Sedative-Hypnotics: Pharmacology and Use
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RUNNING HEAD: Anomalous Experiences and Hypnotic Suggestibility
Anomalous experiences and hypnotic suggestibility 1 RUNNING HEAD: Anomalous experiences and hypnotic suggestibility Anomalous experiences are more prevalent among highly suggestible individuals who are also highly dissociative David Acunzo1, Etzel Cardeña2, & Devin B. Terhune3* 1 Centre for Mind/Brain Sciences, University of Trento, Rovereto, Italy 2 Department of Psychology, Lund University, Lund, Sweden 3 Department of Psychology, Goldsmiths, University of London, London, UK * Correspondence address: Devin B. Terhune Department of Psychology Goldsmiths, University of London 8 Lewisham Way New Cross, London, UK SE14 6NW [email protected] Word count: 3,186 The data that support the findings of this study are openly available in Open Science Framework at osf.io/cfa3r. Anomalous experiences and hypnotic suggestibility 2 Abstract Introduction: Predictive coding models propose that high hypnotic suggestibility confers a predisposition to hallucinate due to an elevated propensity to weight perceptual beliefs (priors) over sensory evidence. Multiple lines of research corroborate this prediction and demonstrate a link between hypnotic suggestibility and proneness to anomalous perceptual states. However, such effects might be moderated by dissociative tendencies, which seem to account for heterogeneity in high hypnotic suggestibility. We tested the prediction that the prevalence of anomalous experiences would be greater among highly suggestible individuals who are also highly dissociative. Methods: We compared high and low dissociative highly suggestible participants and low suggestible controls on multiple psychometric measures of anomalous experiences. Results: High dissociative highly suggestible participants reliably reported greater anomalous experiences than low dissociative highly suggestible participants and low suggestible controls, who did not significantly differ from each other. Conclusions: These results suggest a greater predisposition to experience anomalous perceptual states among high dissociative highly suggestible individuals. -

Anesthetic Barbiturates in Refractory Status Epilepticus
LE JOURNAL CANADIEN DES SCIENCES NEUROLOGIQUES Anesthetic Barbiturates in Refractory Status Epilepticus G.B. YOUNG, W.T. BLUME, C.F. BOLTON and K.G. WARREN SUMMARY: Two patients with previous INTRODUCTION hours). With intubation and respiratory cerebral damage and seizures and three Generalized status epilepticus is a support an intravenous bolus of 250 mgms. patients with acute inflammatory cerebral medical emergency requiring prompt thiopental was given, followed by 80-120 lesions developed status epilepticus. They mgm/hr. as a continuous infusion for four treatment to prevent cerebral damage days. The seizures stopped promptly. A were unresponsive to standard anticon or death. Rapidly acting anticonvuls vulsants, but anesthetic barbiturates right-sided hemiparesis resolved over the (thiopental and pentobarbital) stopped the ants such as diazepam, phenytoin or next week and he returned home without seizures promptly. paraldehyde are usually effective. additional neurologicaldeficit. Neurology texts, review articles and Case J. A 41 year old woman developed monographs on epilepsy occasionally measles a week prior to the onset of mention anesthesia for resistant cases. delirium and convulsions. Multi-focal RESUME: Deux patients souffrant pre- Anesthetic barbiturates are less com clonic or grand mal seizures continued for alablement de lesion cerebrate et d'epilepsie two days. These were