Anesthetic Barbiturates in Refractory Status Epilepticus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chloral Hydrate and Paraldehyde As Drugs of Addiction
Sept., 1932J CHLORAL HYDRATE DRUG HABIT : CHOPRA & SINGH CHOPRA 481 certain parts of the Punjab. This is not the outcome of the use of the drug in the treatment Original Articles of insomnia, but is due to entirely different causes. Until a few years ago in that province potable country-made spirits were allowed to CHLORAL HYDRATE AND PARALDE' be sold to retail dealers in bulk and the vendors HYDE AS DRUGS OF ADDICTION bottled the liquor themselves. Some of these ingenious people conceived the idea of diluting R. N. m.d. By CHOPRA, m.a., (Cantab.) the spirit and adding small quantities of chloral I.M.S. LIEUTENANT-COLONEL, hydrate to make up for the loss in its potency and which would result from dilution. The know- GURBAKHSH SINGH CHOPRA, m.b., b.s. ledge that the drug had hypnotic and narcotic was obtained from the (Drug Addiction Inquiry, Indian Research Fund effects undoubtedly Association) medical profession and compounders work- in It was further learnt that Series No. 15 ing dispensaries. the effects chloral hydrate in many Chloral produced by hydrate and paraldehyde belong to resemble those by alcohol, the of ways produced group drugs known as soporifics or especially when the latter is taken in large The chief use of hypnotics. this class of drugs quantities. When the two articles are taken is in the treatment of one insomnia, of the together they act in a manner synergistic to worst evils of modern times from which man- each other and in this way the effect of either kind can suffer. -

INF.20/Rev.1
INF.20/Rev.1 Economic Commission for Europe Inland Transport Committee 17 January 2017 Working Party on the Transport of Dangerous Goods Joint Meeting of Experts on the Regulations annexed to the European Agreement concerning the International Carriage of Dangerous Goods by Inland Waterways (ADN) (ADN Safety Committee) Thirteenth session Geneva, 23 - 27 January 2017 Item 5 (b) of the provisional agenda Proposals for amendments to the Regulations annexed to ADN: other proposals Autonome Schutzsysteme Mitteilung von EBU, ESO und ERSTU Ausgangslage Zur 29. Sitzung des Sicherheitsausschusses sind zahlreiche Dokumente vorgelegt worden, die die Anforderungen an Explosionsgruppen für nicht-elektrische Geräte betreffen. Weil es aus Zeitgründen nicht möglich war, im ADN 2017 Änderungen vorzunehmen, hat sich der Sicherheitsausschuss darauf geeinigt, die Probleme in der ersten Phase durch multilaterale Abkommen zu regeln. Hierfür ist das Binnenschifffahrtsgewerbe dankbar. Allerdings verlangt die multilaterale Vereinbarung ADN / M 018 von denjenigen Schiffen, deren Zulassungszeugnis nach dem 31. Dezember 2018 erneuert werden muss, schon sehr bald Maßnahmen, die gründlicher Vorbereitung bedürfen. Aus diesem Grunde ist es erforderlich, sich mit einigen vom Schifffahrtsgewerbe aufgeworfenen Fragen rechtzeitig zu beschäftigen. Frage Im Protokoll der 29. Sitzung des Sicherheitsausschusses ADN/WP.15/AC.2/60 ist unter Ziffer 44. festgehalten worden, dass die informelle Arbeitsgruppe „Stoffe“ mittlerweile um die Prüfung verschiedener Sachverhalte gebeten worden ist. Wie weit sind diese Prüfungen gediehen ? Nachfrage zum Protokolls der 29. Sitzung Im Protokoll der 29. Sitzung des Sicherheitsausschusses ADN/WP.15/AC.2/60 ist unter Ziffer 44. – zweiter Unterpunkt - festgehalten worden, dass das Gewerbe die Arbeitsgruppe Stoffe mit einschlägigen Informationen versorgen müsse. Diese Formulierung des Protokolls bedarf der Nachfrage. -

124.210 Schedule IV — Substances Included. 1
