India Institute of Medical Sciences, New Delhi, India (all authors). ABSTRACT Introduction: Laparoscopic port site metastases are recurrent nodular lesions developing locally in the abdominal wall within the scar tissue of one or more trocar sites. We are reporting an extremely rare case of delayed multiple port site metastases 3 years after laparoscopic radical prostatectomy. In this case, 3 port site metastases appeared 3 years after laparoscopic radical prostatectomy. Case Description: A 65-year-old man was evaluated for lower urinary tract symptoms and found to have raised serum prostate-specific antigen of 9.06 ng/mL. Transrectal ultrasonography-guided biopsy of the prostate revealed an adeno- carcinoma of the prostate (Gleason score 3 ϩ 4 ϭ 7), with 5 of 12 cores positive for tumor. Contrast-enhanced computed tomography showed localized disease with no involvement of seminal vesicle or lymph nodes. The bone scan was normal. He underwent laparoscopic radical prostatectomy for localized carcinoma of the prostate. He developed 3 port site metastases 3 years after surgery. In view of multiple port site metastatic disease, bilateral orchiectomy was done. The patient is doing well after 1 year of follow-up. Conclusion: We report an occurrence of delayed multiple port site metastases after laparoscopic radical prostatectomy. The 3 sites of metastases in our case included the extraction site, the most active instrument site, and the drain placement site. -

Gender Dysphoria Treatment – Commercial Medical Policy
UnitedHealthcare® Commercial Medical Policy Gender Dysphoria Treatment Policy Number: 2021T0580J Effective Date: April 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ....................................................................... 1 • Blepharoplasty, Blepharoptosis and Brow Ptosis Documentation Requirements ...................................................... 3 Repair Definitions ...................................................................................... 4 • Botulinum Toxins A and B Applicable Codes .......................................................................... 5 • Cosmetic and Reconstructive Procedures Description of Services ................................................................. 9 • Gonadotropin Releasing Hormone Analogs Benefit Considerations .................................................................. 9 Clinical Evidence ......................................................................... 10 • Habilitative Services and Outpatient Rehabilitation U.S. Food and Drug Administration ........................................... 15 Therapy References ................................................................................... 15 • Panniculectomy and Body Contouring Procedures Policy History/Revision Information ........................................... 16 • Rhinoplasty and Other Nasal Surgeries Instructions for Use ..................................................................... 17 Community Plan Policy • Gender Dysphoria -

Examining Male Infertility
C O Examining Male Infertility N T I N U Susanne Quallich I N G n increasing number of Problems of male infertility can seem like minor issues within the couples seek evaluation larger realm of urology. But many male infertility diagnoses can be and treatment for infer- successfully treated, allowing the couple to conceive naturally or E tility, especially as more with minimal medical assistance. Some patients presenting with male D Acouples delay childbearing in infertility can have more significant disease. Treatments for male U order to establish their careers. A infertility will continue to progress, and as an increasing number of male factor alone is the cause of couples seek infertility services, the need to provide basic informa- C infertility in up to 20% of infer- tion grows as well. A tile couples and a contributing factor in another 30% to 40% of T all couples presenting for infertil- reproductive technologies. influence on overall male develop- I ity evaluations (American It is common to recommend ment and growth. Spermatogenesis O Urological Association [AUA] & an infertility evaluation in couples is driven by testosterone production N American Society for Reproduc- with a history of unprotected in the Leydig cells of the testes. tive Medicine (ASRM), 2001a; intercourse for at least 12 months Under the influence of luteinizing ASRM, 2004). Problems with without a pregnancy and with hormone (LH) and follicle-stimulat- infertility affect approximately 6.1 attempts to time intercourse with ing hormone (FSH), which are million people in the United ovulation, although this length of released from the anterior pituitary, States, or roughly 10% of the time can be shortened as the the testes begin to produce sperm in reproductive-age population. -

Gender Dysphoria Treatment – Community Plan Medical Policy
UnitedHealthcare® Community Plan Medical Policy Gender Dysphoria Treatment Policy Number: CS145.I Effective Date: March 1, 2021 Instructions for Use Table of Contents Page Related Community Plan Policies Application ..................................................................................... 1 • Blepharoplasty, Blepharoptosis, and Brow Ptosis Coverage Rationale ....................................................................... 1 Repair Definitions ...................................................................................... 3 • Botulinum Toxins A and B Applicable Codes .......................................................................... 4 • Cosmetic and Reconstructive Procedures Description of Services ................................................................. 8 • Gonadotropin Releasing Hormone Analogs Benefit Considerations .................................................................. 9 Clinical Evidence ........................................................................... 9 • Panniculectomy and Body Contouring Procedures U.S. Food and Drug Administration ........................................... 14 • Rhinoplasty and Other Nasal Surgeries References ................................................................................... 14 • Speech Language Pathology Services Policy History/Revision Information ........................................... 16 Commercial Policy Instructions for Use ..................................................................... 16 • Gender Dysphoria Treatment -
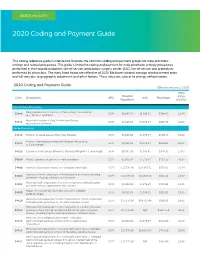
2020 Coding and Payment Guide
MEN’S HEALTH 2020 Coding and Payment Guide This coding reference guide is intended to illustrate the common coding and payment groups for male prosthetic urology and related procedures. This guide is limited to coding and payment for male prosthetic urology procedures performed in the hospital outpatient site-of-service, ambulatory surgery center (ASC) site-of-service and procedures performed by physicians. The rates listed below are reflective of 2020 Medicare national average reimbursement rates and will vary due to geographic adjustment and other factors. These rates are subject to change without notice. 2020 Coding and Payment Guide Effective January 1, 2020 Total Hospital Code Description APC ASC Physicians RVUs Outpatient (Facility) Urinary Sling Procedures Sling operation for correction of male urinary incontinence 53440 5376 $8,067.93 $6.546.11 $784.59 21.74 (e.g., fascia or synthetic) Removal or revision of sling for male incontinence 53442 5375 $4,231.62 $1,976.27 $816.35 22.62 (e.g., fascia or synthetic) Penile Procedures 54110 Excision of penile plaque (Peyronie’s Disease) 5374 $3,018.54 $1,376.97 $650.33 18.02 Excision of penile plaque (Peyronie’s Disease); with graft up 54111 5375 $4,231.62 $1,976.27 $834.03 23.11 to 5 cm in length 54112 Excision of penile plaque (Peyronie’s Disease); with graft > 5 cm in length 5376 $8,067.93 $3,995.65 $976.95 27.07 54360 Plastic operation on penis to correct angulation 5374 $3,018.54 $1,376.97 $751.39 20.82 54400 Insertion of penile prosthesis; non-inflatable (semi-rigid) 5377 $17,573.96