refractory to et trois patients avec lesions cerebrates de monly specified and their effectiveness is not well documented. We present intravenous phenytoin (a loading dose of nature . inflammatoire aigue developpent 1000 mgm intravenously followed by 200 un status epilepticus. Les patients ne five cases successfully treated with mgm every twelve hours), phenobarbital repondent pas a la medication anticon anesthetic barbiturates after conven (200 mgm intravenous bolus and 60 mgm vulsive standard mais I'emploi de barbitur- tional anticonvulsants failed. -

Date Rape and Steroid Panels, Updated Feb 1 2010
DRUG-FACILITATED SEXUAL ASSAULT (aka “DATE RAPE”) AND STEROID PANELS (Effective January 26, 2010) Basic Date Rape Panel Comprehensive Date Rape Panel • GHB (Hair Only) • Ketamine • GHB • Benzodiazepines, including Rohypnol • Benzodiazepines Alprazolam Clonazepam Alprazolam Clonazepam Diazepam Flunitrazepam (Rohypnol) Diazepam Flunitrazepam Lorazepam Oxazepam Lorazepam Oxazepam Temazepam Nitrazepam Temazepam Nitrazepam • Opioids Codeine Hydrocodone Comprehensive Date Rape Panel Meperidine Tramadol (Urine Only) Methadone Fentanyl • GHB • Sedatives/Hypnotics Ketamine Methaqualone • Barbiturates Zolpidem Zopiclone Amobarbital Butalbital Pentobarbital Phenobarbital • Over-The-Counter Drugs Secobarbital Diphenhydramine Dextromethorphan Doxylamine Chlorpheniramine • Benzodiazepines Brompheniramine Promethazine Alprazolam Clonazepam Pheniramine Diazepam Flunitrazepam Lorazepam Oxazepam • Muscle Relaxants Temazepam Nitrazepam Carisoprodol Meprobamate • Opioids Cyclobenzaprine Methocarbamol Codeine Morphine • Hallucinogens (PCP) Hydrocodone Hydromorphone Oxycodone Oxymorphone Meperidine Tramadol ANABOLIC STEROID PANEL Methadone Fentanyl (Urine or Blood) Propoxyphene Buprenorphine Androstenedione Boldenone • Sedatives/Hypnotics Fluoxymesterolone Mesterolone Ketamine Methaqualone 17-a-Methyltestosterone Methenolone Zolpidem Zopiclone Methandrostenolone Nandrolone • Over-The-Counter Drugs Norethandrolone Oxandrolone Diphenhydramine Dextromethorphan Stanozolol Trenbolone Doxylamine Chlorpheniramine Brompheniramine Promethazine Pheniramine For additional steroids, • Muscle Relaxants call for details and pricing Carisoprodol Meprobamate EXPERTOX, INC. Cyclobenzaprine Methocarbamol Blood should only be 1803 CENTER STREET, SUITE A submitted for date rape • Hallucinogens DEER PARK, TX 77536 PCP MDMA panels if within five (5) hours of 281.476.4600 MDA MDEA ingestion. FAX 281.930.8856 Cannabinoids (Carboxy-THC) • WWW.EXPERTOX.COM Turaround Time: Ten (10) Urine must be collected within five (5) days business days from specimen of drug exposure receipt at the lab . -

Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy Using Machine Learning
Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy using Machine Learning Kate Wang et al. Supplemental Table S1. Drugs selected by Pharmacophore-based, ML-based and DL- based search in the FDA-approved drugs database Pharmacophore WEKA TF 1-Palmitoyl-2-oleoyl-sn-glycero-3- 5-O-phosphono-alpha-D- (phospho-rac-(1-glycerol)) ribofuranosyl diphosphate Acarbose Amikacin Acetylcarnitine Acetarsol Arbutamine Acetylcholine Adenosine Aldehydo-N-Acetyl-D- Benserazide Acyclovir Glucosamine Bisoprolol Adefovir dipivoxil Alendronic acid Brivudine Alfentanil Alginic acid Cefamandole Alitretinoin alpha-Arbutin Cefdinir Azithromycin Amikacin Cefixime Balsalazide Amiloride Cefonicid Bethanechol Arbutin Ceforanide Bicalutamide Ascorbic acid calcium salt Cefotetan Calcium glubionate Auranofin Ceftibuten Cangrelor Azacitidine Ceftolozane Capecitabine Benserazide Cerivastatin Carbamoylcholine Besifloxacin Chlortetracycline Carisoprodol