1 CONTROLLED SUBSTANCES, §124.210 124.210 Schedule IV — substances included. 1. Schedule IV shall consist of the drugs and other substances, by whatever official name, common or usual name, chemical name, or brand name designated, listed in this section. 2. Narcotic drugs. Unless specifically excepted or unless listed in another schedule, any material, compound, mixture, or preparation containing any of the following narcotic drugs, or their salts calculated as the free anhydrous base or alkaloid, in limited quantities as set forth below: a. Not more than one milligram of difenoxin and not less than twenty-five micrograms of atropine sulfate per dosage unit. b. Dextropropoxyphene (alpha-(+)-4-dimethylamino-1,2-diphenyl-3-methyl-2- propionoxybutane). c. 2-[(dimethylamino)methyl]-1-(3-methoxyphenyl)cyclohexanol, its salts, optical and geometric isomers and salts of these isomers (including tramadol). 3. Depressants. Unless specifically excepted or unless listed in another schedule, any material, compound, mixture, or preparation which contains any quantity of the following substances, including its salts, isomers, and salts of isomers whenever the existence of such salts, isomers, and salts of isomers is possible within the specific chemical designation: a. Alprazolam. b. Barbital. c. Bromazepam. d. Camazepam. e. Carisoprodol. f. Chloral betaine. g. Chloral hydrate. h. Chlordiazepoxide. i. Clobazam. j. Clonazepam. k. Clorazepate. l. Clotiazepam. m. Cloxazolam. n. Delorazepam. o. Diazepam. p. Dichloralphenazone. q. Estazolam. r. Ethchlorvynol. s. Ethinamate. t. Ethyl Loflazepate. u. Fludiazepam. v. Flunitrazepam. w. Flurazepam. x. Halazepam. y. Haloxazolam. z. Ketazolam. aa. Loprazolam. ab. Lorazepam. ac. Lormetazepam. ad. Mebutamate. ae. Medazepam. af. Meprobamate. ag. Methohexital. ah. Methylphenobarbital (mephobarbital). -

Continuous Midazolam Infusion As Treatment of Status Epilepticus
Archives of Disease in Childhood 1997;76:445–448 445 Continuous midazolam infusion as treatment of Arch Dis Child: first published as 10.1136/adc.76.5.445 on 1 May 1997. Downloaded from status epilepticus Roshan Lal Koul, Guru Raj Aithala, Alexander Chacko, Rajendra Joshi, Mussalem Seif Elbualy Abstract Midazolam is a recently developed water In a tertiary referral centre, midazolam soluble benzodiazepine, commonly used as a infusion was tried as treatment for 20 preanaesthetic agent with remarkable anticon- children with status epilepticus over a vulsant action.5 It has been shown to have a period of two years. The mean age of the wide margin of safety and a broad therapeutic children was 4.07 years. Twelve children index. Furthermore, it diVuses rapidly across with refractory status epilepticus had the capillary wall into the central nervous received intravenous or per rectal di- system and can be mixed with saline or glucose azepam and intravenous phenytoin/ solutions to allow its administration as a phenobarbitone or both before midazolam continuous infusion.6 was given (0.15 mg/kg bolus followed by 1–5 µg/kg/min infusion). Eight children required only midazolam to control the Subjects and methods established status epilepticus. The sei- Twenty children suVering from status epilepti- zures were controlled in 19 children. The cus admitted to the paediatric ward from mean time required for complete cessa- November 1993 to November 1995 were tion of seizures was 0.9 hours. The mean included in this study. Eleven were already tak- infusion rate required was 2.0 µg/kg/min. -

State of Illinois Environmental Protection Agency Application for Environmental Laboratory Accreditation
State of Illinois Environmental Protection Agency Application for Environmental Laboratory Accreditation Attachment 6 Program: RCRA Field of Testing: Solid and Chemical Materials, Organic Matrix: Non Solid and Potable Chemical Accredited Water Materials Analyte: Status* Method (SW846): 1,2-Dibromo-3-chloropropane (DBCP) 8011 1,2-Dibromoethane (EDB) 8011 1,4-Dioxane 8015B 1-Butanol (n-Butyl alcohol) 8015B 1-Propanol 8015B 2-Butanone (Methyl ethyl ketone, MEK) 8015B 2-Chloroacrylonitrile 8015B 2-Methyl-1-propanol (Isobutyl alcohol) 8015B 2-Methylpyridine (2-Picoline) 8015B 2-Pentanone 8015B 2-Propanol (Isopropyl alcohol) 8015B 4-Methyl-2-pentanone (Methyl isobutyl ketone, 8015B MIBK) Acetone 8015B Acetonitrile 8015B Acrolein (Propenal) 8015B Acrylonitrile 8015B Allyl alcohol 8015B Crotonaldehyde 8015B Diesel range organics (DRO) 8015B Diethyl ether 8015B Ethanol 8015B Ethyl acetate 8015B Ethylene glycol 8015B Ethylene oxide 8015B Gasoline range organics (GRO) 8015B Hexafluoro-2-methyl-2-propanol 8015B * PI: Pending Initial Accreditation A: Accredited SP: Suspended WD: Accreditation Withdrawn Attachment 6: Page 1 of 62 Program: RCRA Field of Testing: Solid and Chemical Materials, Organic Matrix: Non Solid and Potable Chemical Accredited Water Materials Analyte: Status* Method (SW846): Hexafluoro-2-propanol 8015B Isopropyl benzene ((1-methylethyl) benzene) 8015B Methanol 8015B N-Nitrosodi-n-butylamine (N-Nitrosodibutylamine) 8015B o-Toluidine 8015B Paraldehyde 8015B Propionitrile (Ethyl cyanide) 8015B Pyridine 8015B t-Butyl alcohol 8015B -
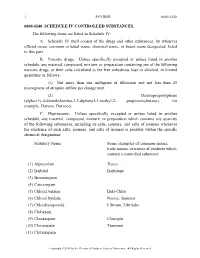
A. Schedule IV Shall Consist Of
1 REVISOR 6800.4240 6800.4240 SCHEDULE IV CONTROLLED SUBSTANCES. The following items are listed in Schedule IV: A. Schedule IV shall consist of the drugs and other substances, by whatever official name, common or usual name, chemical name, or brand name designated, listed in this part. B. Narcotic drugs. Unless specifically excepted or unless listed in another schedule, any material, compound, mixture, or preparation containing any of the following narcotic drugs, or their salts calculated as the free anhydrous base or alkaloid, in limited quantities as follows: (1) Not more than one milligram of difenoxin and not less than 25 micrograms of atropine sulfate per dosage unit. (2) Dextropropoxyphene (alpha-(+)-4-dimethylamino-1,2-diphenyl-3-methyl-2- propionoxybutane), for example, Darvon, Darvocet. C. Depressants. Unless specifically excepted or unless listed in another schedule, any material, compound, mixture, or preparation which contains any quantity of the following substances, including its salts, isomers, and salts of isomers whenever the existence of such salts, isomers, and salts of isomers is possible within the specific chemical designation: Statutory Name Some examples of common names, trade names, or names of products which contain a controlled substance (1) Alprazolam Xanax (2) Barbital Barbitone (3) Bromazepam (4) Camazepam (5) Chloral betaine Beta-Chlor (6) Chloral hydrate Noctec, Somnos (7) Chlordiazepoxide Librium, Libritabs (8) Clobazam (9) Clonazepam Clonopin (10) Clorazepate Tranxene (11) Clotiazepam Copyright ©2013 -

EPI 1: Antiepileptic Medications for Management of Acute Convulsive
[Updated 2015] EPI 1: Antiepileptic medications for management of acute convulsive seizures when no intravenous access is available [Updated 2015] SCOPING QUESTION: In adults with acute convulsive seizures in first-level care or in the community (when no IV access is available), which antiepileptic medications produce benefits and/or harm when compared to comparator? BACKGROUND The treatment for acute convulsive seizures is aimed at earliest cessation of seizures in order to prevent progression to status epilepticus, cardiorespiratory compromise and cerebral damage. Absence of timely intervention may lead to a protracted seizure episode that is more difficult to control with significant