beta-L-fructofuranose Cilastatin Chlorobutanol Bictegravir Citicoline Cidofovir Bismuth subgallate Cladribine Clodronic acid Bleomycin Clarithromycin Colistimethate Bortezomib Clindamycin Cyclandelate Bromotheophylline Clofarabine Dexpanthenol Calcium threonate Cromoglicic acid Edoxudine Capecitabine Demeclocycline Elbasvir Capreomycin Diaminopropanol tetraacetic acid Erdosteine Carbidopa Diazolidinylurea Ethchlorvynol Carbocisteine Dibekacin Ethinamate Carboplatin Dinoprostone Famotidine Cefotetan Dipyridamole Fidaxomicin Chlormerodrin Doripenem Flavin adenine dinucleotide -
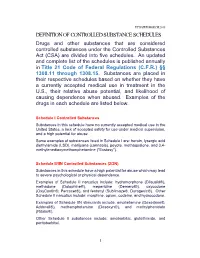
Definition of Controlled Substance Schedules
UPDATED MARCH 2018 DEFINITION OF CONTROLLED SUBSTANCE SCHEDULES Drugs and other substances that are considered controlled substances under the Controlled Substances Act (CSA) are divided into five schedules. An updated and complete list of the schedules is published annually in Title 21 Code of Federal Regulations (C.F.R.) §§ 1308.11 through 1308.15. Substances are placed in their respective schedules based on whether they have a currently accepted medical use in treatment in the U.S., their relative abuse potential, and likelihood of causing dependence when abused. Examples of the drugs in each schedule are listed below. Schedule I Controlled Substances Substances in this schedule have no currently accepted medical use in the United States, a lack of accepted safety for use under medical supervision, and a high potential for abuse. Some examples of substances listed in Schedule I are: heroin, lysergic acid diethylamide (LSD), marijuana (cannabis), peyote, methaqualone, and 3,4- methylenedioxymethamphetamine ("Ecstasy"). Schedule II/IIN Controlled Substances (2/2N) Substances in this schedule have a high potential for abuse which may lead to severe psychological or physical dependence. Examples of Schedule II narcotics include: hydromorphone (Dilaudid®), methadone (Dolophine®), meperidine (Demerol®), oxycodone (OxyContin®, Percocet®), and fentanyl (Sublimaze®, Duragesic®). Other Schedule II narcotics include: morphine, opium, codeine, and hydrocodone. Examples of Schedule IIN stimulants include: amphetamine (Dexedrine®, Adderall®), methamphetamine (Desoxyn®), and methylphenidate (Ritalin®). Other Schedule II substances include: amobarbital, glutethimide, and pentobarbital. 1 Schedule III/IIIN Controlled Substances (3/3N) Substances in this schedule have a potential for abuse less than substances in Schedules I or II and abuse may lead to moderate or low physical dependence or high psychological dependence. -

An FAQ Explaining the Use of Benzodiazepine Sedative Hypnotic Medications in the Elderly
Pharmacy Quality Measures An FAQ Explaining the Use of Benzodiazepine Sedative Hypnotic Medications in the Elderly by Natalie Bari WHERE DOES THIS MEASURE sures feature medications from the the diagnoses (such as insomnia, agi- FIT INTO THE OVERALL MEDI- American Geriatrics Society’s Beers tation, delirium) that the Beers Criteria CARE PART D STAR RATINGS? Criteria for potentially inappropriate state should be avoided. This measure was endorsed by the medication use in older adults. The Pharmacy Quality Alliance (PQA) original HRM measure discussed the WHAT DOES THIS MEASURE in May 2014. But to date, it has not use of non-benzodiazepine sedative ANALYZE? been adopted by the Medicare Part D hypnotics, but it did not include This measure calculates the percent of Star Ratings program. The measure benzodiazepines as they were listed as patients 65 years of age and older who is often described as an extension “avoid only for treatment of insomnia, have received two or more prescription of the PQA