subsequent neurological morbidity and mortality (Chen et al., 2014). Rapid and sustained control of seizure status may obviate the need for multiple anti-epileptics and prolonged hospitalization and drastically reduces the chances of adverse outcomes (Chen et al., 2014). It is generally accepted that brief tonic-clonic seizures do not require medication treatment, as they are usually self-limiting. However, seizures of more than five minutes duration, recurrent seizures, delayed recovery of consciousness and a compromised cardio-respiratory system warrant emergency medication treatment. The ideal anti-epileptic medication is one that can be given safely and easily, is rapidly acting, has minimum cardiorespiratory adverse effects, has a long-lasting effect and is inexpensive (Shorvon, 2012). Dispensing antiepileptic medications intravenously is the fastest route of administration; however, achieving peripheral venous access may be difficult in a convulsing patient. This situation is compounded by resource constraints, lack of trained personnel and pre-hospital settings, resulting in the frequent use of non-intravenous routes as the first line for administration of anti-epileptic medications in resource-limited settings (Anderson and Saneto, 2012). -

Pharma Chem 2Nd Hypnotic & Sedative and Tranquilizers
NAME OF Km Uma TEACHER MOB. NO. 6396132349 EMAIL ID [email protected] DESIGNATION Assistant Professor UNIVERSITY NAME Monad University COLLEGE NAME School of Pharmacy Monad University Hapur. STREAM NAME Pharmacy FACULTY NAME Km Uma DEPARTMENT NAME School of Pharmacy nd SUBJECT NAME Pharmaceutical Chemistry 2 COURSE D. Pharm COURSE 2Years DURATION SUB TOPIC NAME Sedative and Hypnotic and tranquilizers CONTENT TYPE Notes Introduction of hypnotic and sedative , Introduction of SEARCH KEY WORD tranquilizers (CONTENTCREATER/TEACHER) Course Content: UNIT CONTENTS Hypnotic and sedative and tranquilizers: detail of UNIT-2 compounds. nd UNIT 2 HYPNOTIC AND SEDATIVE Hypnotics are the drugs which produce sleep and so are used in cases of insomnia (sleeplessness). Sedatives are drugs which reduce excitement and cause sedation. The same drug may act as a hypnotic or sedative or both depending upon the dose. Hypnotic and sedatives depress the central nervous system for producing sleep and sedation. CLASSIFICATION OF SEDATIVE AND HYPNOTIC:- a) Barbiturates Phenobarbitone Butobarbitone Cyclobarbitone b) Aldehyde Paraldehyde c) Benzodiazepines Nitrazepam d) Miscellaneous Methyprylone Glutethimide Triclofos sodium Phenobarbitone Phenobarbitone is a long acting barbiturate. It is a derivative of barbituric acid and its structure has been given below. Physical properties :- Colour:- Colourless crystals or occurs as white crystalline powder Odour:- Odourless Taste:- Bitter taste Solubility:- It is very slightly soluble in water and soluble in ethanol and ether spalingly soluble in chloroform . Chemical properties:- 1) When phenobarbione is dissolved in ethanol and one drop of cobalt chloride solution and one drop of dilute ammonia solution are added, a violet colour is produced. 2) When phenobarbitone and phenobarbitone sodium is dissolved in methanol and a mixture of cobaltous chloride and calcium chloride solutions is added to this solution and then after mixing and shaking , dilute sodium hydroxide solution is added , a violet-blue colour and a precipitate are produced. -
Guideline for the Management of Convulsive Status Epilepticus in Infants and Children