measure on the use of agitation or delirium.” The additional fills for any benzodiazepine sedative high-risk medications in the elderly measure was created to address the hypnotic for a cumulative period of (HRM), which was used in the calcu- concern that an unintended conse- more than 90 days. The benzodiaze- lation of the CMS 2015 Star Ratings quence of the HRM measure would be pine sedative hypnotic medications using 2013 claims data. Both mea- increased use of benzodiazepines for are defined to include estazolam, 32 America’s PHARMACIST | January 2015 temazepam, triazolam, flurazepam, them frequently over a prolonged peri- use of the benzodiazepine agents spe- and quazepam. -

Chloral Hydrate and Paraldehyde As Drugs of Addiction
Sept., 1932J CHLORAL HYDRATE DRUG HABIT : CHOPRA & SINGH CHOPRA 481 certain parts of the Punjab. This is not the outcome of the use of the drug in the treatment Original Articles of insomnia, but is due to entirely different causes. Until a few years ago in that province potable country-made spirits were allowed to CHLORAL HYDRATE AND PARALDE' be sold to retail dealers in bulk and the vendors HYDE AS DRUGS OF ADDICTION bottled the liquor themselves. Some of these ingenious people conceived the idea of diluting R. N. m.d. By CHOPRA, m.a., (Cantab.) the spirit and adding small quantities of chloral I.M.S. LIEUTENANT-COLONEL, hydrate to make up for the loss in its potency and which would result from dilution. The know- GURBAKHSH SINGH CHOPRA, m.b., b.s. ledge that the drug had hypnotic and narcotic was obtained from the (Drug Addiction Inquiry, Indian Research Fund effects undoubtedly Association) medical profession and compounders work- in It was further learnt that Series No. 15 ing dispensaries. the effects chloral hydrate in many Chloral produced by hydrate and paraldehyde belong to resemble those by alcohol, the of ways produced group drugs known as soporifics or especially when the latter is taken in large The chief use of hypnotics. this class of drugs quantities. When the two articles are taken is in the treatment of one insomnia, of the together they act in a manner synergistic to worst evils of modern times from which man- each other and in this way the effect of either kind can suffer. -

National Clearinghouse for Drug Abuse Information Selected Reference Series, Series 1, No
DOCUMENT RESOHE ED 090 455 CG 008 832 TITLE National Clearinghouse For Drug Abuse Information Selected Reference Series, Series 1, No. 1. INSTITUTION National Inst. of Mental Health (DHEW), Rockville, Hd. National Clearinghouse for Drug Abuse Information.; Student Association for the Study of Hallucinogens, Biloit, His. PDB DATE Nov 73 NOTE 13p. AVAILABLE FROM National Clearinghouse for Drug Abuse Information, p. 0. Box 1908, Rockville, Maryland 20850 EDRS PRICE MF-10.75 HC-S1.50 PLUS POSTAGE DESCRIPTORS ^Bibliographies; *Drug Abuse; *Drug Education; *Drug Therapy; Government Publications; ^Narcotics ABSTRACT One of a series of bibliographies published by the National Clearinghouse for Drug Abuse Information, this reference focuses on the drug, methagualone. Literature is selected for inclusion on the basis of its currency, significance in the field, and its availability to the public. Materials are directed toward researchers, educators, lawyers, physicians, and members of the public with more than a general need for information. Citations are not annotated. (Author/CJ) SERIES 7, No.l NOVEMBER 1973 Each bibliography of the National Clearinghouse for Drug Abuse 3- Information Selected Reference Series is a representative listing of citations on subjects of topical interest. The selection of o literature is based on its currency, its significance in the field, and its availability in local bookstores or research libraries. The scope of the material is directed toward students writing research papers, special interest groups, such as educators, lawyers and phy sicians, and the general public requiring more resources than public information materials can provide. Each reference series is meant to present an overview of the existing literature, but is not meant to be comprehensive or definitive in scope. -

Drug-Facilitated Sexual Assault Panel, Blood
DRUG-FACILITATED SEXUAL ASSAULT PANEL, BLOOD Blood Specimens (Order Code 70500) Alcohols Analgesics, cont. Anticonvulsants, cont. Antihistamines, cont. Ethanol Phenylbutazone Phenytoin Cyclizine Amphetamines Piroxicam Pregabalin Diphenhydramine Amphetamine Salicylic Acid* Primidone Doxylamine BDB Sulindac* Topiramate Fexofenadine Benzphetamine Tapentadol Zonisamide Guaifenesin Ephedrine Tizanidine Antidepressants Hydroxyzine MDA Tolmetin Amitriptyline Loratadine MDMA Tramadol Amoxapine Oxymetazoline* Mescaline* Anesthetics Bupropion Pyrilamine Methcathinone Benzocaine Citalopram Tetrahydrozoline Methamphetamine Bupivacaine Clomipramine Triprolidine Phentermine Etomidate Desipramine Antipsychotics PMA Ketamine Desmethylclomipramine 9-hydroxyrisperidone Phenylpropanolamine Lidocaine Dosulepin Aripiprazole Pseudoephedrine Mepivacaine Doxepin Buspirone Analgesics Methoxetamine Duloxetine Chlorpromazine Acetaminophen Midazolam Fluoxetine Clozapine Baclofen Norketamine Fluvoxamine Fluphenazine Buprenorphine Pramoxine* Imipramine Haloperidol Carisoprodol Procaine 1,3-chlorophenylpiperazine (mCPP) Mesoridazine Cyclobenzaprine Rocuronium Mianserin* Norclozapine Diclofenac Ropivacaine Mirtazapine Olanzapine Etodolac Antibiotics Nefazodone Perphenazine Fenoprofen Azithromycin* Nordoxepin Pimozide Hydroxychloroquine Chloramphenicol* Norfluoxetine Prochlorperazine Ibuprofen Ciprofloxacin* Norsertraline Quetiapine Ketoprofen Clindamycin* Nortriptyline Risperidone Ketorolac Erythromycin* Norvenlafaxine Thioridazine Meclofenamic Acid* Levofloxacin* Paroxetine -
Uniform Classification Guidelines for Foreign Substances and Recommended Penalties Model Rule
DRUG TESTING STANDARDS AND PRACTICES PROGRAM. Uniform Classification Guidelines for Foreign Substances And Recommended Penalties Model Rule. January, 2018 (V.13.4) Ó ASSOCIATION OF RACING COMMISSIONERS INTERNATIONAL – 2018. Association of Racing Commissioners International 1510 Newtown Pike, Lexington, Kentucky, United States www.arci.com Page 1 of 61 Preamble to the Uniform Classification Guidelines of Foreign Substances The Preamble to the Uniform Classification Guidelines was approved by the RCI Drug Testing and Quality Assurance Program Committee (now the Drug Testing Standards and Practices Program Committee) on August 26, 1991. Minor revisions to the Preamble were made by the Drug Classification subcommittee (now the Veterinary Pharmacologists Subcommittee) on September 3, 1991. "The Uniform Classification Guidelines printed on the following pages are intended to assist stewards, hearing officers and racing commissioners in evaluating the seriousness of alleged violations of medication and prohibited substance rules in racing jurisdictions. Practicing equine veterinarians, state veterinarians, and equine pharmacologists are available and should be consulted to explain the pharmacological effects of the drugs listed in each class prior to any decisions with respect to penalities to be imposed. The ranking of drugs is based on their pharmacology, their ability to influence the outcome of a race, whether or not they have legitimate therapeutic uses in the racing horse, or other evidence that they may be used improperly. These classes of drugs are intended only as guidelines and should be employed only to assist persons adjudicating facts and opinions in understanding the seriousness of the alleged offenses. The facts of each case are always different and there may be mitigating circumstances which should always be considered. -