James Lee, MD, Linda Huh, MD, FRCPC, Paul Korn, MD, FRCPC, Kevin Farrell, MD, MBChB Guideline for the management of convulsive status epilepticus in infants and children Children treated more aggressively and those with shorter episodes of status epilepticus have been found less likely to develop neuro- logical deficits. ABSTRACT: Convulsive status epi - onvulsive status epilepticus underlying cause is considered to be lep ticus is a medical emergency accounts for 70% of episodes the most important determinant of out- requiring early and effective treat- Cof status epilepticus (SE) oc - come, and the morbidity appears to be ment. Airway, respiratory, and circu- curring in infants and children.1 Status less in those with febrile and unpro- latory support should be provided epilepticus, whether convulsive or non- voked status epilepticus.6 Studies of immediately. Initial investigations convulsive, is “an epileptic seizure status epilepticus in primates have should then focus on possible meta- that is sufficiently prolonged or re - demonstrated a direct relationship bolic derangements and conditions peated at sufficiently brief intervals between the duration of the seizure that require immediate treatment, so as to produce an unvarying and and the development of permanent such as meningitis. The recommen - enduring epileptic condition.”2 Early brain injury that probably occurs as a ded first-line therapy includes a fast- studies used a definition of continu- result of the depletion of energy sub- acting benzodiazepine followed by a ous seizure activity lasting for 30 min- strate.10 In addition, children treated longer-acting antiepileptic. In cases utes or recurrent seizures without any more aggressively and those with of refractory status epilepticus, fur- intervening recovery of full con- shorter episodes of SE are less likely ther treatment will depend on the sciousness.3 However, most seizures to develop subsequent neurological setting. -
Department of Justice
Vol. 76 Monday, No. 238 December 12, 2011 Part II Department of Justice Drug Enforcement Administration 21 CFR Part 1308 Schedules of Controlled Substances: Placement of Carisoprodol Into Schedule IV; Final Rule VerDate Mar<15>2010 15:56 Dec 09, 2011 Jkt 226001 PO 00000 Frm 00001 Fmt 4717 Sfmt 4717 E:\FR\FM\12DER2.SGM 12DER2 jlentini on DSK4TPTVN1PROD with RULES2 77330 Federal Register / Vol. 76, No. 238 / Monday, December 12, 2011 / Rules and Regulations DEPARTMENT OF JUSTICE (1) [The drug’s] actual or relative that the then-available data did not potential for abuse. support controlling carisoprodol. Id. Drug Enforcement Administration (2) Scientific evidence of its Thereafter, at the direction of the pharmacological effect, if known. National Institute on Drug Abuse 21 CFR Part 1308 (3) The state of current scientific (NIDA) and the College of Problems of knowledge regarding the drug or other Drug Dependence (CPDD), additional [Docket No. DEA–333] substance. pharmacological studies of (4) Its history and current pattern of carisoprodol’s abuse liability were Schedules of Controlled Substances: abuse. conducted. In the meantime, DEA Placement of Carisoprodol Into (5) The scope, duration, and gathered additional new data on actual Schedule IV significance of abuse. abuse and law enforcement encounters (6) What, if any, risk there is to the involving the drug, as well as other AGENCY: Drug Enforcement information, which it sent to HHS on Administration, Department of Justice. public health. (7) Its psychic or physiological November 14, 2005. FDA also acquired ACTION: Final rule. dependence liability. new data from the Drug Abuse Warning Network (DAWN), the National Survey SUMMARY: With the issuance of this final (8) Whether the substance is an rule, the Administrator of the Drug immediate precursor of a substance on Drug Use and Health (NSDUH), Enforcement Administration (DEA) already controlled under this Florida Medical Examiners Commission places the substance carisoprodol, subchapter. -