House Bill No.11 (2019)
LEGISLATURE OF THE STATE OF IDAHO Sixty-fifth Legislature First Regular Session - 2019 IN THE HOUSE OF REPRESENTATIVES HOUSE BILL NO. 11 BY HEALTH AND WELFARE COMMITTEE 1 AN ACT 2 RELATING TO CONTROLLED SUBSTANCES; AMENDING SECTION 37-2705, IDAHO CODE, TO 3 REVISE THE LIST OF SCHEDULE I CONTROLLED SUBSTANCES; AMENDING SECTION 4 37-2709, IDAHO CODE, TO PROVIDE AN EXCLUSION AND TO MAKE A TECHNICAL 5 CORRECTION; AMENDING SECTION 37-2713, IDAHO CODE, TO REVISE THE LIST OF 6 SCHEDULE V DRUGS AND SUBSTANCES; AND DECLARING AN EMERGENCY. 7 Be It Enacted by the Legislature of the State of Idaho: 8 SECTION 1. That Section 37-2705, Idaho Code, be, and the same is hereby 9 amended to read as follows: 10 37-2705. SCHEDULE I. (a) The controlled substances listed in this sec- 11 tion are included in schedule I. 12 (b) Any of the following opiates, including their isomers, esters, 13 ethers, salts, and salts of isomers, esters, and ethers, unless specifically 14 excepted, whenever the existence of these isomers, esters, ethers and salts 15 is possible within the specific chemical designation: 16 (1) Acetyl-alpha-methylfentanyl (N-[1-(1-methyl-2-phenethyl)-4-pip- 17 eridinyl]-N-phenylacetamide); 18 (2) Acetylmethadol; 19 (3) Acetyl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylac- 20 etamide); 21 (4) Allylprodine; 22 (5) Alphacetylmethadol (except levo-alphacetylmethadol also known as 23 levo-alpha-acetylmethadol, levomethadyl acetate or LAAM); 24 (6) Alphameprodine; 25 (7) Alphamethadol; 26 (8) Alpha-methylfentanyl; 27 (9) Alpha-methylthiofentanyl -

Punjab Technical University/Msc. Clinical Research
Punjab Technical University/MSc. Clinical Research Scheme and Syllabus First Semester Teaching Load Course Marks Distribution Exam Course Title Allocation Credit Code (hr.) (hr.) L T P Internal External Total Pharmacology- C R- 101 3 1 - 40 60 100 3 4 101 Clinical CR - 102 3 1 - 40 60 100 3 4 Research-102 CR - 103 Medicine - 103 2 2 - 40 60 100 3 4 CR - 104 Biostatistics -104 2 2 - 40 60 100 3 4 Practical Lab (Part I-IT & Part- CR-105 - - 8 40 60 100 3 4 II Communication and management) 10 06 8 200 300 500 -- 20 Second Semester Teaching Load Course Marks Distribution Exam Course Title Allocation Credit Code (hr.) (hr.) L T P Internal External Total C R- 201 Pharmacology- 3 1 - 40 60 100 3 4 201 CR - 202 Clinical Research- 3 1 - 40 60 100 3 4 202 CR - 203 Medicine - 203 2 2 - 40 60 100 3 4 CR - 204 Biostatistics -204 2 2 - 40 60 100 3 4 CR-205 Practical Lab - - 8 40 60 100 3 4 (Part I-IT & Part- II Communication and management) 10 06 8 200 300 500 -- 20 Page 1 of 27 Punjab Technical University/MSc. Clinical Research Third Semester Teaching Load Exa Course Marks Distribution Course Title Allocation (hr.) m Credit Code L T P Internal External Total (hr.) CR- Pharmacology- 301 3 1 - 40 60 100 3 4 301 CR- Clinical Research-I - 3 1 - 40 60 100 3 4 302 302 CR- Clinical Research-II- 3 1 - 40 60 100 3 4 303 303 CR- Medicine -304 3 1 - 40 60 100 3 4 304 CR- Practical Lab - - 8 40 60 100 3 4 305 (Part I-IT & Part-II Communication and Management) Total 12 4 8 200 300 500 - 20 Fourth Semester Marks Distribution Course Title Dissertation Viva-Voce Total Credits Evaluation Dissertation 100 200 300 12 The thesis/project report shall be presented by the candidate at the end of record academic year.