Mechanism Deposited by the Faculty of Graduate Studies and Research
MECHANISM DEPOSITED BY THE FACULTY OF GRADUATE STUDIES AND RESEARCH X^VA - \^pCA^f^T ra Wy M^QILL UNIVERSITY LIBRARY ACC. NO DATE \ ea^ - A Thesis : ented to ' mlty of Gi Studies h of McGill University L.II. Pidgeon, B.A. - • t of the 3 irenents for the Degz of Ilaster of Soienoe Montreal, G; , 1927. MBQ&aittSM OF CYCLIC ACBTAL FOBM&TION. The importance of the cyclic acetals in relation to the chemistry of the carbohydrates is well recognized and their synthesis 1) has been the subject of much experiment and study. 2) In earlier work dealing with the formation of cyclic acetals by the action of acetylene on polyhydroxy compounds in the presence of a catalyst* an interesting speculation as to the mechanism of this reaction was brought forward. With acetylene and ethylene glycol, for example, it was assumed that the first change involves the addition of one hydroxyl to the unsaturated acetylene linkage with formation of the intermediate hydroxy-ethyl Tinyl ether, (A). HCSGH H-—6 - CB*2- CRg00 —*- CH2=CH - 0 - GH2- CH20H W and that (A), repeating the same general reaction, intra-molecularly rearranges as fast as formed into ethylidene glycol. (B). H2C — CH - 0 - GH2 0 - CH2 C J 1 — CH3 - CH' | N E—0 GH2 0 - CH2 (B) The present investigation deals with the direct synthesis of the Intermediate (A) and the establishment of its constitution. It is shown further that the rearrangement into (B)t as indicated above, takes place in a most striking manner* When pure, freshly prepared, hydroxy-ethyl vinyl ether is brought In contact with a trace of 40$ sulphuric acidtan explosive reaction occurs^and the unsaturated alcohol-ether rearranges itself quantitatively into the saturated cyclic acetal, ethylidene glycol* Both the rate and the energy of this transformation are remarkable* In small amounts, however, and with strong cooling, the violence may be modified somewhat, although even under control the cyclization is complete witon a very short time. -

Jack Deruiter, Principles of Drug Action 2, Fall 2003 1
Jack DeRuiter, Principles of Drug Action 2, Fall 2003 BARBITURATE ANALOGUES AND OTHER SEDATIVE-HYPNOTICS I. Primidone (Mysoline) O CH2CH3 O CH2CH3 R H N N H ON O N O H H H Phenobarbital Primidone ("2-deoxyphenobarbital") Structure, Chemistry and Actions: The 2-deoxy analogue of phenobarbital. Primidone is similar to phenobarbital in its chemical properties, except that it is not acidic (not an imide!). It is metabolized by oxidation to phenobarbital and phenylethylmalonamide (PEMA), both of which have anticonvulsant activity (tonic/clonic and partial seizures) and may express their actions by a mechanism similar to the barbiturates (GABA actions). Thus primidone could be considered to be a prodrug: O CH2CH3 H N O CH2CH3 O N O H O CH2CH3 CYP H N H Phenobarbital H CYP N N O H HO H N O O CH CH H 2 3 Primidone H (2-deoxyphenobarbital) H2N Oxidation Intermediate H2N O PEMA Absorption/Distribution: Primidone is readily absorbed from the GI tract yielding peak serum concentrations occur in 3 hours. Peak serum concentrations of PEMA occur after 7 to 8 hours. Phenobarbital appears in plasma after several days of continuous therapy. Protein binding of primidone and PEMA is negligible; phenobarbital is about 50% protein bound. Monitoring of primidone therapy should include plasma level determinations of primidone and phenobarbital. Metabolism/Execretion: PEMA is the major metabolite and is less active than primidone. Phenobarbital formation ranges from 15% to 25%. The plasma half-life of primidone is 5-15 hours. PEMA and phenobarbital have longer half-lives (10-18 hours and 53-140 hours, respectively) and accumulate with chronic use.